Endoscopic biopsy is a common procedure performed in the hospital for a variety of benign and malignant lesions of gastrointestinal tract. Endoscopy is incomplete without biopsy and histopathology is the gold standard for the diagnosis of endoscopically detected lesions. This study aims at analysing age-wise spectrum of gastrointestinal biopsies with their endoscopic correlation. A total of 556 endoscopic biopsy specimens from upper and lower gastrointestinal tract were studied retrospectively from January 2014 to October 2019 in the department of pathology, Jawaharlal Nehru Medical College (JNMC) Aligarh Muslim University, Aligarh. Biopsies were retrieved using flexible fibre-optic endoscope and also video endoscope. Out of 556 gastrointestinal endoscopic biopsy samples, maximum numbers of cases were in the adult age group (13-59 yrs) 403 (72%). M:F ratio in paediatric, adult, geriatric population was 1.4:1, 1.5:1, 1.6:1 respectively. Among paediatric population duodenal biopsies were maximum being 29 (44%), most common diagnosis being celiac disease 14 (22%). Among adult population maximum were stomach biopsies 190 (47%), most common being non specific inflammation 105 (26%). Among geriatric population maximum were oesophageal biopsies, most common lesion being squamous cell carcinoma 24 (28%). Endoscopic examination and biopsy is a convenient procedure for accurate objective assessment of patients with gastrointestinal symptoms. Clinical and endoscopic findings along with histopathological correlation help in making an accurate diagnosis.
Gastrointestinal biopsies, Histopathology, Endoscopy, Non-specific inflammation, Celiac disease, Squamous cell carcinoma
Gastrointestinal (GI) tract extends from oesophagus to anus, and is a common site for various pathologies ranging from non-neoplastic lesions to pre-malignant and malignant lesions. Gastrointestinal disorders are most commonly encountered in clinical practice. According to GLOBOCAN 2018, gastric cancer is the 5th most common cancer worldwide and is 3rd most common cause of cancer related deaths [1]. Gastrointestinal cancers are associated with substantial morbidity and mortality. Early diagnosis is thus required to lessen patient suffering and improve disease outcome [2].
Gastrointestinal biopsies are the major bulk specimens received in the surgical pathology section of tertiary hospital. These include endoscopic biopsies from gastric and duodenal mucosa, appendicectomies, colonoscopic biopsies, colectomies, etc. [3]. Endoscopy and colonoscopy are minimally invasive diagnostic procedures which aids in diagnosis and treatment. Endoscopic biopsies play a critical role in detecting dysplasias and early cancers, hence, aids in early management.
Endoscopic biopsies are not just of diagnostic significance, but they are also used to monitor the disease course, also aids in detecting treatment response and its complications. These are considered as the gold standard investigation for diagnosing gastrointestinal lesions [2].
To study age wise distribution of GI lesions in a tertiary healthcare centre of North India, along with their clinical, endoscopic and histopathological correlation.
This was a retrospective study conducted in the department of pathology, Jawaharlal Nehru Medical College (JNMC) Aligarh Muslim University, Aligarh over a period of 5 years from January 2014 to October 2019. A total of 556 endoscopic biopsies from upper and lower GI tract were evaluated during this period. Relevant clinical details were noted as required for diagnostic support. Biopsies were retrieved using flexible fibre-optic endoscope and video endoscope. They were transferred to a bottle containing 10% neutral formalin, processed and embedded. 5micron thick sections were done and routine staining with haematoxylin and eosin was done in all the cases. Special stains such as PAS and Giemsa were applied as and when required.
In this study we propose to analyse the histopathological spectrum of gastrointestinal lesions, received in the Department of Pathology, Jawaharlal Nehru Medical College, AMU, Aligarh. Age and sex distribution of these lesions was studied along with the distribution of benign and malignant lesions with respect to age and site.
The present study comprised 556 endoscopic biopsies received in the department of pathology over a period of 5 years (Table 1).
Table 1: Age wise distribution of gastrointestinal lesions. View Table 1
Out of 556 gastrointestinal endoscopic biopsy samples, maximum numbers of cases were in the adult age group (13-59 yrs) 403 (72%). This was followed by 88 cases (16%) in geriatric population. Endoscopic biopsies in paediatric group are less comparatively (Table 2).
Table 2: Sex distribution of gastrointestinal lesions in each group. View Table 2
There was a clear male preponderance in each age-group, with M:F ratio in paediatric, adult and geriatric population being 1.4:1, 1.5:1 and 1.6:1 respectively (Table 3).
Table 3: Upper and lower GI endoscopic biopsies in different age-groups. View Table 3
The incidence of upper GI endoscopic biopsies was maximum in adults (91%) followed by geriatric population (74%). In our study, maximum numbers of lower gastrointestinal endoscopic biopsies were done in paediatric group (42%) (Table 4).
Table 4: Distribution of benign and malignant lesions in different age-groups. View Table 4
In the present study, among GI lesions diagnosed on endoscopic biopsies benign lesions were more prevalent in all age groups. Among esophageal lesions, malignancies were commonly encountered in adult and geriatric population in comparison to benign lesions. In paediatric group, duodenal biopsies (30 cases out of 65) were most commonly received specimen followed by rectal-biopsies (20 cases). Gastric and duodenal biopsies constituted more than 50% of all GI endoscopic biopsies in adults. While in geriatric group, esophageal biopsies were most common endoscopic biopsy specimen received (32 out of total 88 biopsies). Among the lower GI biopsies, rectal biopsies were most common in all age-groups (Table 5 and Table 6) (Figure 1, Figure 2a, Figure 2b, Figure 3, Figure 4a, Figure 4b, Figure 5a, Figure 5b, Figure 6, Figure 7, Figure 8a, Figure 8b, Figure 9, Figure 10a, Figure 10b and Figure 11).
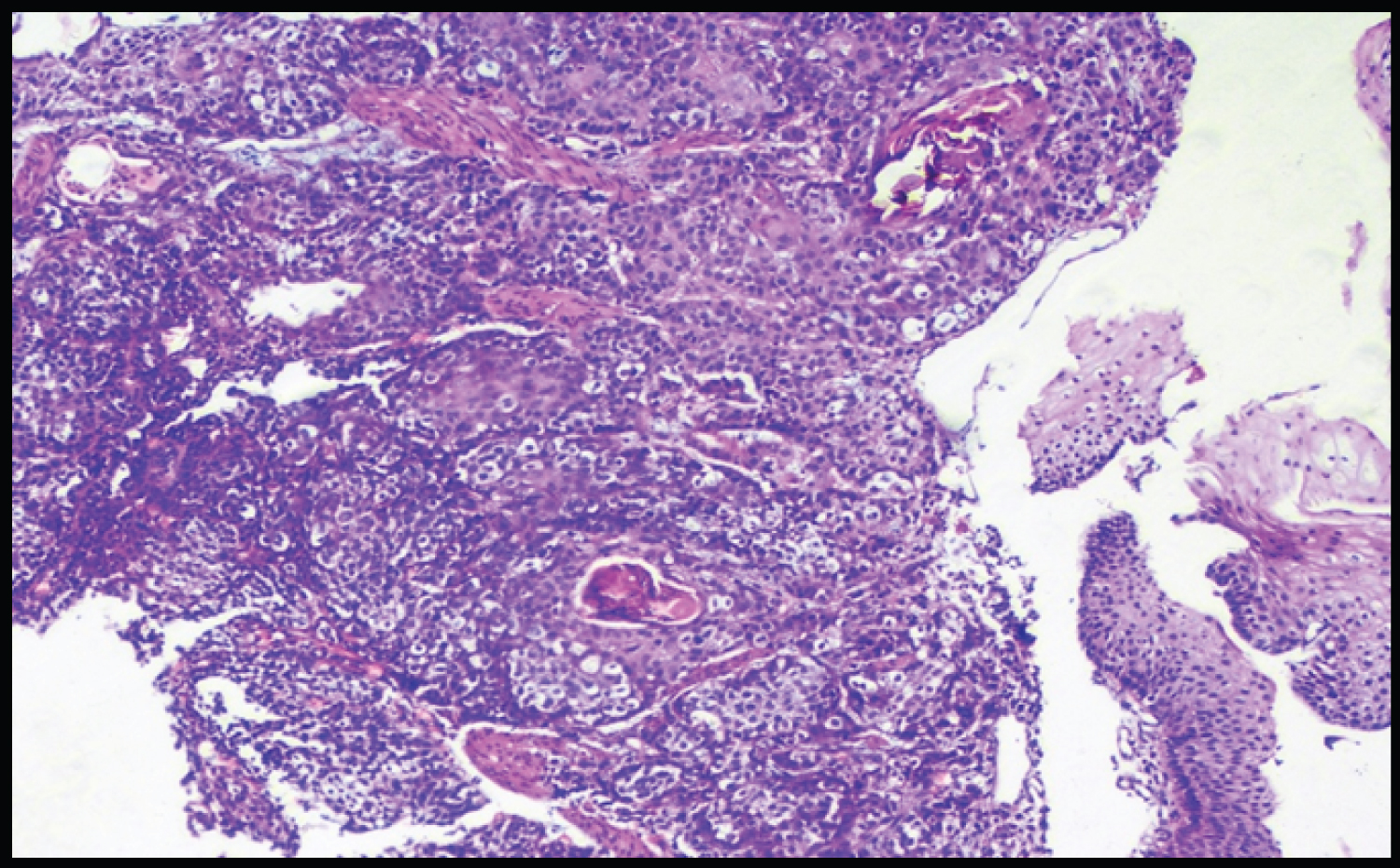 Figure 1: Squamous cell carcinoma esophagus (H&E).
View Figure 1
Figure 1: Squamous cell carcinoma esophagus (H&E).
View Figure 1
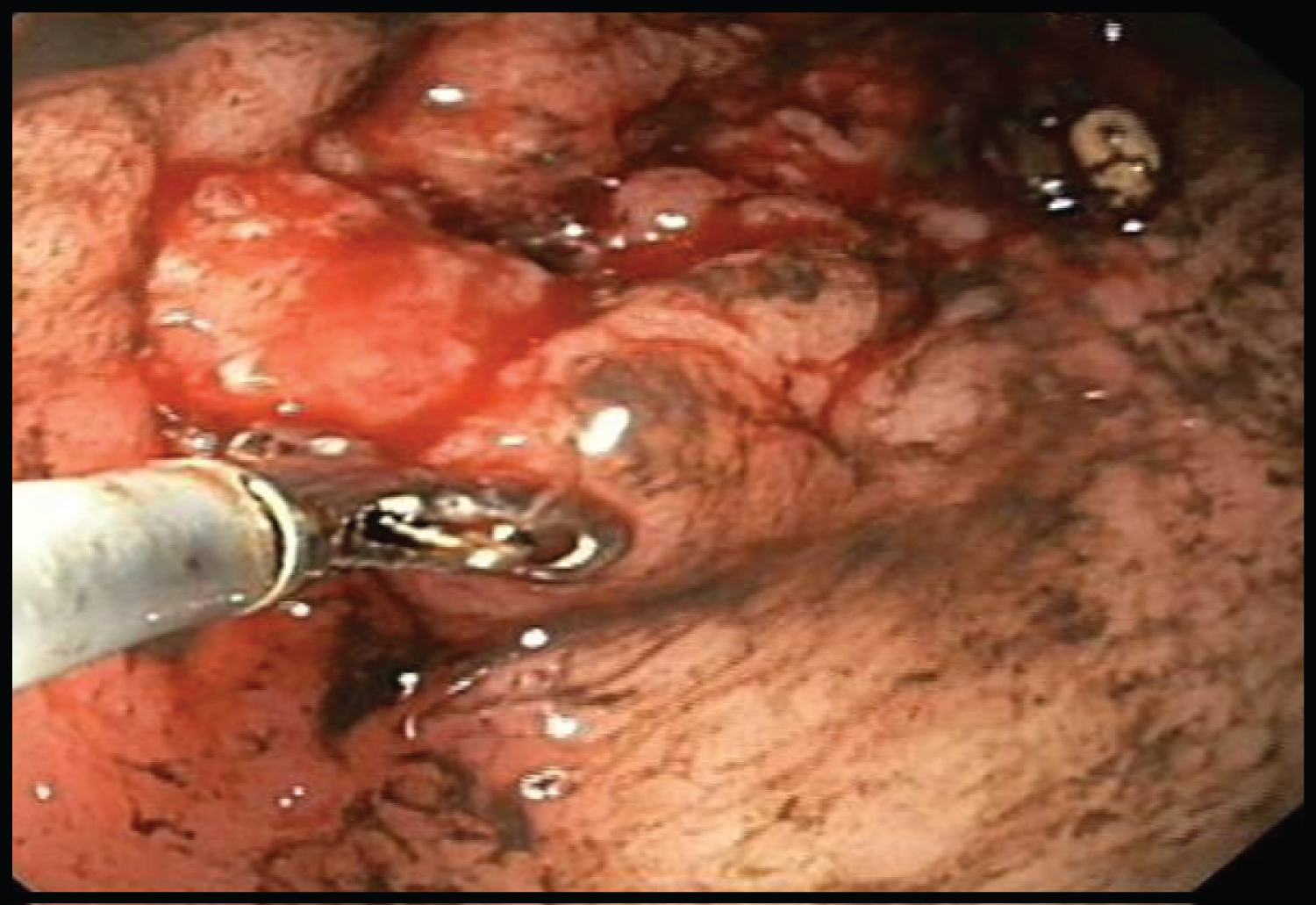 Figure 2a: Adenocarcinoma Stomach (endoscopy image).
View Figure 2a
Figure 2a: Adenocarcinoma Stomach (endoscopy image).
View Figure 2a
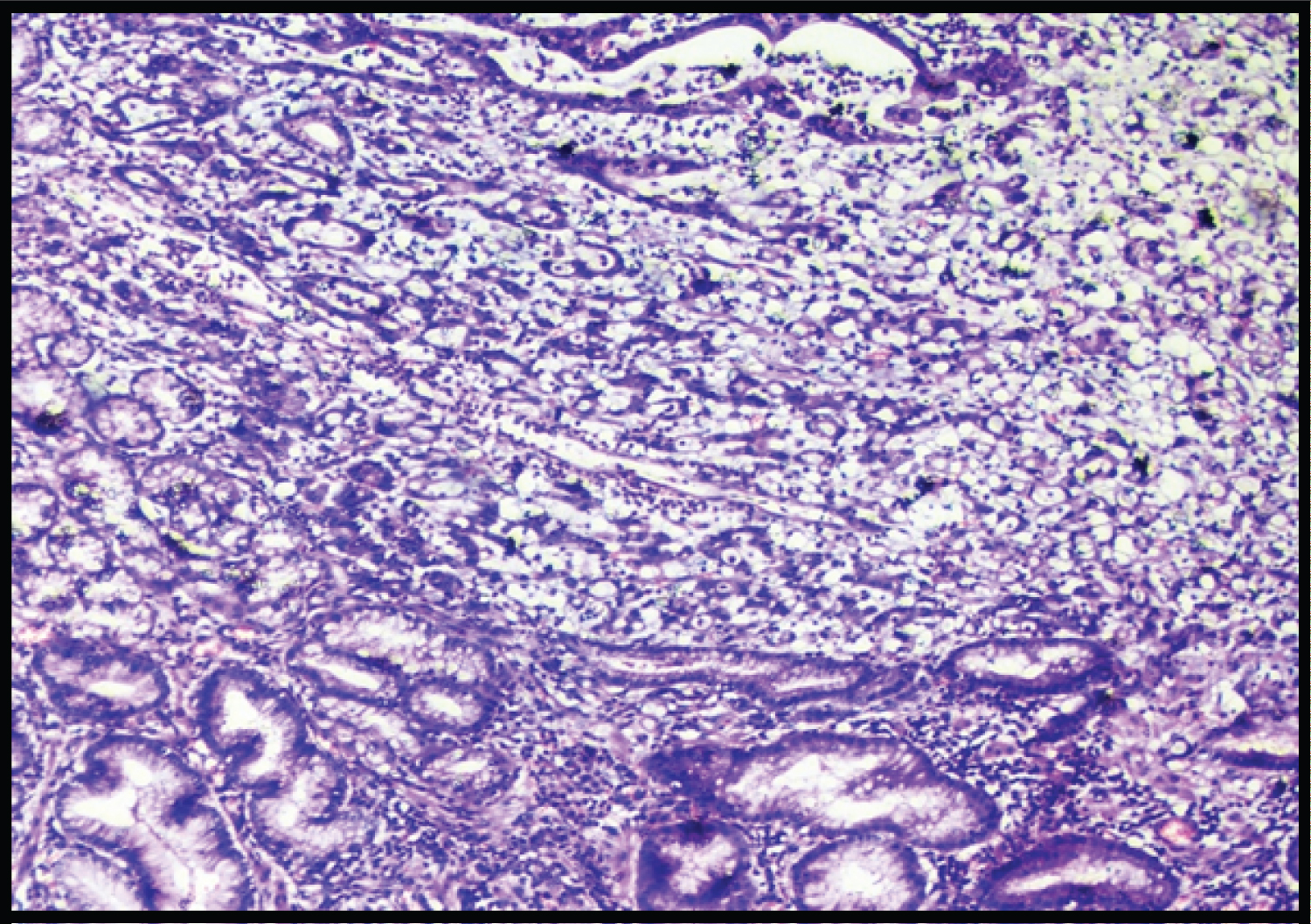 Figure 2b: Adenocarcinoma stomach (H&E).
View Figure 2b
Figure 2b: Adenocarcinoma stomach (H&E).
View Figure 2b
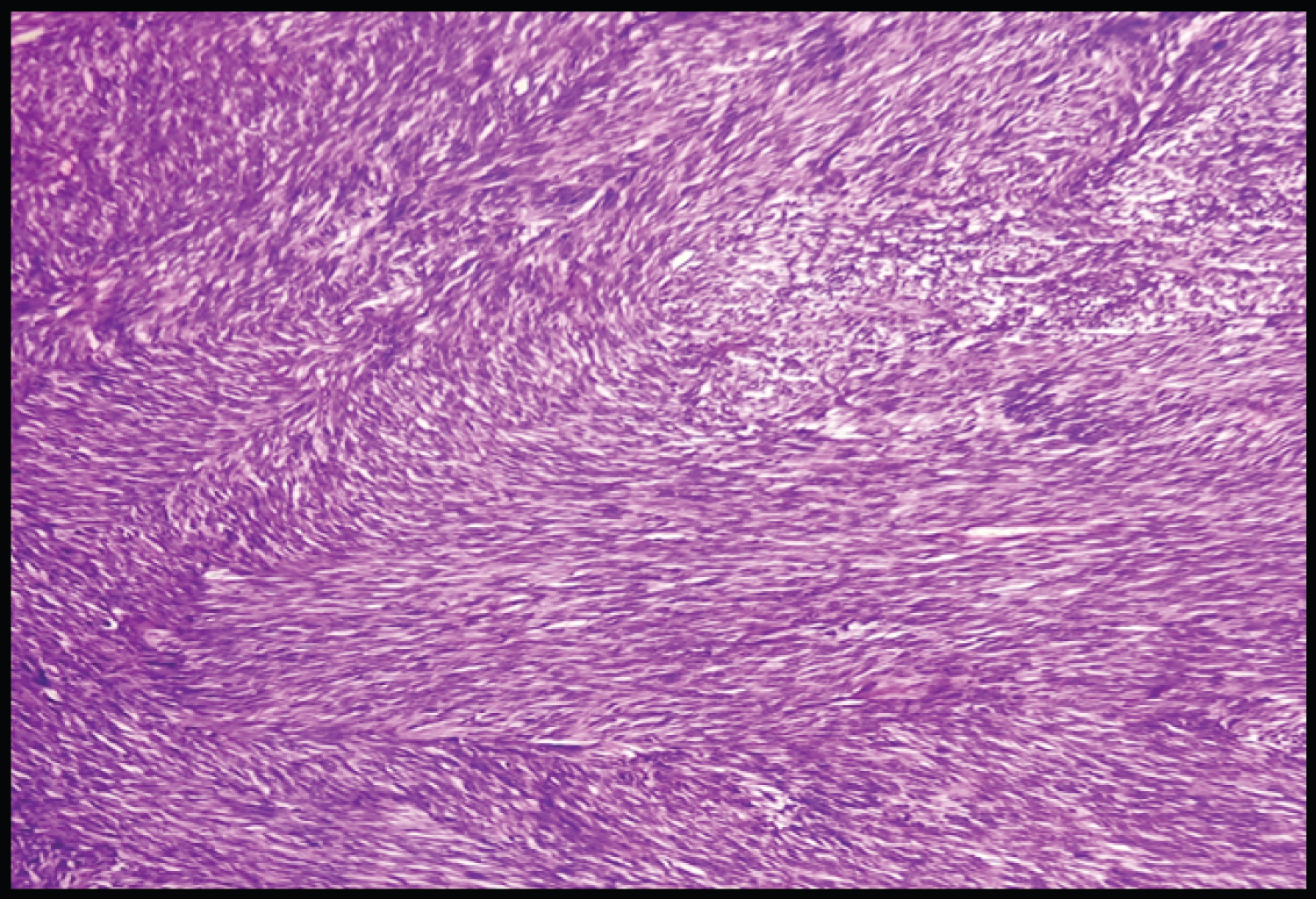 Figure 3: GIST (Gastrointestinal Stromal Tumor) (H&E).
View Figure 3
Figure 3: GIST (Gastrointestinal Stromal Tumor) (H&E).
View Figure 3
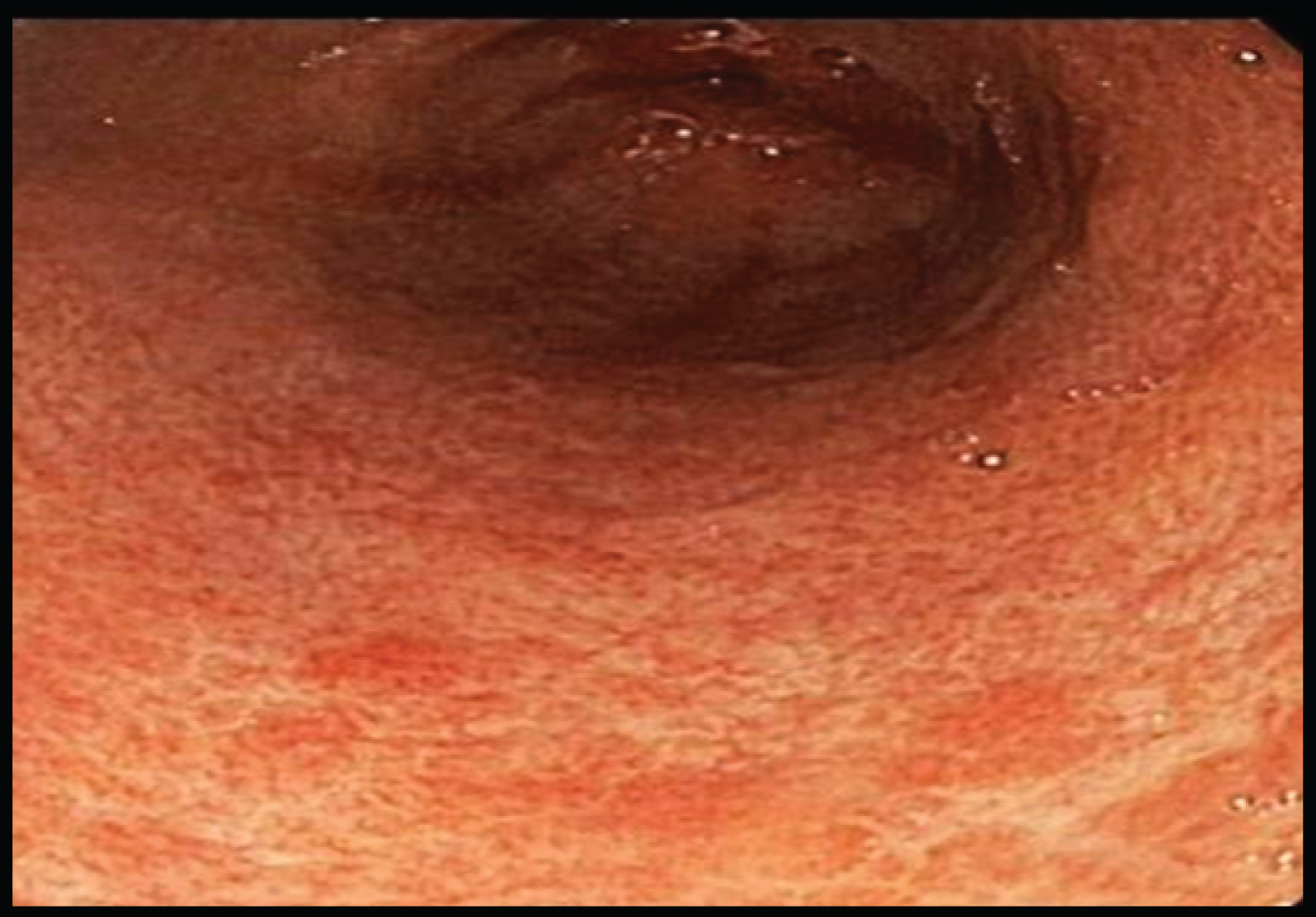 Figure 4a: Non-specific gastritis (endoscopy image).
View Figure 4a
Figure 4a: Non-specific gastritis (endoscopy image).
View Figure 4a
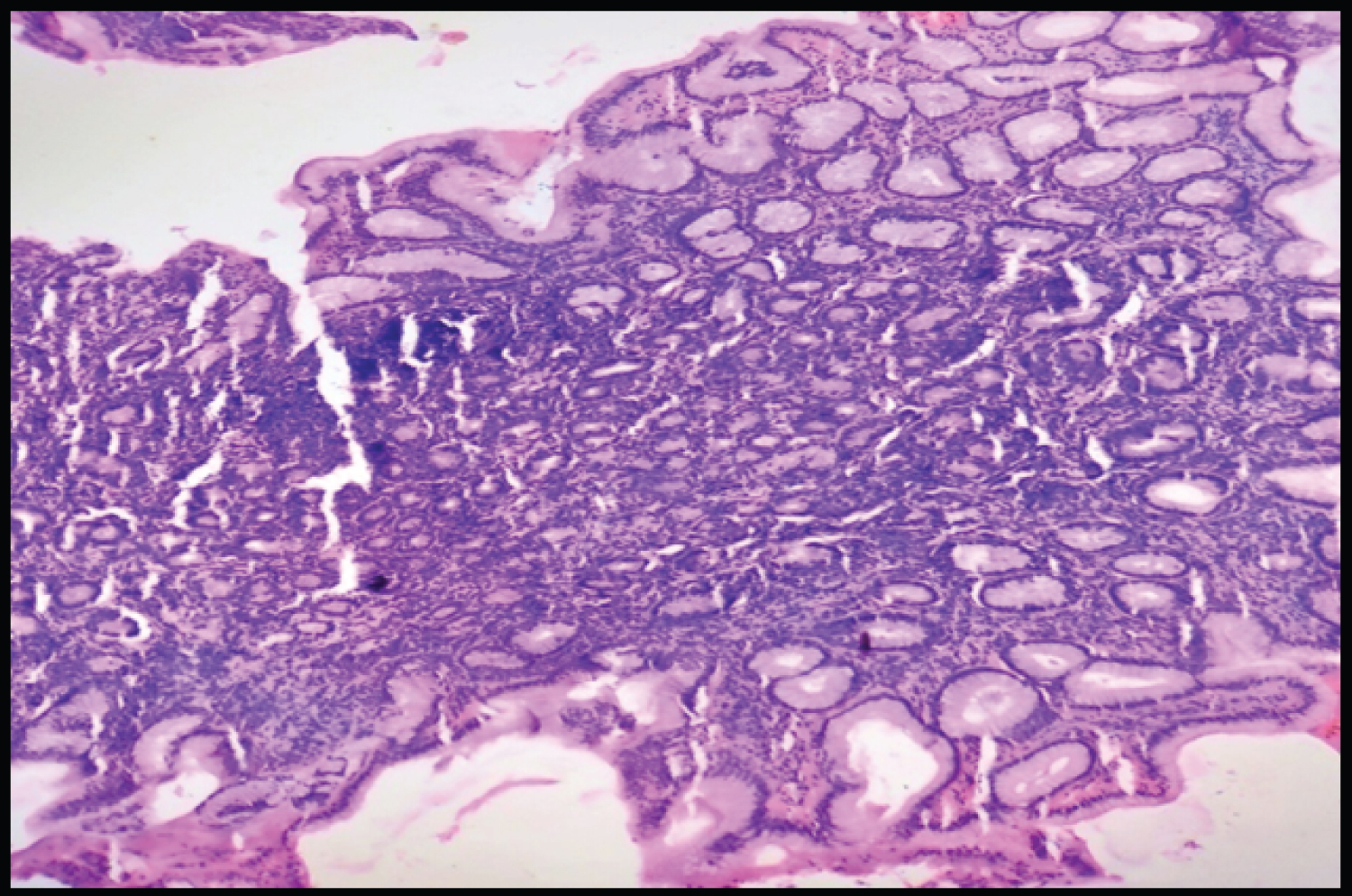 Figure 4b: Non-specific gastritis (H&E).
View Figure 4b
Figure 4b: Non-specific gastritis (H&E).
View Figure 4b
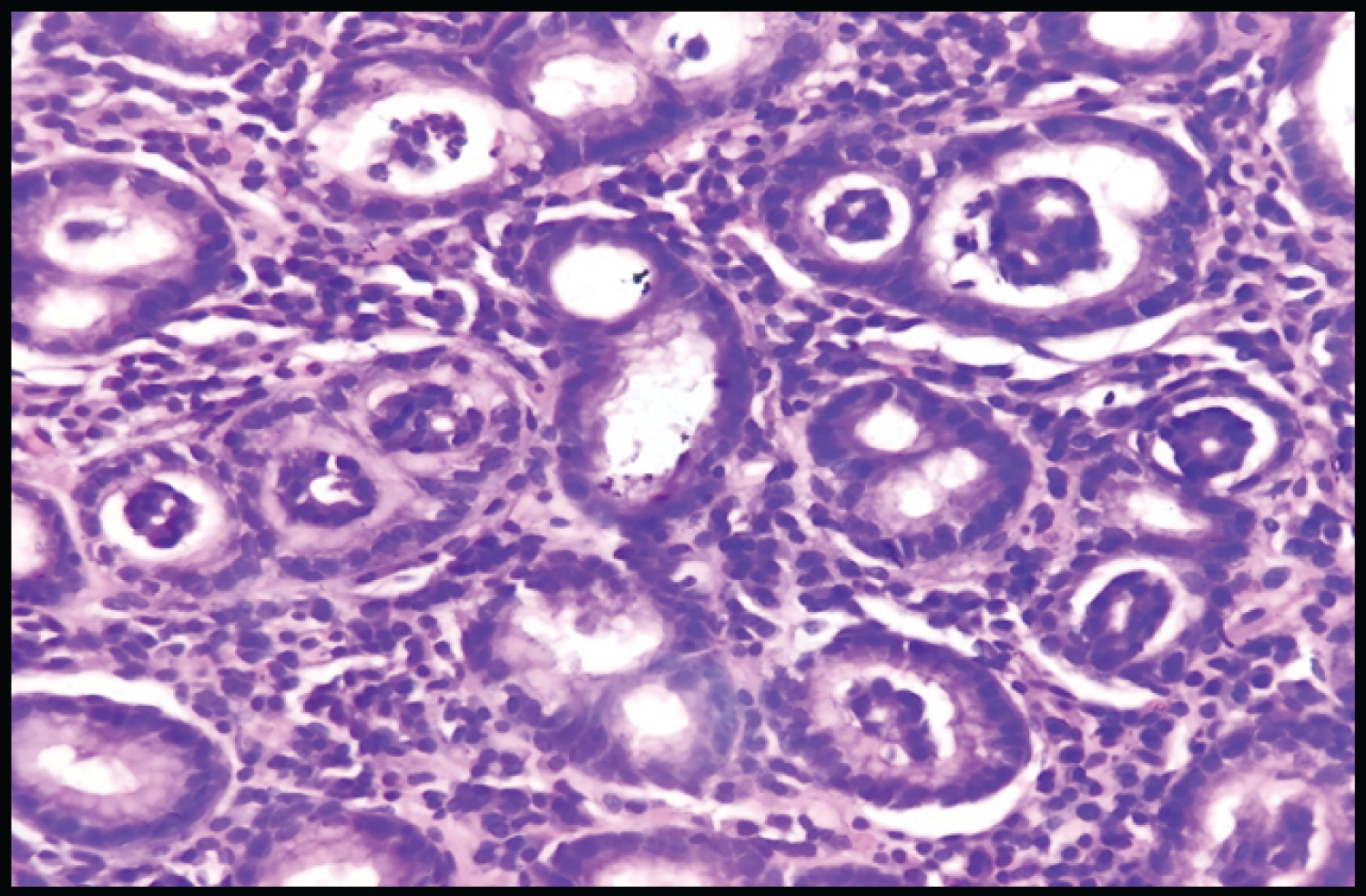 Figure 5a: H. Pylori gastritis (H&E).
View Figure 5a
Figure 5a: H. Pylori gastritis (H&E).
View Figure 5a
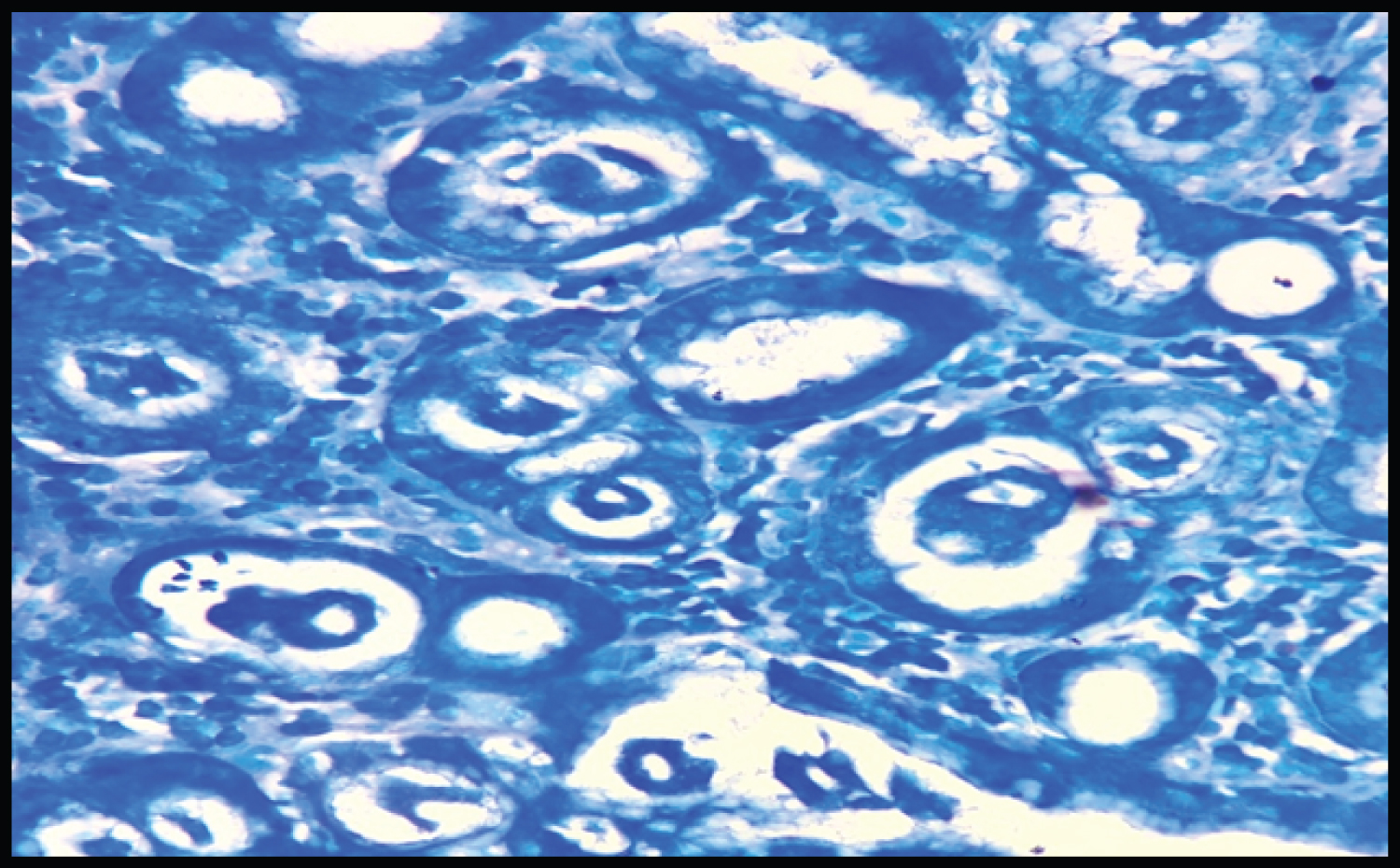 Figure 5b: H. Pylori gastritis (Giemsa stain).
View Figure 5b
Figure 5b: H. Pylori gastritis (Giemsa stain).
View Figure 5b
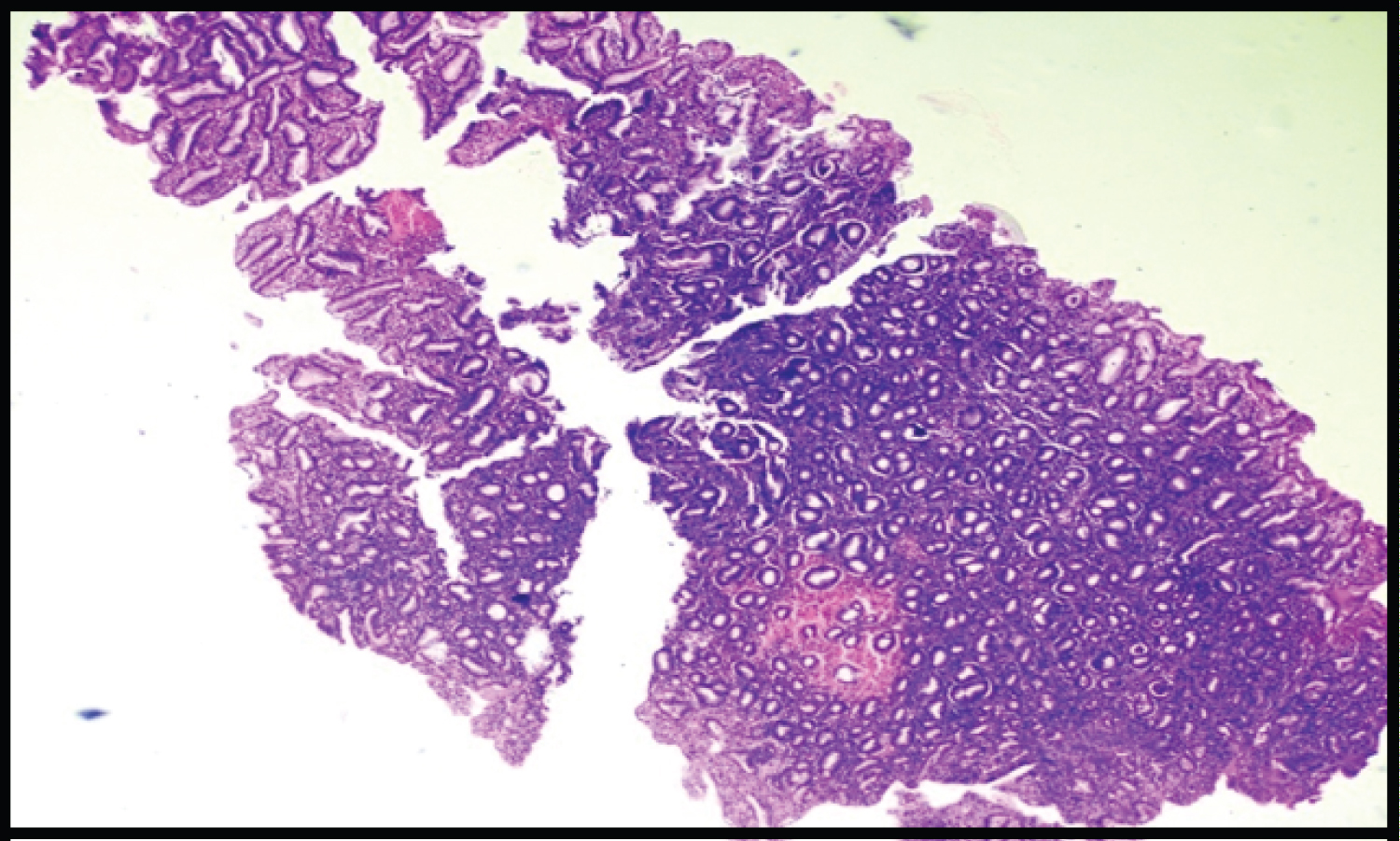 Figure 6: Atrophic gastritis (H n E).
View Figure 6
Figure 6: Atrophic gastritis (H n E).
View Figure 6
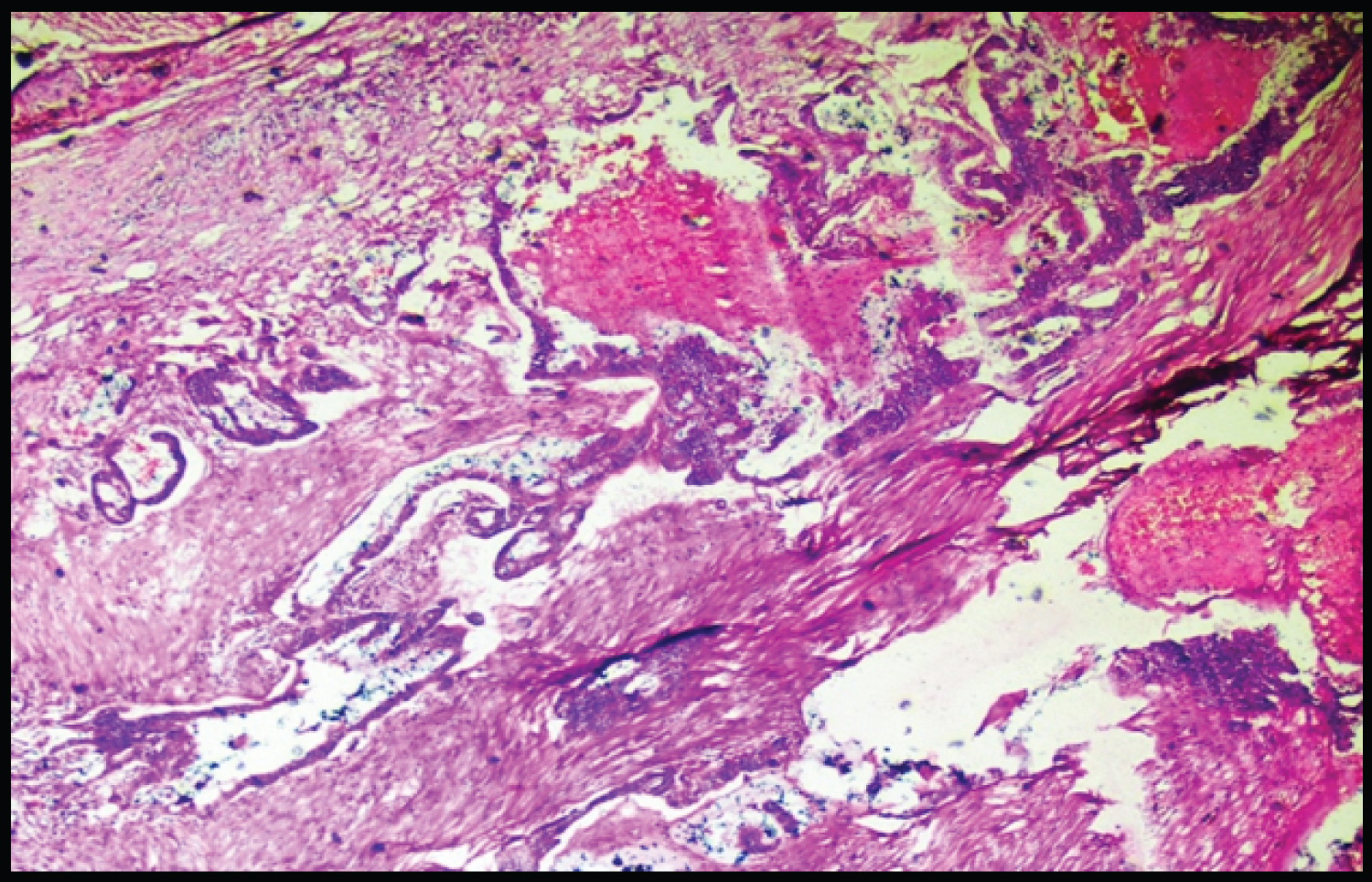 Figure 7: Adenocarcinoma Ileum (H&E).
View Figure 7
Figure 7: Adenocarcinoma Ileum (H&E).
View Figure 7
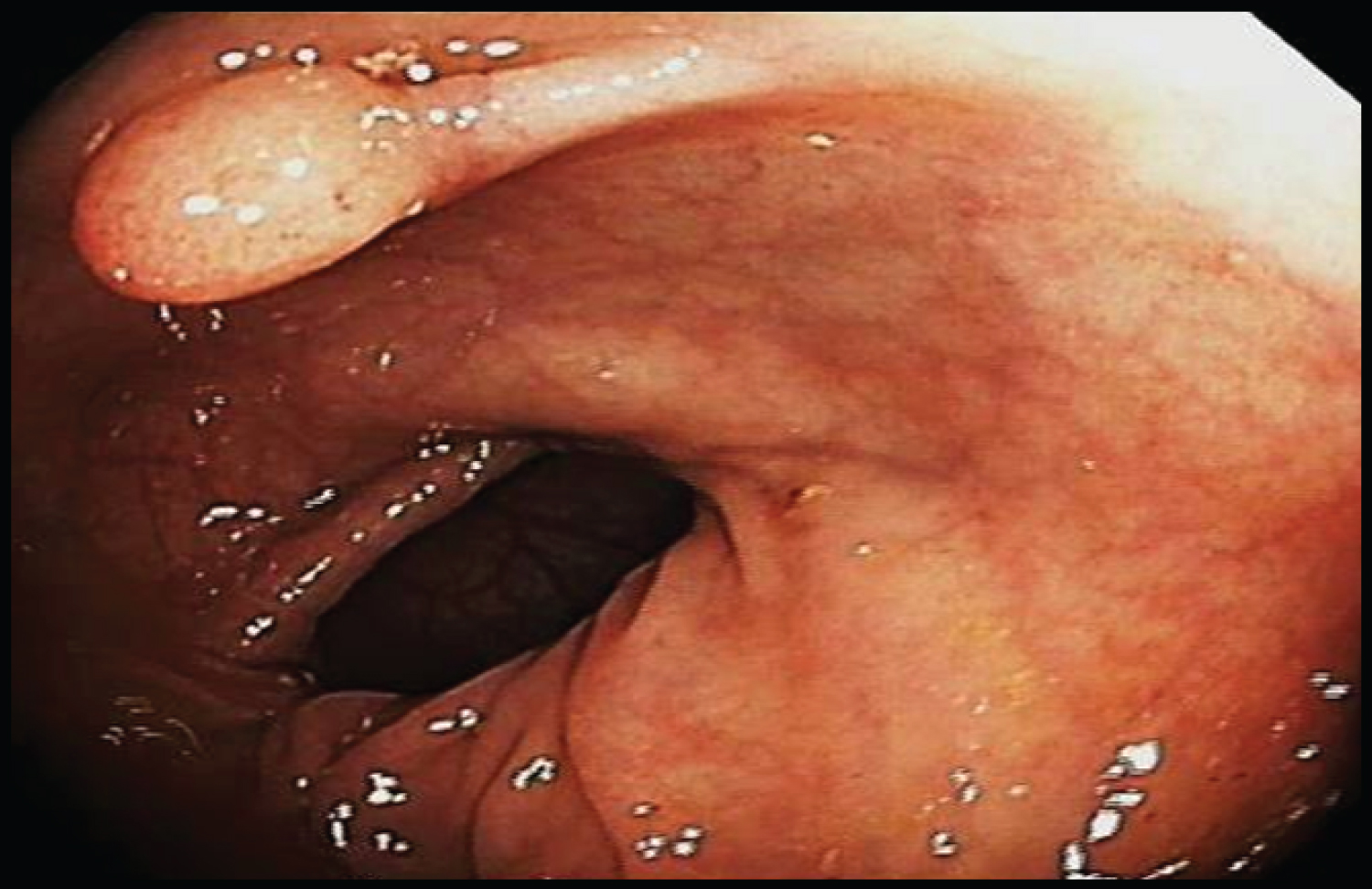 Figure 8a: Rectal polyp (endoscopy image).
View Figure 8a
Figure 8a: Rectal polyp (endoscopy image).
View Figure 8a
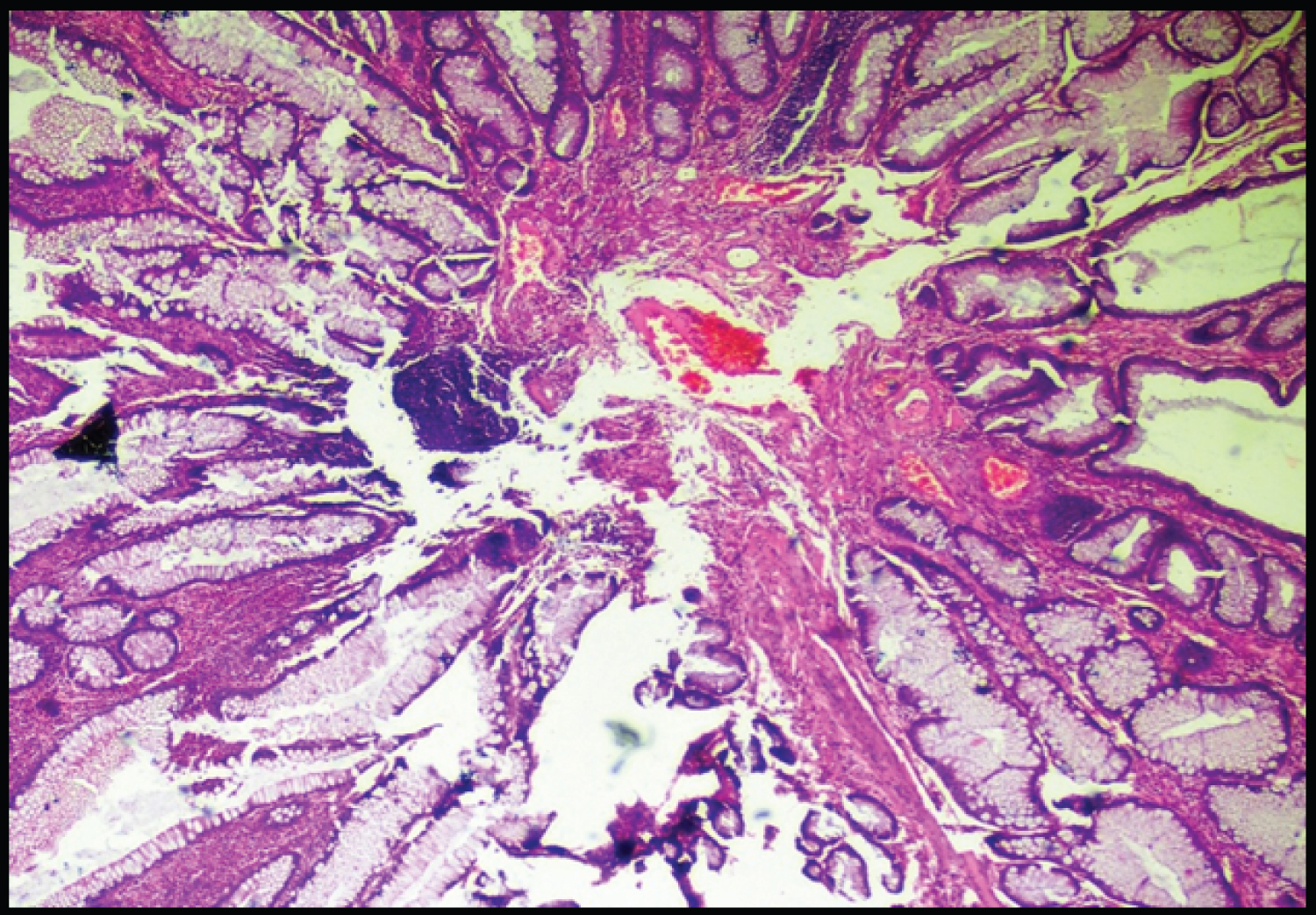 Figure 8b: Rectal polyp (H&E).
View Figure 8b
Figure 8b: Rectal polyp (H&E).
View Figure 8b
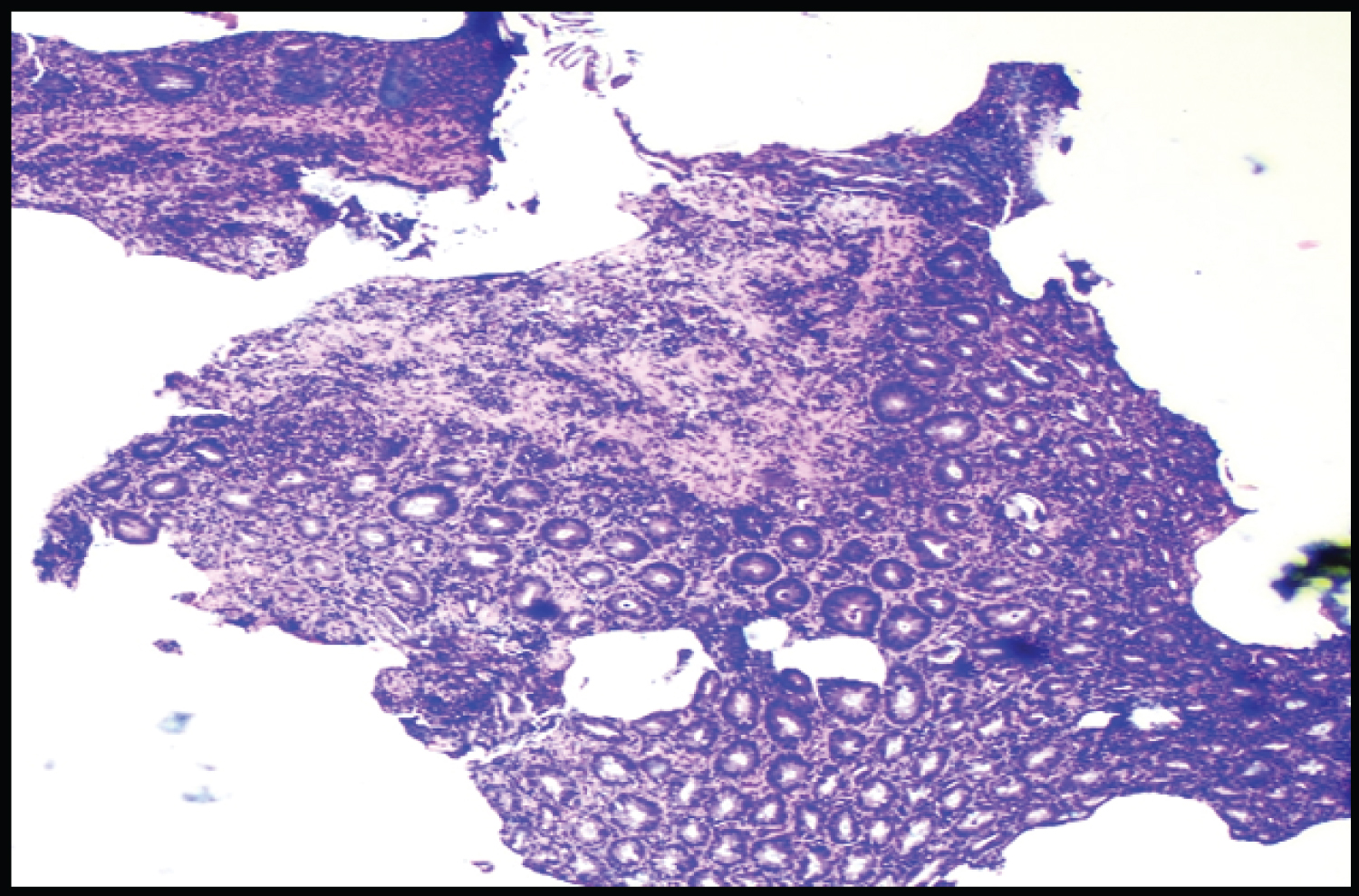 Figure 9: Proctitis (H&E).
View Figure 9
Figure 9: Proctitis (H&E).
View Figure 9
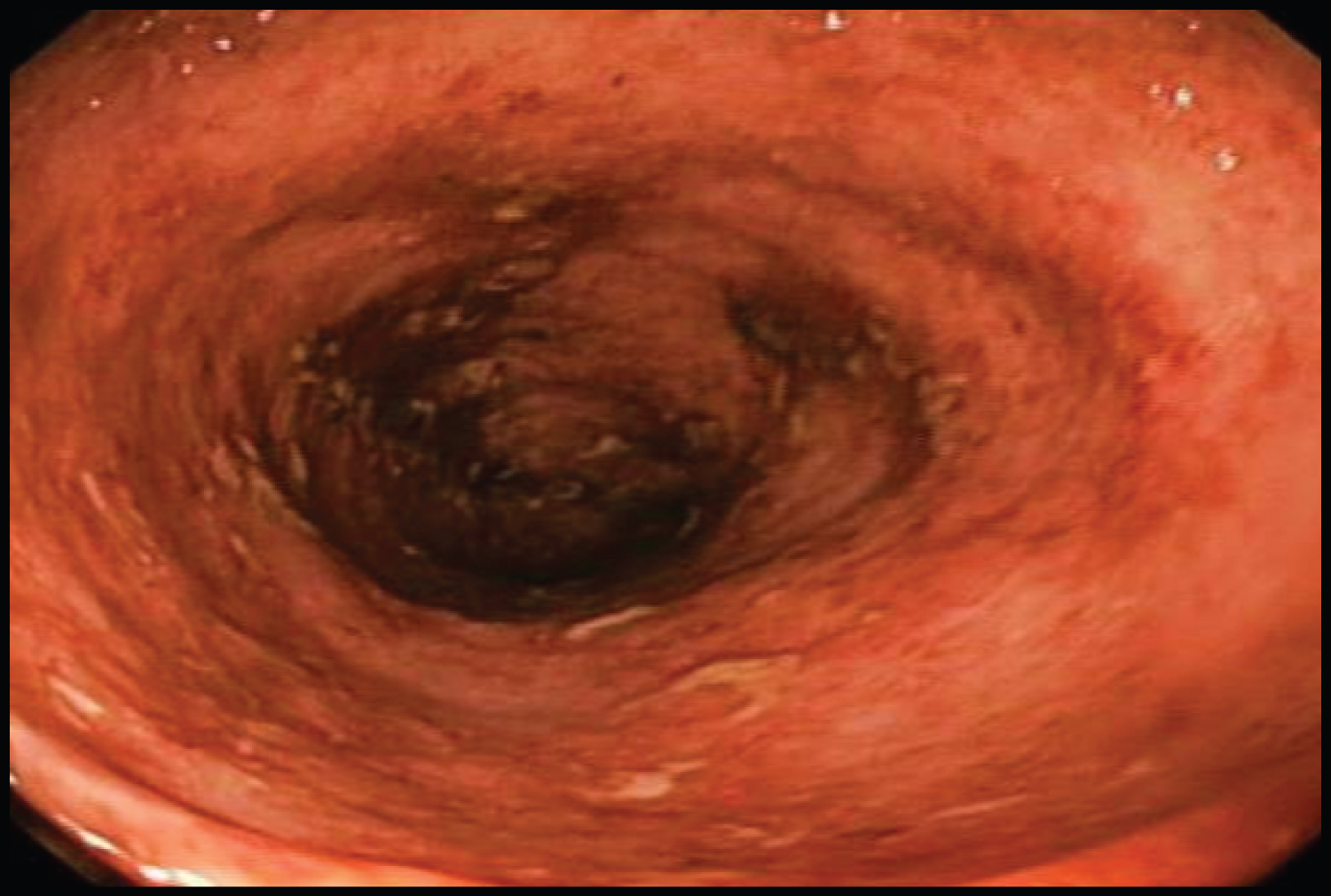 Figure 10a: Ulcerative colitis (endoscopy image).
View Figure 10a
Figure 10a: Ulcerative colitis (endoscopy image).
View Figure 10a
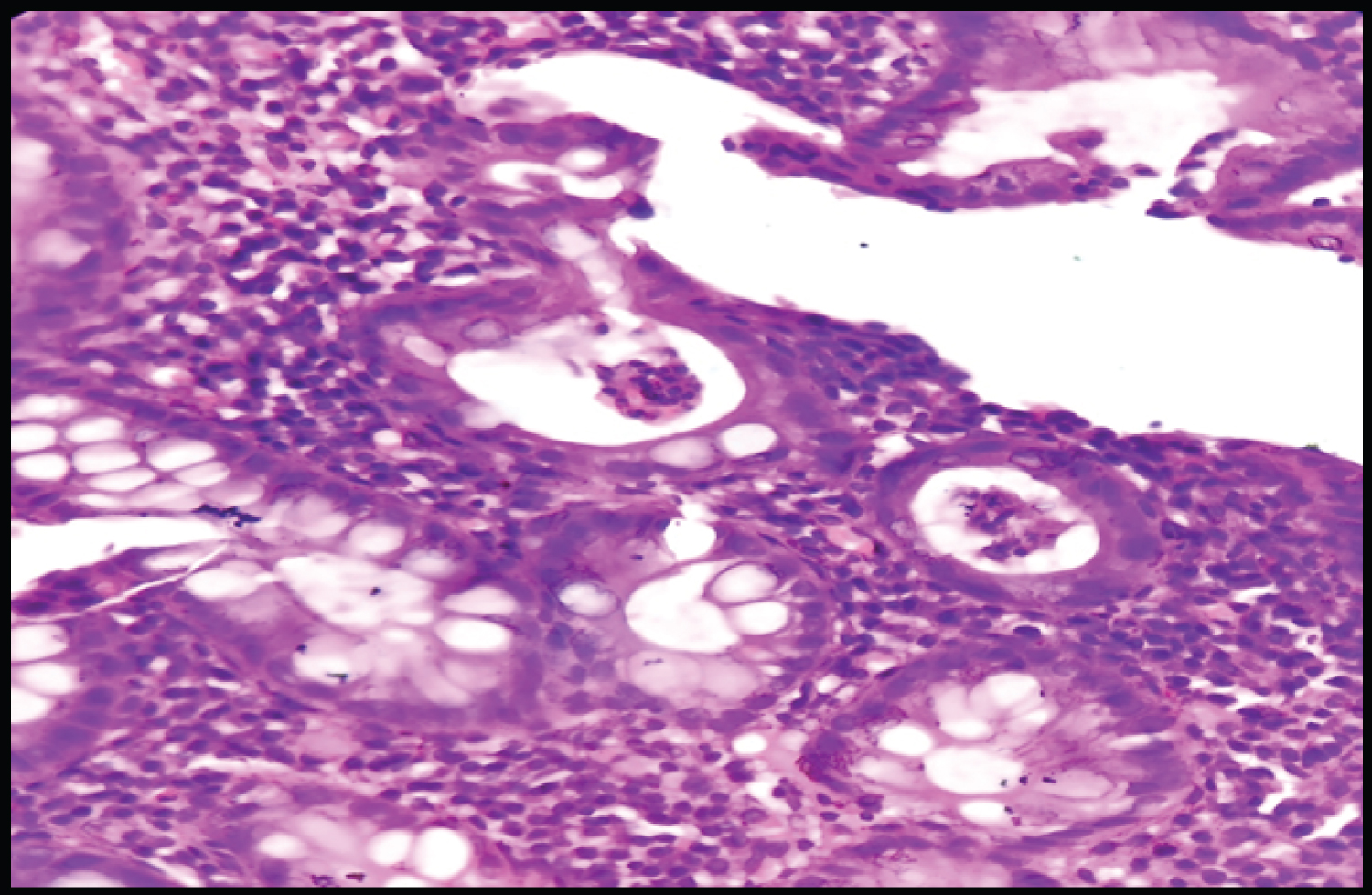 Figure 10b: Ulcerative colitis (H&E).
View Figure 10b
Figure 10b: Ulcerative colitis (H&E).
View Figure 10b
 Figure 11: Hirschsprung disease (H&E).
View Figure 11
Figure 11: Hirschsprung disease (H&E).
View Figure 11
Table 5: Histopathological spectrum of upper GI endoscopic biopsies. View Table 5
Table 6: Histopathological spectrum of lower GI endoscopic biopsies. View Table 6
Among the paediatric population, duodenal biopsies (29 cases, 46.5%) were most frequent and most common diagnosis being celiac disease (14 cases, 22%). In adults, stomach (190 cases, 47%) was most common site of GI endoscopic biopsies, and non-specific inflammation (105 cases, 26%) was most frequent diagnosis. While, in geriatric group esophageal biopsies (32 cases, 36%) were most common, with squamous cell carcinoma (24 cases, 28%) being most common diagnosis made (Table 7).
Table 7: Correlation of clinical, endoscopic and histopathological diagnosis. View Table 7
GI lesions are commonly encountered pathology in routine clinical practice. They are broadly categorised as upper and lower GI lesions based on site. Histopathological study of endoscopic biopsies plays a critical role in early detection of malignant lesions and is also used to monitor the disease course. The risk of GI malignancies increases with advancing age and increased use of endoscopic biopsies have led to early detection of these lesions. In the present study, a total of 556 endoscopic biopsies from upper and lower GI tract were evaluated over the period of 5 years.
It was observed that the incidence of GI lesions was higher in adult population presenting with an age range of 13 to 59 years (72%). Overall number of GI endoscopic biopsies in paediatric group (< 12%) was less comparatively. The age related difference could be due to the variation in risk factors among different age groups. Since the probability of malignancy increases with advancing age, all the suspicious lesions on endoscopy are subjected to biopsy for histopathological analysis. These findings are in concordance with the study conducted by Rashmi, et al. [3], Abilash SC, et al. [4], and Ganga, et al. [5] where majority of GI lesions were in 4th and 5th decade.
In the present study, male preponderance was recorded in all age-groups with male to female ratio being 1.4:1, 1.5:1 and 1.6:1 respectively in paediatric, adult and geriatric group. A male predisposition for GI lesions has been a consistent finding of various studies conducted in different parts of the country. A clear cut male predominance was observed in studies conducted by Hussain, et al. [6], Rashmi, et al. [3] and Ganga, et al. [5] who reported male to female ratio of 2.8:1, 2.03:1 and 1.57:1 respectively. This male predisposition maybe because males are more exposed to risk factors in comparison to females.
In the present study, incidence of upper GI endoscopic biopsies was higher than lower GI endoscopic biopsies in all the age groups. The findings of our study correlated with the observations of Rashmi, et al. [3]. They also reported predominance of upper GI lesions on endoscopic biopsies, with 27% lesions occuring in 5th and 6th decade.
In our study, benign lesions outnumbered the malignant lesions in all age-groups. Out of 65 endoscopic biopsies in paediatric population, 64 biopsies (98%) were benign. Similarly, in adults and geriatric group 76% and 61% biopsies were benign respectively. Rashmi, et al. [3] documented similar findings. They reported the incidence of benign esophageal lesions to be 56% and that of malignant lesions to be 44%. They also reported higher incidence of benign gastric lesions (60%) than malignant lesions (40%). Our observations were again in conformity with the findings of Ganga, et al. [5] where majority of lesions were non-neoplastic.
In this study, stomach was the most common site of biopsy followed by duodenum in the adult group. While in geriatric population, esophageal biopsies were more commonly seen. Our findings were concordant with the study done by Ganga, et al. [5] in which most common site of endoscopic biopsy was stomach followed by duodenum and esophagus. Venkatesh, et al. [2] also reported gastric biopsies to be most common (57% of total 180) GI biopsies. This is similar to study done by Prasad PR [7] and Bilal, et al. [8] who observed gastric biopsies to be most common biopsy received accounting for 56% and 64.8% of total GI biopsies. In our study, among lower GI biopsies rectal biopsy was most common in all age-groups. Venkatesh, et al. [2] showed colon to be the most common site of lower GI biopsies, this finding was discordant with our study.
In the present study, most common lesion in esophagus was squamous cell carcinoma mainly affecting adult age-group followed by geriatric group. The other malignant neoplasm encountered was Adeno-squamous carcinoma. Our findings are in conformity with the study done by Rashmi, et al. [3], Mchembe, et al. [9], Abilash SC, et al. [4] and Shanmugaswamy, et al. [10]. Among non-neoplastic lesions, non-specific inflammation was most common which is similar to the findings by Ganga, et al. [5].
In this study, among gastric biopsies non-neoplastic lesions were common than neoplastic lesions. Out of 190 gastric biopsies in adults, 183 were non-neoplastic and in geriatric group 18 out of 22 biopsies were non-neoplastic. Ganga, et al. reported similar findings, out of 93 gastric biopsies 68 were inflammatory lesions [5]. Among the non-neoplastic lesions (183 cases), highest number of cases fell under the group of non-specific inflammation (105 cases). Similar observations were made by Somani, et al. [11] (40%), Rashmi, et al. [3] (37%). H. Pylori induced gastritis was next most frequently encountered inflammatory lesion in our study, accounting for 14% of all gastric lesions in adults and 6% in elderly patients. In the current study, we didn’t encounter any case of gastric ulcer on endoscopic biopsy. This maybe because most of the patients presenting with symptoms suggestive of gastric ulcer were treated either directly without conforming diagnosis with endoscopy or after performing urea breath test to detect H. pylori.
In the present study, we found all the cases of gastric malignancy as Adenocarcinoma. No malignancy was seen in paediatric group. These observations are again in conformity with the findings of Shiva, et al. [12], Rashmi, et al. [3] and Bilal, et al. [8] who reported adenocarcinoma as most common gastric malignancy. 7 cases of GIST were also reported in our study (4 in adults, 2 in elderly and 1 in paediatric group).
In our study, most common lesion on duodenal biopsy in adults was non-specific inflammation followed by duodenal ulcer. While in paediatric group, celiac disease was commonly encountered. No malignancy was reported in the study. These findings are similar to those of Venkatesh, et al. [2].
The lower GI lesions in present study showed a variable spectrum comprising of non-neoplastic, benign and malignant lesions. Adenocarcinoma was most only malignancy encountered in Ileum. Most common lesion on colonic biopsy in adults was lymphocytic colitis followed by non-specific colitis. 4 cases of Tubular adenoma (2 each in adults and elderly group) were also seen. Ventakesh, et al. reported non-specific colitis as commonest lesion on colon biopsy [2], this finding was discordant with our study.
Among the paediatric group, out of 20 rectal biopsies rectal polyp 13 (20%) was most common diagnosis. 2 cases of Hirschsprung disease and 1 case of Solitary rectal ulcer was also detected in our study. Inflammatory bowel disease was most common diagnosis in adults contributing 7 out of total 18 cases. In a study conducted by Al Brahim, et al. rectal ulceration was most common finding followed by rectal polyps [13].
In this study, most of the histologically confirmed cases of malignancy were either reported as simple growth or ulcerative growth, some also presented as mucosal thickening. This is in concordance with the findings of Somani, et al. who reported growth and mucosal thickening as most common endoscopic finding in malignant lesions [11]. In a study by Rashmi, et al. 90% lesions endoscopically detected as growth turned out malignant [3]. Polyps and Adenomas also presented as growth. Most of non-neoplastic lesions either presented as erythema or as ulcerated mucosal lining.
In our study, a variety of non-neoplastic and neoplastic lesions were studied. Out of 556 GI endoscopic biopsies, maximum numbers of cases were detected in adult age group. Duodenal biopsies were more frequent in paediatric group, with celiac disease being most common diagnosis. In adults, gastric biopsies were maximum, most common being non-specific inflammation. In geriatric group, maximum were esophageal biopsies with squamous cell carcinoma as most common diagnostic entity.
Due to tiny biopsy material limitations in diagnostic interpretation are often encountered. Multiple biopsies from abnormal appearing mucosa on endoscopy may aid with definitive diagnosis and also reduces chances of error. In case of dubious lesions, biopsy results served to correct mistaken endoscopic findings. Hence, we concluded that endoscopy in combination with biopsy is a powerful diagnostic tool in detecting as well monitoring disease course and patient outcome. In addition, it has the advantage of being cost-effective and can be incorporated easily in routine diagnostic protocols.
Nil.
Nil.