Langerhans cell histiocytosis is a rare disease and due to its heterogeneous presentation represents a diagnostic and therapeutic challenge. We present the case of a patient with diabetes insipid us and panhypopituitarism, with the appearance of painful vulvar ulcers. The vulvar biopsy confirmed Langerhans cell histiocytosis with spreading to multiple organs, so it was decided to start chemotherapy, achieving the complete elimination of all lesions.
A systematic review of the literature was carried out in search of all articles in English or Spanish, published until September 2018, related to the diagnosis and treatment of Langerhans cells histiocytosis in the vulva. Two authors independently searched the PUBMED, EMBASE, COCHRANE, LILACS and SCIELO databases with the keywords "Vulva" AND "Langerhans cells Histiocytosis" OR "Vulva" AND "Histiocytosis X". The information obtained in the review was organized through a data collection instrument that included the following variables: year of publication, study design, age, symptoms, history, morphology of the lesions, histopathological examination, management, follow-up time after treatment and presence of relapse. A total of 131 articles were found with full text available. 55 articles met the eligibility criteria reporting a total of 61 cases. The main symptoms reported were pruritus, vulvar pain and dyspareunia. At the vulvar physical exam, the main
findings were papules, nodules, vesicles, ulcers and erythematous plaques in the labia majora and minora. Nowadays, there are no clearly established protocols for the management of these patients.
Hand-Schuller-Christian Disease, Vulvar Histiocytosis X, Langerhans cell, Diabetes insipidus, Panhypopituitarism, Skin manifestations, Vulvar Biopsy
Vulvoscopy
Langerhans cell histiocytosis, also known as Histiocytosis X, is a disease characterized by clonal proliferation of myeloid-derived dendritic cells [1]. These cells reside in the skin and can migrate to the lymph nodes to present antigens to T and B lymphocytes [2]. It occurs predominantly in childhood and the incidence rate has been calculated at 8.9 / million per year in children under 15 years of age [3].
The pathophysiology is still unknown, but it has been suggested that the absence of Alpha Tumor Necrosis Factor and Cadherin E allows the dissemination of histiocytosis from a lesion located in the skin [4]. The etiology is probably multifactorial, but the Herpesvirus type 6 and the Epstein Barr can act as inducers of proliferation [5].
The spectrum of manifestations varies from isolated lesions to a disseminated disease with multiorgan involvement. The forms of presentation include pure genital lesions, subsequent multi-organ involvement, oral and cutaneous involvement with subsequent genital lesions, and diabetes insipidus with organic involvement [6]. When lesions are found in high-risk organs (bone marrow, lung, liver, spleen or central nervous system) the response to treatment decreases significantly [1]. The involvement of the pituitary gland can give rise to panhypopituitarism with important deficiencies of growth hormone, thyroid stimulating hormone, antidiuretic hormone and gonadotropins, this type of commitment is typically manifested with diabetes insipidus and amenorrhea. Systemic involvement occurs mainly in children and local involvement in adults.
Lesions in the lower genital tract are infrequent and include the appearance of pruritic rash, papules, nodules, plaques and ulcers, among others. Within the female genital tract, the vulva is the most frequent site of involvement. The differential diagnosis includes sexually transmitted diseases, tuberculosis, lichen sclerosus, melanoma, sarcoma, and Paget's disease [7]. In children, seborrheic dermatitis, psoriasis and scabies should also be considered [3]. It is important to note that Langerhans histiocytosis has been confused with suspicious signs of sexual abuse in children because of its genital manifestations. Histopathological examination reveals the presence of abnormal Langerhans cells in an inflammatory background of eosinophils, histiocytes, neutrophils and lymphocytes. Histiocytic cells are characterized by the presence of abundant cytoplasm and a horseshoe-shaped nucleus with moderate atypia [8]. The diagnosis is confirmed by immunohistochemistry and electron microscopy studies. Langerhans cells are positive for the proteins CD1A, CD207 (Langerin) and S-100. Electron microscopic examination shows the presence of Birbeck granules in the cytoplasm [8]. The CD207 protein is the most specific marker.
According to the degree of commitment, the proposed treatment can vary between only local resection and the application of topical corticosteroids or nitrogen mustard, up to the requirement of radical vulvectomy associated with adjuvant management with chemotherapy or radiotherapy. Some studies have proposed thalidomide as a good option for patients with recurrent disease. Thalidomide acts as a downstream regulator of adhesion molecules interfering with the adhesion of T cells to antigen presenting cells and preventing the activation of T cells. The teratogenic effects and the risk of thromboembolic events and peripheral neuropathy have limited its use [9].
Here we report a rare case of vulvar Langerhans cell histiocytosis with multisystem involvement. Due to the fact of its heterogeneous presentation, it represents a diagnostic and therapeutic challenge. Nowadays, there are no clearly established protocols for the management of these patients.
We describe the case of a nulliparous 29 years old Hispanic female. She presented a vulvoscopy assessment with a 10 months history of painful vulvar and inframammary lesions, which had increased in number and had not improved with the application of topical antifungal nor with topical and systemic corticosteroids. She had a history of hypophysis tumor resection a year ago, panhypopituitarism, secondary amenorrhea and diabetes insipidus.
Vulvoscopy showed hypopigmentation of the labia majora, ulcerative lesions with a clean background, irregular and erythematous borders, and some excavated lesions without signs of superinfection, which affected the labia majora, labia minora and the perineal region (Figures 1). Screening for sexually transmitted diseases revealed a history of herpes virus type I and II infection without active disease. The biopsy of vulvar lesions identified the presence of Langerhans cells. Immunohistochemical markers show intense positivity for CD1a, CD68 and S100 and negative for HMB 45, CKAE1 / 3 and EMA. Microorganism colorations were negative (Figure 2, Figure 3, Figure 4, Figure 5).
 Figure 1: Ulcerative lesions in labia majora, labia minora and perineal region. (Findings in physical exam)
View Figure 1
Figure 1: Ulcerative lesions in labia majora, labia minora and perineal region. (Findings in physical exam)
View Figure 1
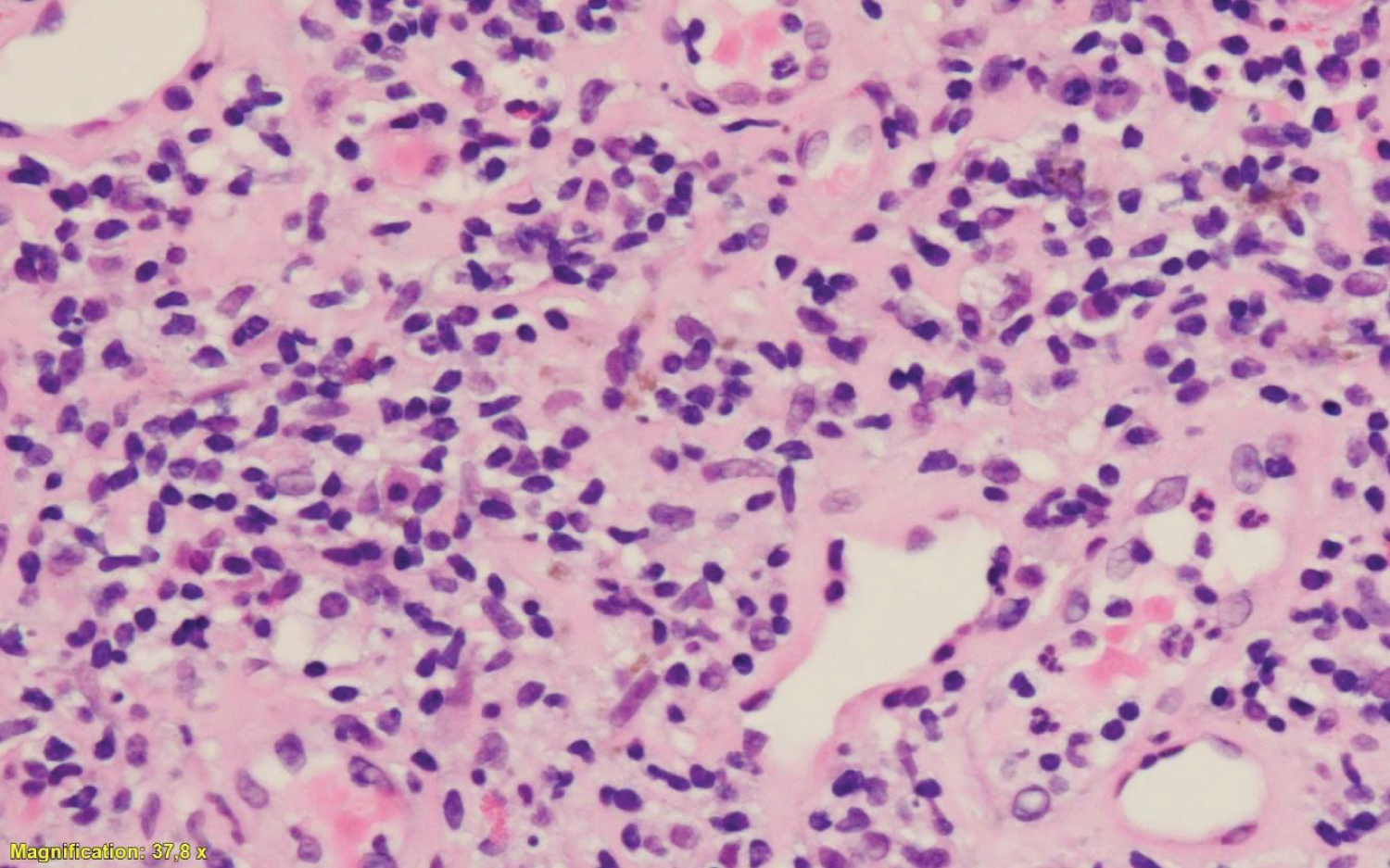 Figure 2: Langerhans cells with eosinophilic, big-sized cytoplasm accompanied by neutrophils and focal eosinophils. (37, 8 x, HE). (Histopathological findings)
View Figure 2
Figure 2: Langerhans cells with eosinophilic, big-sized cytoplasm accompanied by neutrophils and focal eosinophils. (37, 8 x, HE). (Histopathological findings)
View Figure 2
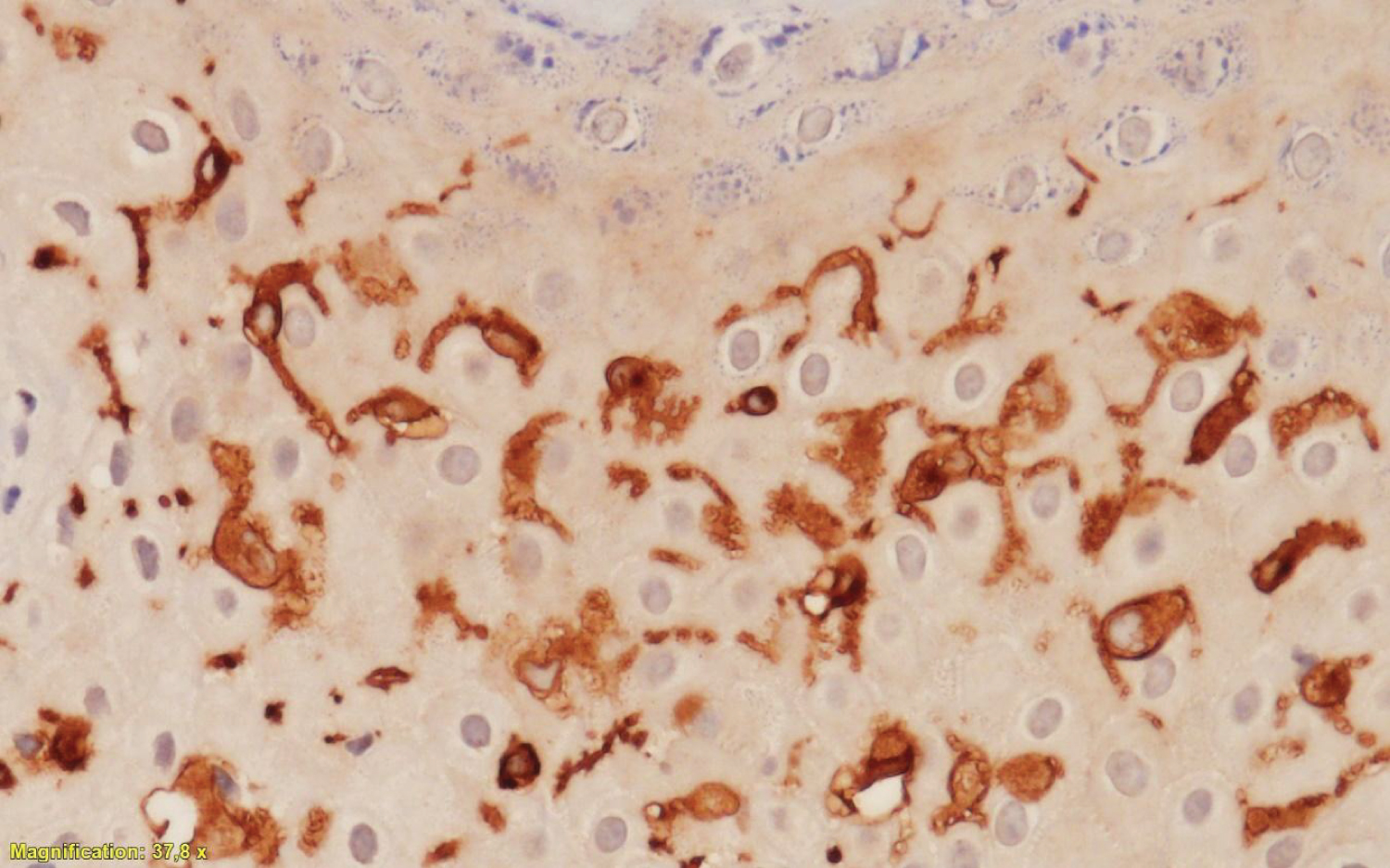 Figure 3: Langerhans cells demonstrating strong positivity to CD1marker (37, 8 x). (Histopathological findings)
View Figure 3
Figure 3: Langerhans cells demonstrating strong positivity to CD1marker (37, 8 x). (Histopathological findings)
View Figure 3
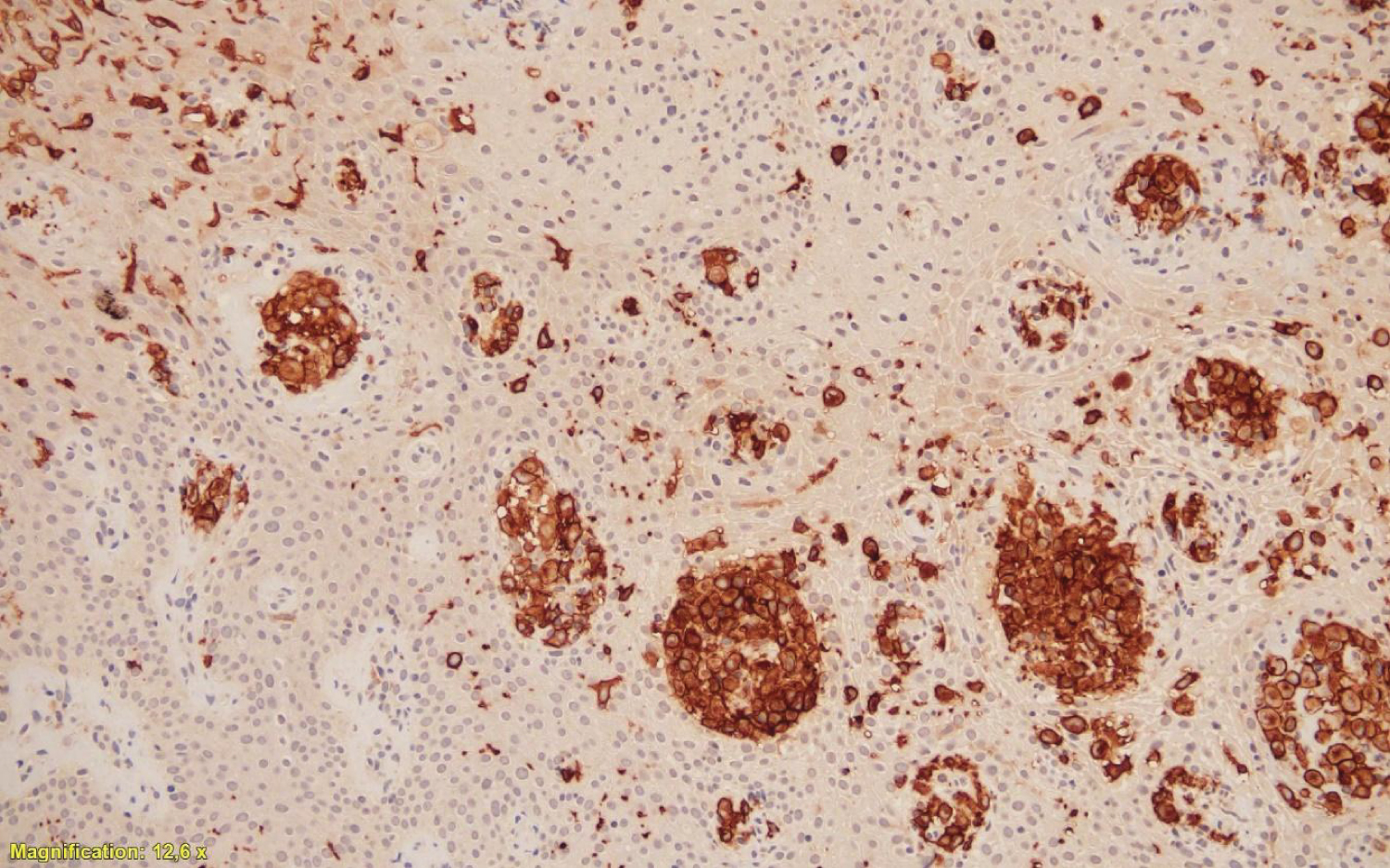 Figure 4: Langerhans cells demonstrating strong positivity to CD68 marker (12, 6 x). (Histopathological findings)
View Figure 4
Figure 4: Langerhans cells demonstrating strong positivity to CD68 marker (12, 6 x). (Histopathological findings)
View Figure 4
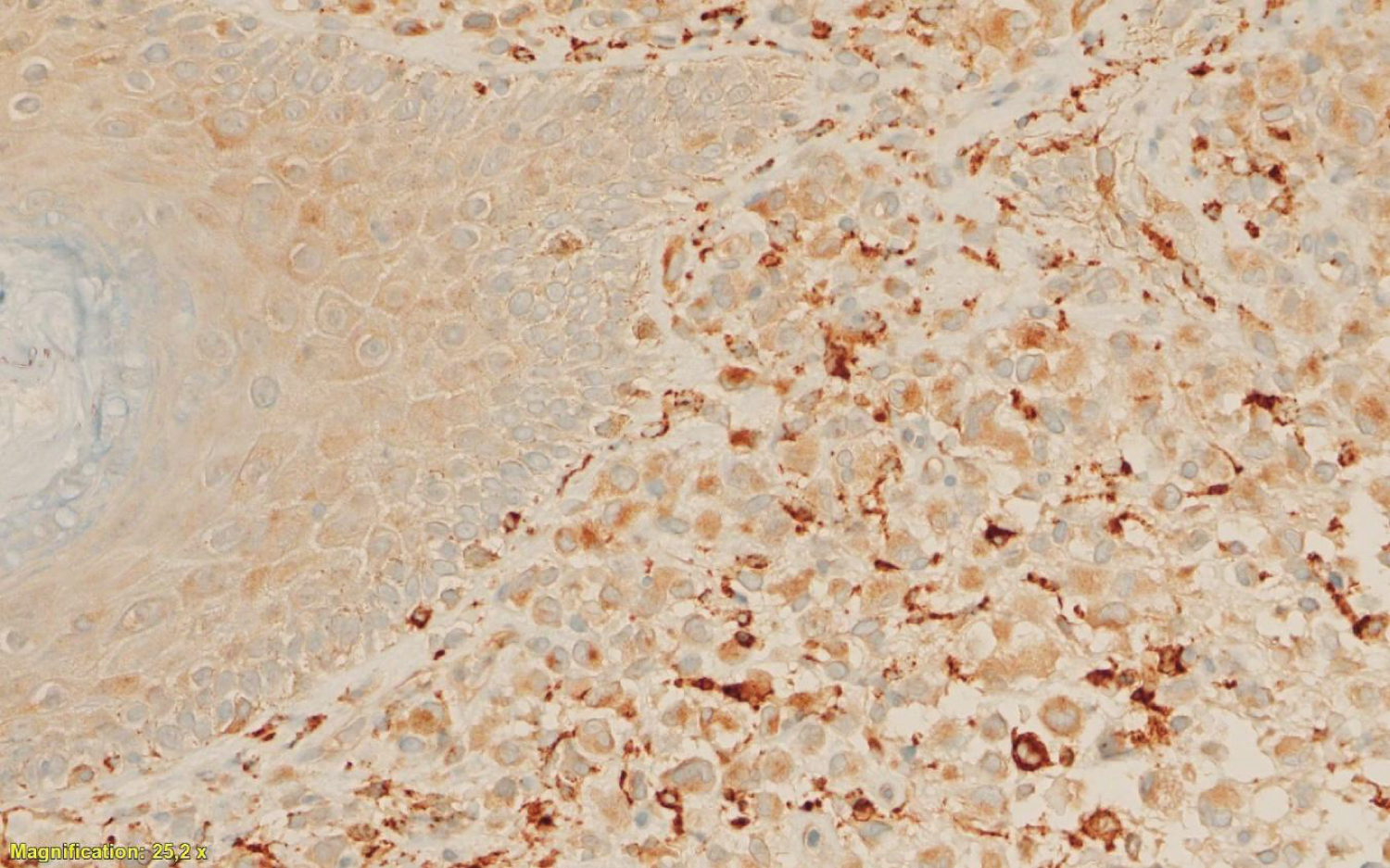 Figure 5: Langerhans cells demonstrating strong positivity to S100 marker (25, 2 x). (Histopathological findings)
View Figure 5
Figure 5: Langerhans cells demonstrating strong positivity to S100 marker (25, 2 x). (Histopathological findings)
View Figure 5
Taking into account the biopsy, diabetes insipidus, and secondary amenorrhea, the diagnosis of Langerhans cell histiocytosis with multisystem involvement were considered. The patient was referred for multidisciplinary management and computed tomography of the abdomen and pelvis was performed to rule out the involvement of other organs. The specialist in hemato oncology considered a multisystem and multifocal Langerhans cell histiocytosis with cerebral, vulvar, ganglionic, cutaneous, hepatic and pulmonary involvement documented by images. Treatment was started with chemotherapy with cytarabine and pegfiligrastin with the disappearance of skin and vulvar lesions.
We have the informed consent provided by the patient
We performed a systematic review of all articles in English or Spanish, published until September 2018, related to the diagnosis and treatment of Langerhans cell histiocytosis in vulva. Two authors (Sandra Marcela Buitrago, Martha Carolina Méndez) independently performed a literature search on MEDLINE, EMBASE, COCHRANE, LILACS and SCIELO databases, with the keywords: "Vulva" AND "Histiocytosis of Langerhans cells'' OR "Vulva" AND "Histiocytosis X". The authors were contacted via email when necessary. The discrepancies were resolved by consensus. The information obtained in the review was organized through a data collection instrument that included the following variables and outcomes: year of publication, study design, age, symptoms, history, morphology of the lesions, histopathological examination, management, follow-up time after treatment and presence of relapse (Flow chart).
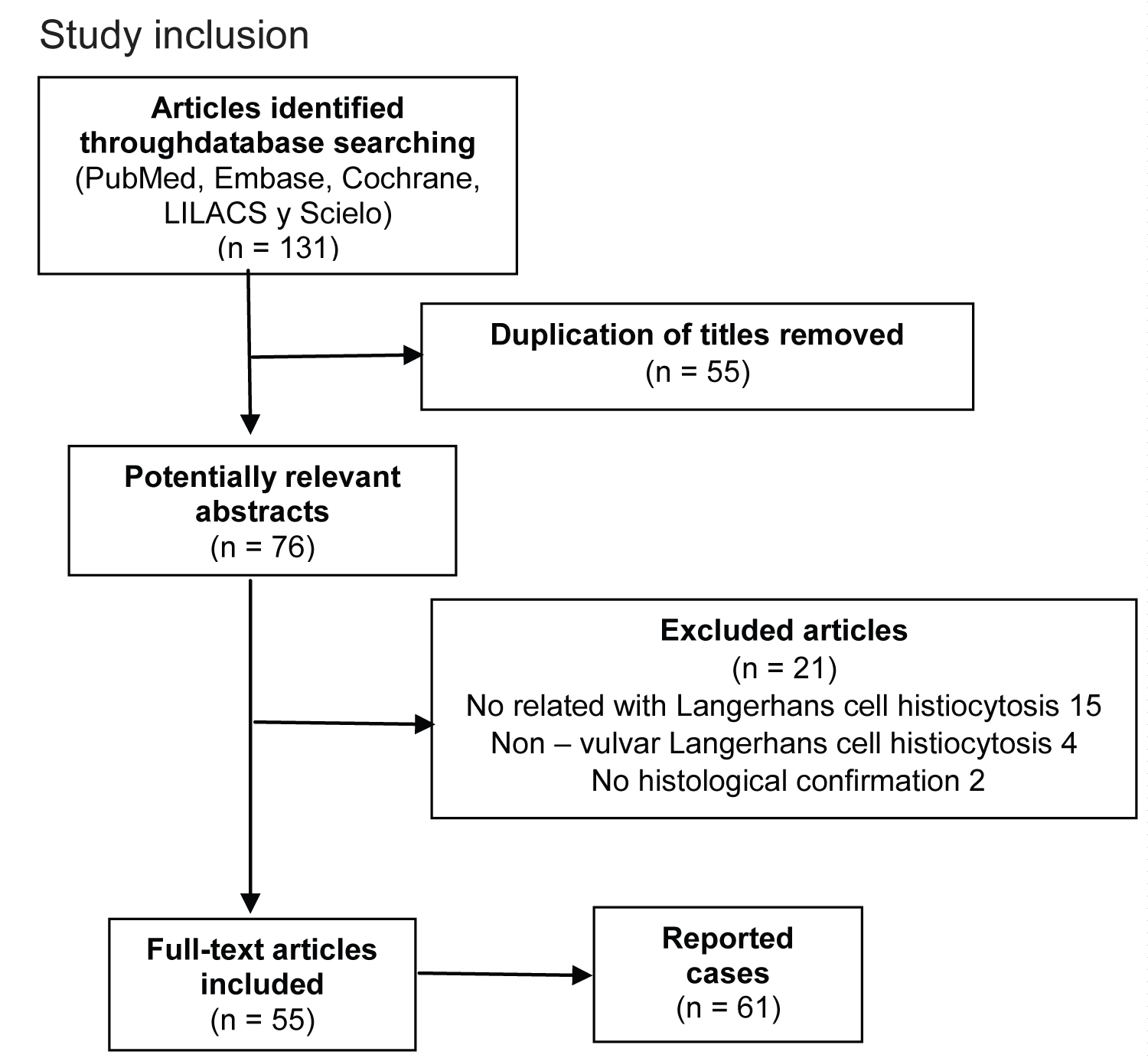 Flowchart of the literature search and the study inclusion.
View Flowchart
Flowchart of the literature search and the study inclusion.
View Flowchart
A total of 164 articles were found, 131 with full text available. We excluded articles that reported cases of non-vulvar Langerhans histiocytosis and that did not have histological confirmation. A total of 55 articles met the eligibility criteria and reported a total of 61 cases.
The largest number of cases has been reported in the United States and the most extensive series of cases were reported by Wieland R. et al and Jiang et al including a total of 3 cases. In Latin America, only four cases have been reported; two in Brazil by Fernández LB et al and Khawali C. et al; and one in Argentina by Ruiz Beguerie J. et al. The demographic, clinical and histological features of reported cases are presented in Table 1A,B.
Table 1A: Demographic, clinical and histological characteristics of patients with Langerhans cell histiocytosis in vulva. View Table 1a
Table 1B: Demographic, clinical and histological characteristics of patients with Langerhans cell histiocytosis in vulva. View Table 1b
In the reported cases, the age of the patients was from 1 to 85 years, with an average of 39 years. The main symptoms reported were pruritus, vulvar pain and dyspareunia; and in patients with pituitary involvement and secondary diabetes insipidus, the main symptoms were polyuria and polydipsia. At the vulvar physical examination, the main findings were papules, nodules, vesicles, ulcers and desquamative erythematous plaques at the labia majora and minora, the interlabial grooves, the clitoris and the perineal region.
As described in the previous section, the immunohistochemically diagnosis of Langerhans cell histiocytosis is made by identifying cells positive for CD1A, CD207 and S-100 and electron microscopic examination with Birbeck granules in the cytoplasm. The majority of reported cases made histological confirmation fulfilling these criteria.
Of the 61 cases reported, 24 (39.3%) also presented systemic involvement. The main organs affected were the pituitary gland (with the subsequent development of diabetes mellitus and amenorrhea), the lung, the bones and the skin.
Due to the fact that Langerhans cell histiocytosis may affect different organs and systems, the clinical manifestations are variable, and the therapeutic approach depends on the affected organs and the extension of that commitment. This is reflected in the multiple treatment regimens reported in the different cases. In patients with isolated vulvar involvement, management included the application of potent topical corticosteroid, local excision, simple or radical vulvectomy, chemotherapy (Vinblastine or Cytarabine), radiotherapy, thalidomide, tacrolimus, methotrexate, clobetasol, interferon or Lenalidomide in different combinations. In the patients with systemic compromise management included chemotherapy (Vinblastine or Vincristine), systemic corticosteroid, thalidomide, chlorodeoxyadenosine, thalidomide, methotrexate and radiotherapy.
In the group of patients with isolated vulvar involvement, 78.3% were followed up (29/37). The follow-up varied between 1.5 and 130 months with an average of 23.7 months. There were 6 relapses (16.2%). Descriptions of findings in the physical exam were not specific, and therefore do not allow to determine any characteristic in the presentation that is associated with a higher risk for relapse. In the group of patients with systemic commitment, 26.0 % were followed up (6/23). The follow-up varied between 6 and 180 months with an average of 54 months. There were 3 relapses (13.04%).
Langerhans cell histiocytosis is a disease that can affect only one organ or several organs and in a multifocal way, this characteristic turns it into a disease of variable presentation and that often can only be diagnosed if an explanation is sought for all the symptoms of the patient. Histologically behaves like a great simulator and this can delay and even confuse the diagnosis, preventing the start of an effective treatment. This disease therefore requires a multidisciplinary approach including specialties such as gynecology, dermatology, endocrinology, neurosurgery and oncology. It is important to provide constant support to the patient because the diagnostic and therapeutic process can be long and frustrating. There is still no scientific evidence of quality that allows the construction of clinical practice guidelines for their management according to each type of presentation. More studies are required to be able to define which treatment achieves the best results in terms of relapse and survival.
The authors would like to thank the Department of Pathology and Cytology of Clínica Colsubsidio el Lago, for making the microscopic tissue analysis.
We know of no conflicts of interest associated with this publication
There has been no financial support for this work that could have influenced its outcome
Sandra Buitrago: Searched the PUBMED, EMBASE, COCHRANE, LILACS and SCIELO databases and organization through a data collection instrument. Writing of the manuscript
Carolina Morante: Writing of the manuscript and critical revision of intellectual content, approval of the final version for publication Laura Hernández: approval of the final version for publication
Martha Mendez: Searched the PUBMED, EMBASE, COCHRANE, LILACS and SCIELO databases and organization through a data collection instrument.