Introduction: Stability in implantology and periodontology can be assessed by both subjective and objective means. As the use of subjective measures can be biased, objective means such as the periotest and Ostell have been developed. However, its application in normal clinical therapy is ineffectual due to the absence of dental reference values. The objective of this study was to provide stability values for natural permanent teeth that could serve as benchmarks in periodontics and implantology.
Methodology: We conducted a cross-sectional study at the Implant and Periodontology Laboratory, FMSB/UY1from December 2021 to May 2022. All students who gave informed consent and had no pathology, history of trauma or dental treatment were included. Three stability measurements were performed at 20 min intervals using a Periotest. A p-value of less than 0.05 was considered significant.
Results: We recruited 120 patients and assessed 3204 teeth. The age group 18-20 years was the most represented. The periotest values of canines, premolars and molars were significantly higher in women (p < 0.001). Also, the stability of maxillary teeth was significantly higher than that of the mandible (p < 0.001). The most stable tooth was the canine (-2.47), followed by the molars (-1.84), premolars (-1.10) and incisors (2.42). With regard to the reproducibility of the periotest, no significant differences were observed between the 3 stability measurements performed.
Conclusion: The stability values of all teeth were within the range of physiological values defined in the literature. The periotest is a reliable and reproducible test.
Natural Tooth, Implant, Mobility, Periotest
Physiologic or normal tooth mobility refers to the limited tooth movement or tooth displacement, that is allowed by the resilience of an intact and healthy periodontium.
Mobility in is generally used as a diagnostic tool for clinical monitoring and follow-up, as well as for the evaluation of a therapeutic outcome in periodontics, prosthetics, implantology and orthodontics [1-4].
More so, as stability is part of the objective of most of our treatments, it is imperative to have a reliable, reproducible and easy to use method to assess it.
Tooth and implant stability can be evaluated by subjective and objective means.
Among subjective methods we have those introduced by Miller [5], Muhlemann [6] and Lindhe. These methods are widely accepted and mainly applied in clinical routine because it is quick and easy to perform however these methods have an inconsistent reproducibility and operator-dependent nature [7].
The use of subjective means can be biased and induce clinical appreciation errors.
Objective assessment of tooth mobility is a necessity.
The periostest and Ostell are some objective means that have been developed. However, their utilization is only difficult because there aren't adapted reference values.
Moreover, these methods are less invasive and less radiating than the subjective methods and radiographs used in periodontics and implantology and could be a complementary method to subjective methods.
By the fact that we do not have an objective, quick, easy to use, regular and reproducible clinical diagnosis method that allows a periodontal and tooth implant therapeutic decision in relation to the natural tooth.
Hence, we carried out this study to have a dental reference value in relation to the application in periodontal and tooth implant therapy.
This study aims at evaluating the stability values of the natural permanent teeth and to analyze the reliability of the Periotest device.
We conducted a descriptive cross-sectional study from December 2021 to May 2022 at the laboratory of implantology and periodontology of the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé I.
The participants were students of the FMSB aged 18 years and above. After sanitation of the oral cavity (scaling and hygiene advice), teeth considered pathological were not included. The pathologies considered were: Carious pathologies, pulpopathies, periapical pathologies, malocclusions, periodontal diseases, previous orthodontic treatments or crowding, endodontic restorations or treatments, signs or history of trauma.
All teeth were evaluated except for the third molars in all quadrants.
Before starting the measurements, we calibrated the device with the test sleeve provided by the manufacturer.
Using an indelible ink marker, the percussion area of the Periotest was marked on the vestibular side and this mark ensured the reproducibility of the percussion area between measurement series.
The measurement cycle consisted of 16 pulses of the pressure sensitive impactor head against the tooth to be evaluated.
After a measurement cycle (approximately 4 seconds) was completed, a short audio signal played. At least 4 of the 16 pulses had to be valid in order to obtain a valid measurement value.
3 readings of Periotest M ® were taken, for each tooth per series with intervals between each measurement. Once the measurement was displayed, the operator recorded it in the patient's collection sheet.
The measurements were collected randomly to eliminate systematic allocation bias.
We carried out our evaluation at a specific time for all our patients to avoid a bias due to the variability of tooth mobility throughout the day.
Data were collected using a questionnaire, was recorded and analysis was performed using SPSS version 23.0 software. Quantitative data were presented as mean and standard deviation and qualitative data as proportions. The significance level was set at 0.05.
The study was approved by the institutional research ethics committee of the Faculty of Medicine and Biomedical Sciences of the University of Yaoundé I (N°112/UY1/FMSB/VDRC/DAASR/CSD). Data collection was carried out anonymously, each data collection form being identified by a 3-digit code. The data were encoded in a database accessible only to the research team. Our study was conducted in accordance with the principles of the Declaration of Helsinki.
Socio-demographic data and Periotest values for each tooth.
Of the 289 patients evaluated for inclusion, 120 constituted our final sample. The main criteria for non-inclusion were hard tissue lesions, refusal to participate and endodontic restorations or treatments.
The Table 1 shows the characteristics of our sample. The sex ratio was 1.1 with a slight male predominance. The mean age was 20.23 +/- 2.22 years with extremes of 18 and 25 years.
Table 1: Socio-demographic characteristics of the study population (N = 120). View Table 1
A total of 3204 teeth were assessed and considered healthy in the 120 patients. The graph shows the distribution according to the type of teeth and jaw. It can be seen that in our sample, maxillary teeth are more represented than mandibular teeth (Figure 1 and Figure 2).
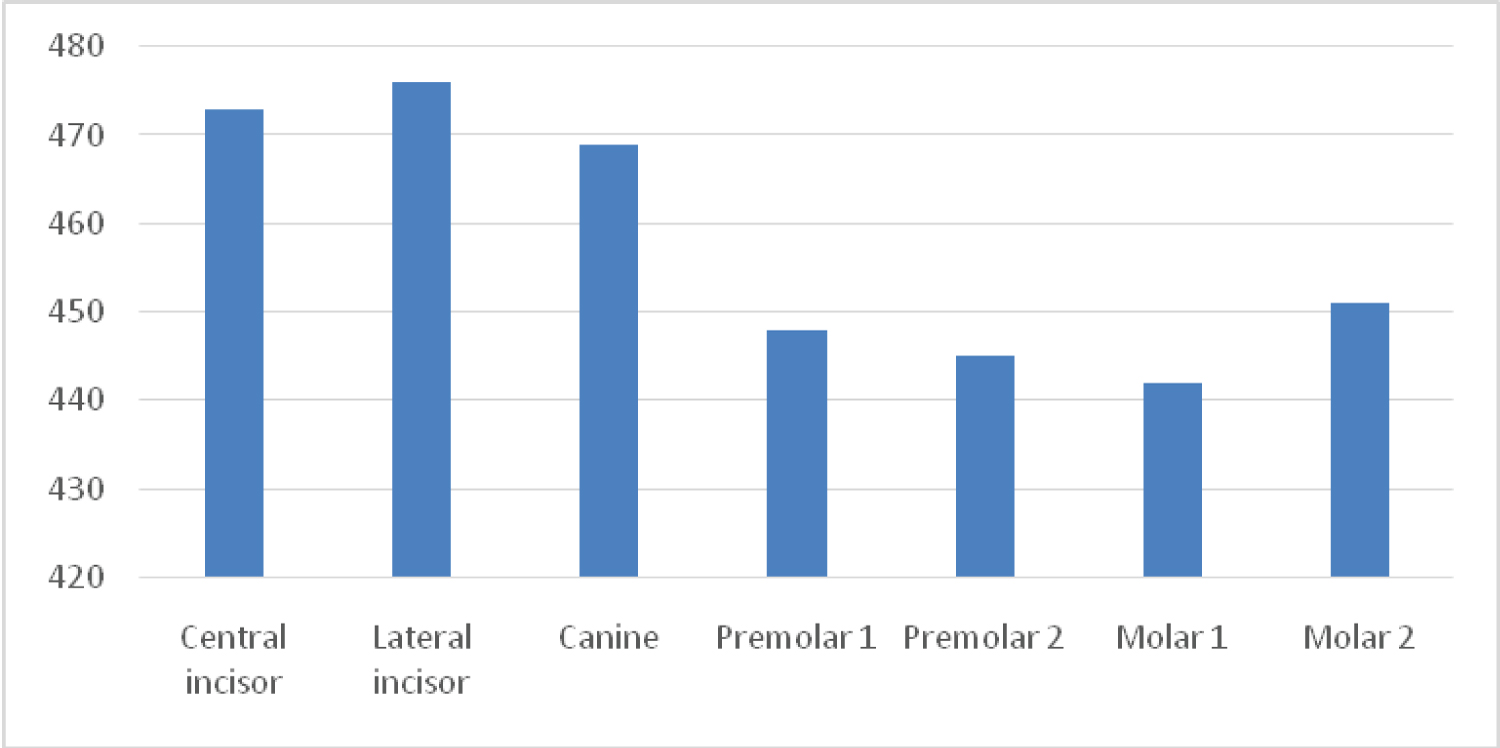 Figure 1: Number Distribution by type of teeth.
View Figure 1
Figure 1: Number Distribution by type of teeth.
View Figure 1
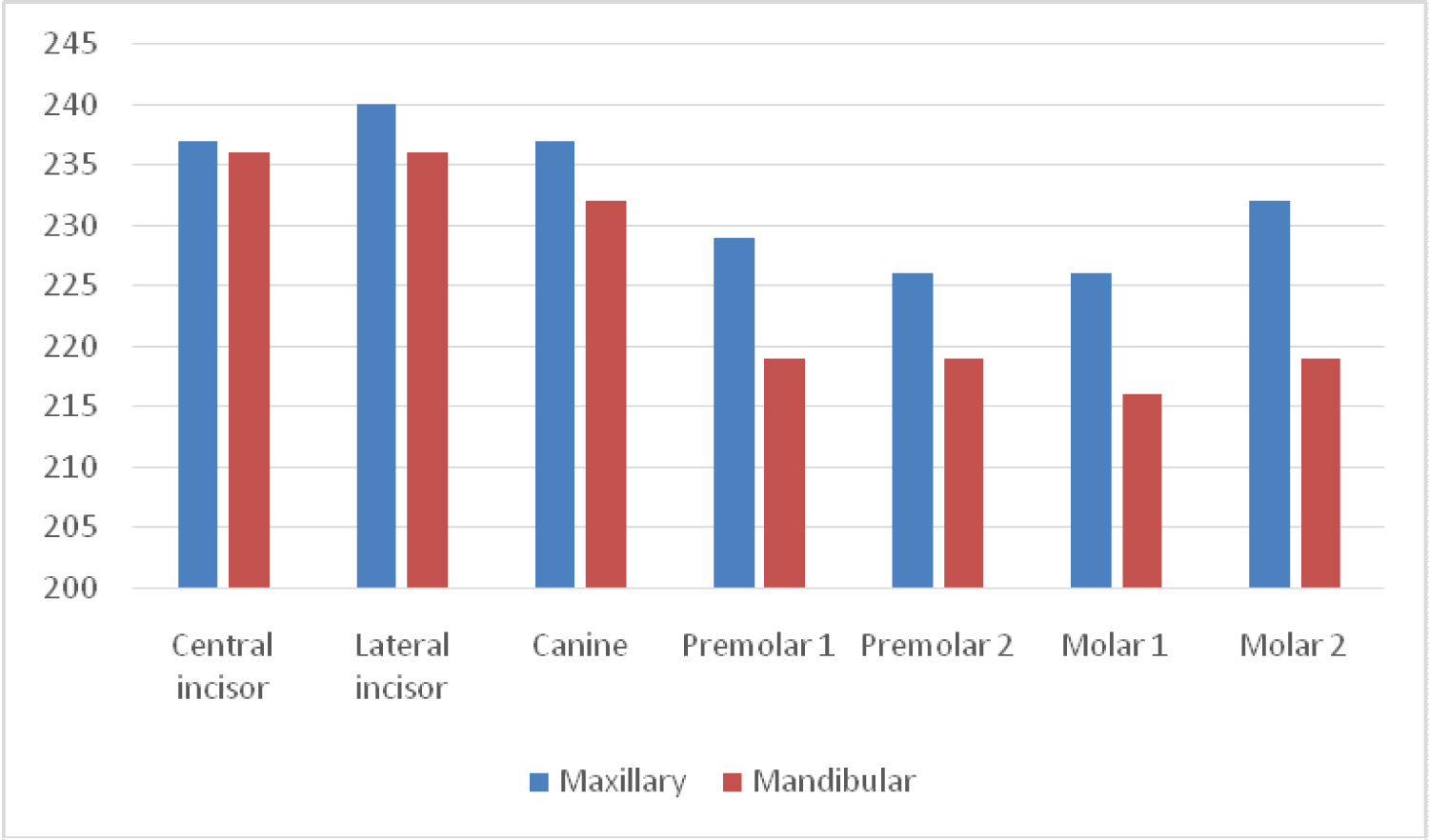 Figure 2: Distribution of numbers of teeth by jaw arch type.
View Figure 2
Figure 2: Distribution of numbers of teeth by jaw arch type.
View Figure 2
Dental stability on the Periotest was -0.19 ± 5.05 for the study population. The mean values found for each tooth were 2.42 for the central incisor, 2.48 for the lateral incisor, -2.47 for the canine, -1.10 for the first bicuspid, -1.11 for the second bicuspid, -1.73 for the first molar and -1.84 for the second molar.
We observed that the stabilities of canines (-2.60 ± 1.25 vs. -2.17 ± 0.99; p = 0.043), and premolars (-1.02 ± 1.89 vs. -0.21 ± 1.97; p = 0.025) were higher in males compared to females. No significant gender differences were found for the other tooth types. Also, no statistically significant differences were observed between the stabilities of the teeth according to age groups.
When comparing dental stability by jaw (Figure 3), we found that the stability of mandibular teeth was higher than that of maxillary teeth for all tooth types except for the central incisor and the first premolar.
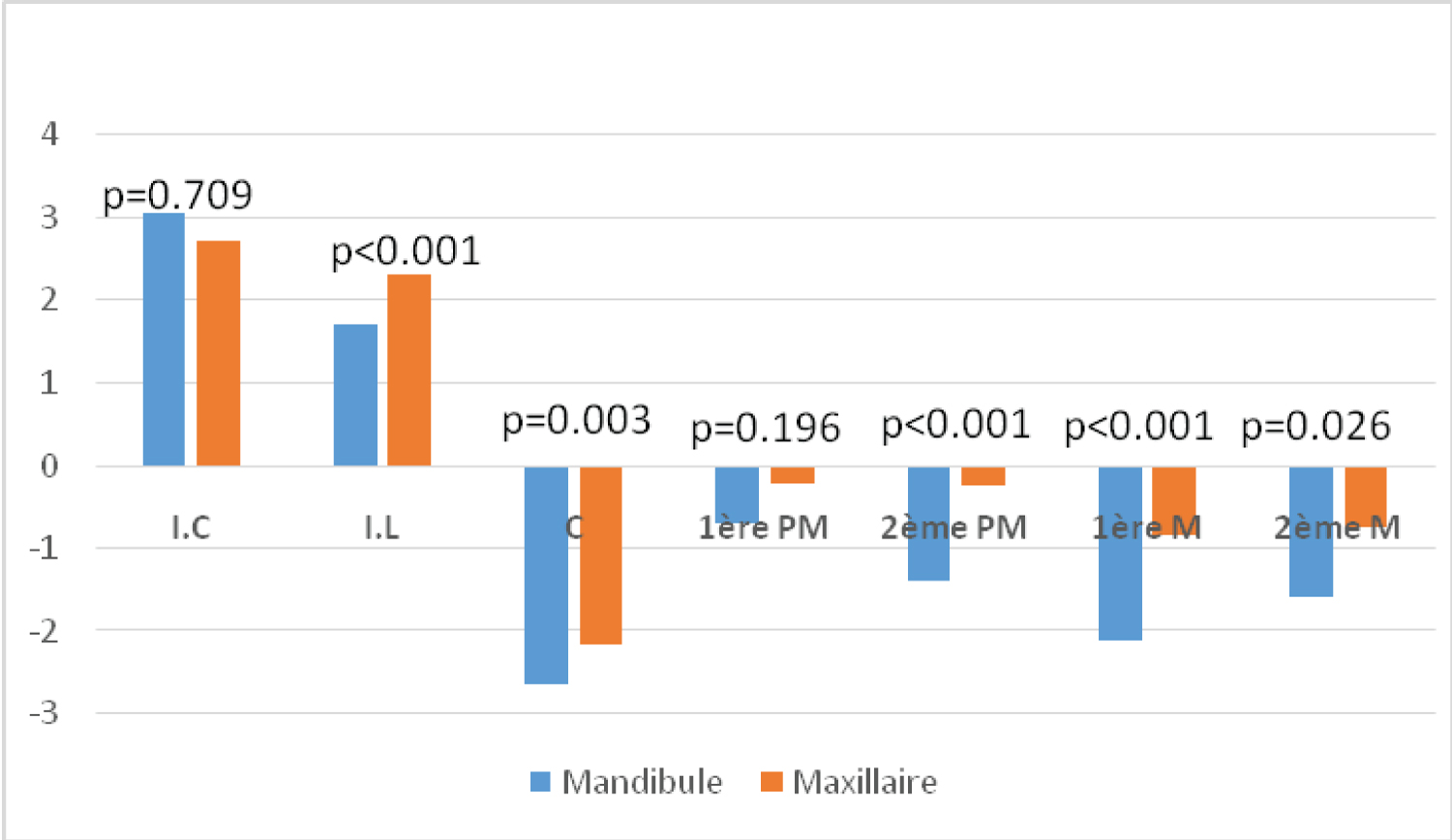 Figure 3: Comparison of dental stabilities by jaw.
View Figure 3
Figure 3: Comparison of dental stabilities by jaw.
View Figure 3
For each patient in the study, three periotest measurements were taken. We then assessed the reproducibility of the periotest measurements. No significant differences were observed between the means of the three measurements, except for those of teeth 17 and 25 as shown in the Table 2.
Table 2: Periotest measurements. View Table 2
We conducted a cross-sectional study to assess the stability of natural teeth and the reproducibility of the measurements made by the periotest. We found good average stability in the population, with better stability for canines, molars and premolars. Also the reproducibility of the periotest measurements was satisfactory.
The overall mean stability of the study population (𝑃𝑇𝑉 = -0.19) was higher than that reported in the US study by Winkler, et al. (𝑃𝑇𝑉 = +1.8) [8]. This could be explained by differences in bone density, which is higher in melanodermal subjects than in Caucasians [9], by the greater mesio-distal dimensions of African subjects compared to Caucasians [10], and by the dietary habits of African subjects, which are based on a more solid diet.
We found no significant difference in Periotest values by gender for all tooth types except for central and lateral incisors. This result differs slightly from the study by Schulte, et al. who found that all teeth except the central incisors were more stable in men [3]. This could be explained by the absence of sexual dimorphism in these teeth, which are characterized by similar mesio-distal and coronal-radicular dimensions [11].
When comparing the stability of natural teeth by age, no differences were found. This result contrasts with the results of Andresen, et al., who observed that Periotest values varied with age in patients aged between 8 and 12 years [1]. Also, Chakaprani, et al. in 2015, Showed in their study that the teeth of pubertal subjects (11-14 years) are more mobile than those of adolescents (8-13 years) [12]. These results can be explained by the fact that root development, characterized by the attachment of a progressively high number of periodontal fibres to the root and alveolar bone, is already completed after 18 years of age [1,13].
In the present study, the stability of mandibular teeth was higher than that of maxillary teeth. These results are in agreement with those of Schulte, et al. [11] and Winkler, et al. [14], who reported that mandibular teeth have lower Periotest values than maxillary teeth.
For our study population, the tooth types with the best stability were the canine, followed by the molars, the premolars and finally the incisors. This result is in line with the study by Hwang, et al. who found the same order of teeth for stability values [2]. However, it differs from Schulte, et al. who showed that the molars had the best stability, followed by the canines, then the premolars and finally the incisors [3]. The better stability of the canine could be explained by its large total root surface and its long coronal-radicular length. Furthermore, the leverage effect resulting from its crown-root ratio to the root is responsible for the lower Periotest values [15].
The study of the reproducibility of the measurements revealed a very high reproducibility of Periotest for all teeth except 25 and 17. Similar results were found by authors such as Schulte, et al. [3, 11] and Chakrapani, et al. [12]. The intrinsic characteristics of the Periotest device and the marking of the measurement points could explain this high reproducibility. Also, the fact that all measurements are performed by the same experienced operator reduces inter-examiner variability, thus improving reproducibility. However, Andresen, et al. and de Mackie, et al. [13] found significant differences between the first and second readings. The discrepancy between these results highlights the need for further, larger studies to assess the reproducibility of the Periotest. The poor reproducibility of measurements for teeth 25 and 17 could be partly explained by the more convex surface of these teeth compared to the almost flat surface of teeth such as incisors, which complicates the measurement of Periotest.
These results could help guide the position of the implant in different zones, at bone level, by comparing them to the values with natural teeth.
A multi-centric study would have been better because of the variability in diets around the world that will allow us to have a cut-off value.
Proposing a consensus in periodontology and dental implantology based on tooth mobility evaluation for therapeutic purposes as it is easy to use and didactic is plausible (Annexes).
In our study population, the stability of the teeth was generally good. The stability of the mandibular teeth was higher than that of the maxillary teeth and the canine was the most stable tooth. The Periotest measuring device has a satisfactory reproducibility for the measurement of tooth stability.
None.
All the patients who participated in this study gave consent.
None.