Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) infection continues to prevail as the deadliest epidemic of the 21st century and an unprecedented global crisis. Global statistics as of July 2021 revealed that, more than 196 million people worldwide have been infected and more than 4.19 million people have succumbed to the SARS-CoV-2. In Trinidad and Tobago there has been approximately 38,000 confirmed Covid-19 cases in which 1,056 resulted in death; with no study being done on prevalence on ethnic background, age or gender as of July, 2021 [1,2].
Although the average incubation period is 3 to 9 days which sometimes ranges 24 days, transmission of the virus can occur before a person becomes symptomatic, and approximately 18% of cases remain asymptomatic. Apart from fever, dry cough, fatigue, dyspnea, and loss of appetite being the most common symptoms experienced by those who were diagnosed with SARS-CoV-2, numerous studies have also reported a wide range of neurological dysfunctions, including mild symptoms such as headaches and gastrointestinal disturbances to serious complications such as strokes and encephalitis. Despite numerous reports of neurological associations and complications of COVID19 in the face of a pandemic raging with limited resources, there is still a significant lack of control over causative factors. Significant confounding factors include the severity of the systemic disease, exacerbation or recurrence of pre-existing neurological disorders and drug-induced complications and hospital conditions. In addition, given the prevalence and variants of the virus, analysing COVID19-related complications from coexisting conditions is difficult [3]. In this case report it discusses the initial visit of Patient X to the University of the West Indies Optometry Clinic on the 29-03-2021 before the Patient contracted SARS-CoV-2 and the clinical findings and observations of Patient X after being infected with the virus as well as receiving his initial first dose of Oxford Astrazeneca. The intended audiences for this report are students, residents, and clinicians in all aspects of the medical disciplines.
Patient X, a 35-year-old man of East-Indian descent with no underlying systemic medical conditions came into the University of the West Indies (UWI) Optometry clinic in late March, 2021 for a glaucoma workup; as there is a maternal link in his family. A full panel glaucoma assessment was done, which included Tonometry, Pachymetry, Visual Field Testing 24-2 (Humphery VFT), Dilated Optical Coherence Tomography Imaging (Optic Nerve, Ganglion Cell Layer GCL and Retinal Nerve Fibre Layer RNFL). All tests done on Patient X in March 2021 showed no abnormalities or defects. In April 2021, Patient X had flu like symptoms accompanied by a throbbing, intense headache to the occipital portion of his head which subsided in a couple (3-4) days. With no flu like symptoms and headaches, Patient X proceeded to get his first dose of his Covid-19 Vaccine (Oxford AstraZeneca). After receiving his first ‘jab’ he was notified by his company that there has been a Covid-19 outbreak in his office; and that every staff member should proceed to do a polymerase chain reaction (PCR) test. After doing the mandatory PCR testing, he was declared Covid-19 Positive. During his quarantine period at home, he reported severe throbbing headaches, dreadful chest pains and intermittent blurry vision. His conditions and complaints worsened with time to the extent where he had to be placed temporarily in a Public Hospital with a CoVid-19 facility in Trinidad. After doing 4 PCR tests, the results came back negative in June 2021. Though being cleared from the virus, his headache was still there accompanied by intermittent chest pains and blurry vision. After seeking help from a General Public Hospital, he was referred to a Private Ophthalmologist for testing as at that moment in time the UWI Optometry Clinic was closed due to a nation-wide lockdown. However, once re-opened, Patient X reached out to the Authors for assessment. On the follow-up visit, it was found that an abnormal presentation of a left homonymous hemianopsia was found and the patient was referred urgently to Neurology that detected no abnormalities on MRI, MRA and CT scans. Currently the patient is under palliative care by a Private Neurologist (Figure 1, Figure 2, Figure 3, Figure 4 and Figure 5).
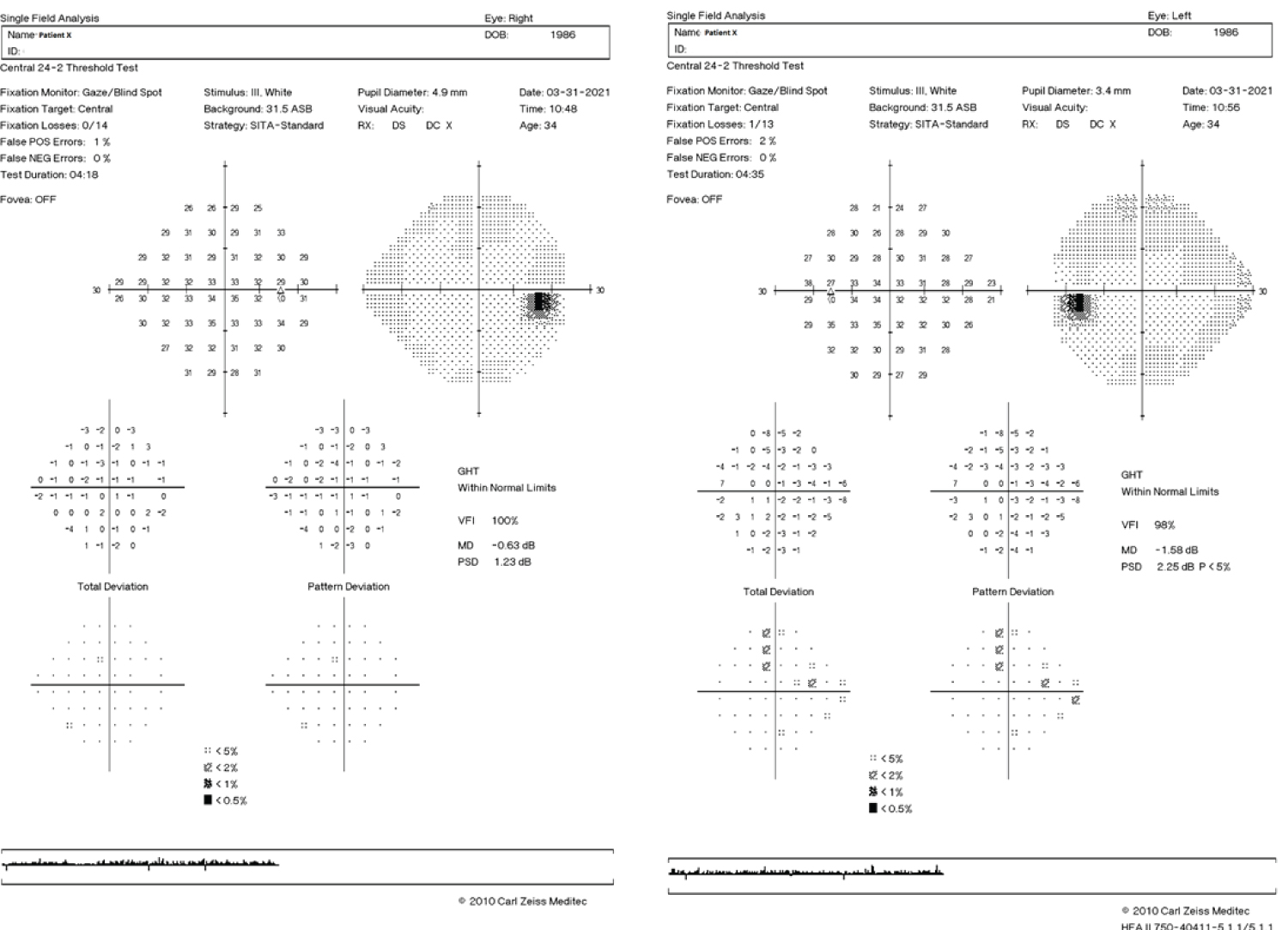 Figure 1: Humphery Visual Field Test 24-2: OU Report, March 2021.
View Figure 1
Figure 1: Humphery Visual Field Test 24-2: OU Report, March 2021.
View Figure 1
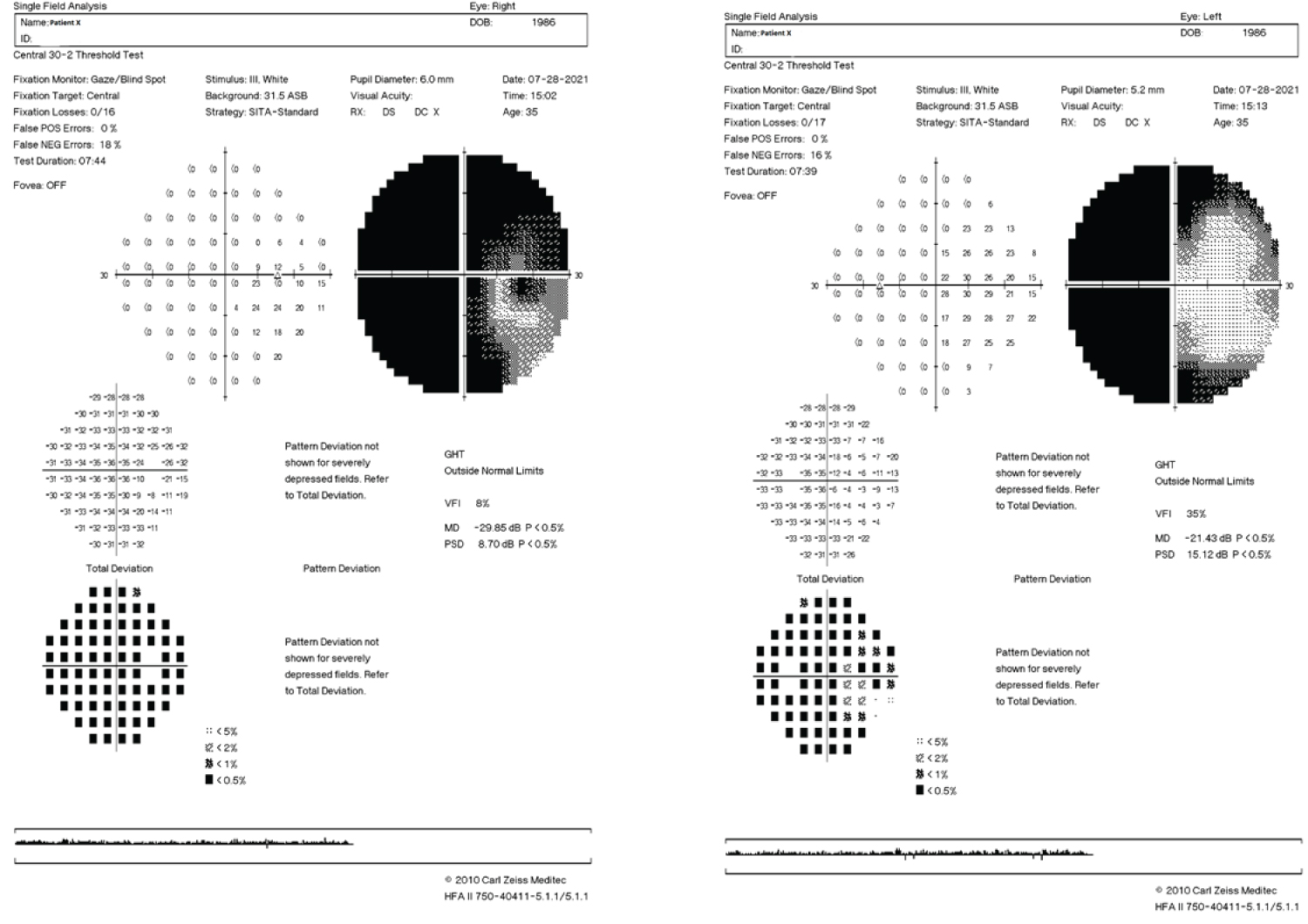 Figure 2: Humphrey Visual Field Test 30-2: OU Report, July 2021.
View Figure 2
Figure 2: Humphrey Visual Field Test 30-2: OU Report, July 2021.
View Figure 2
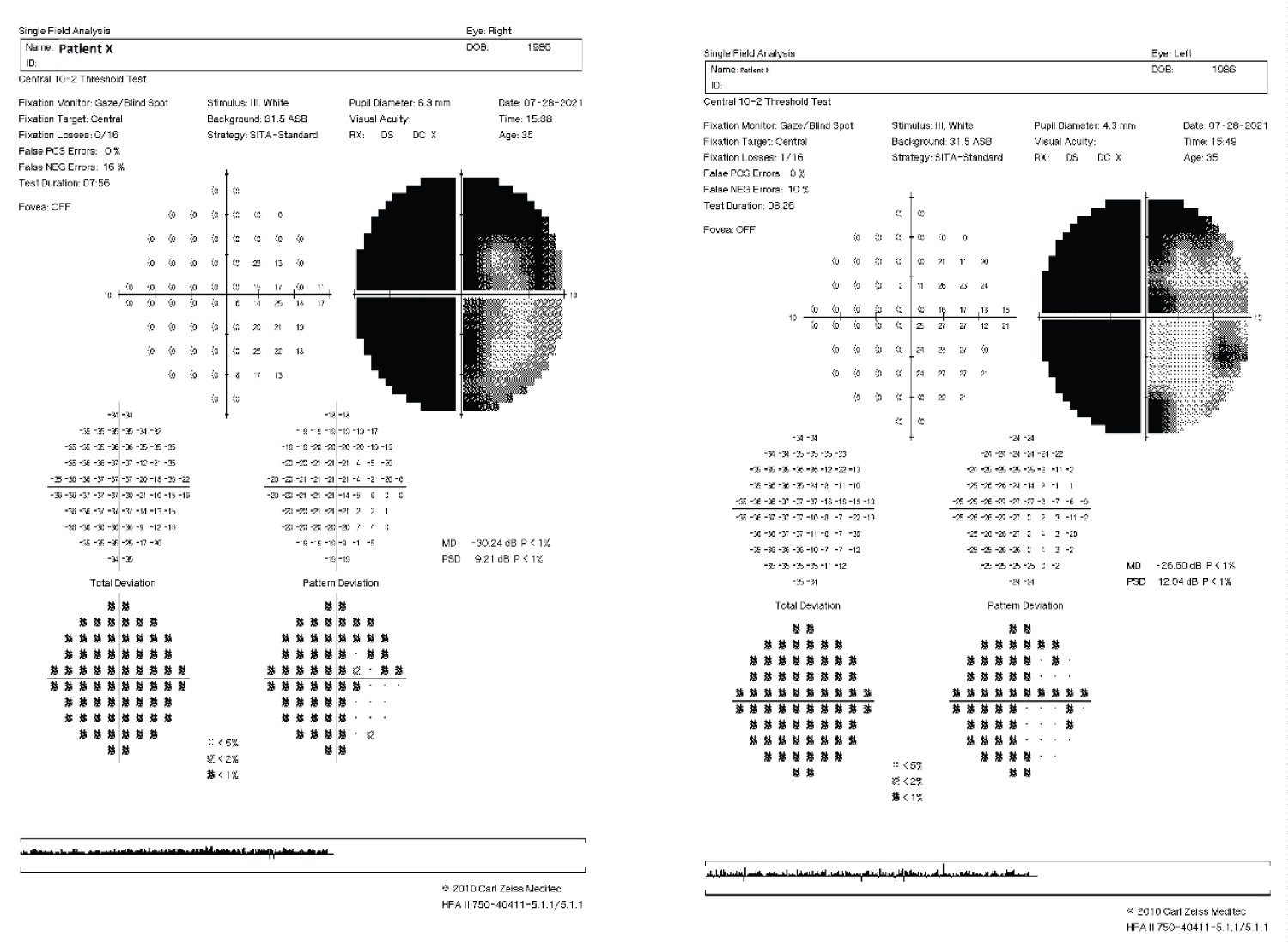 Figure 3: Humphrey Visual Field Test 10-2: OU Report, July 2021.
View Figure 3
Figure 3: Humphrey Visual Field Test 10-2: OU Report, July 2021.
View Figure 3
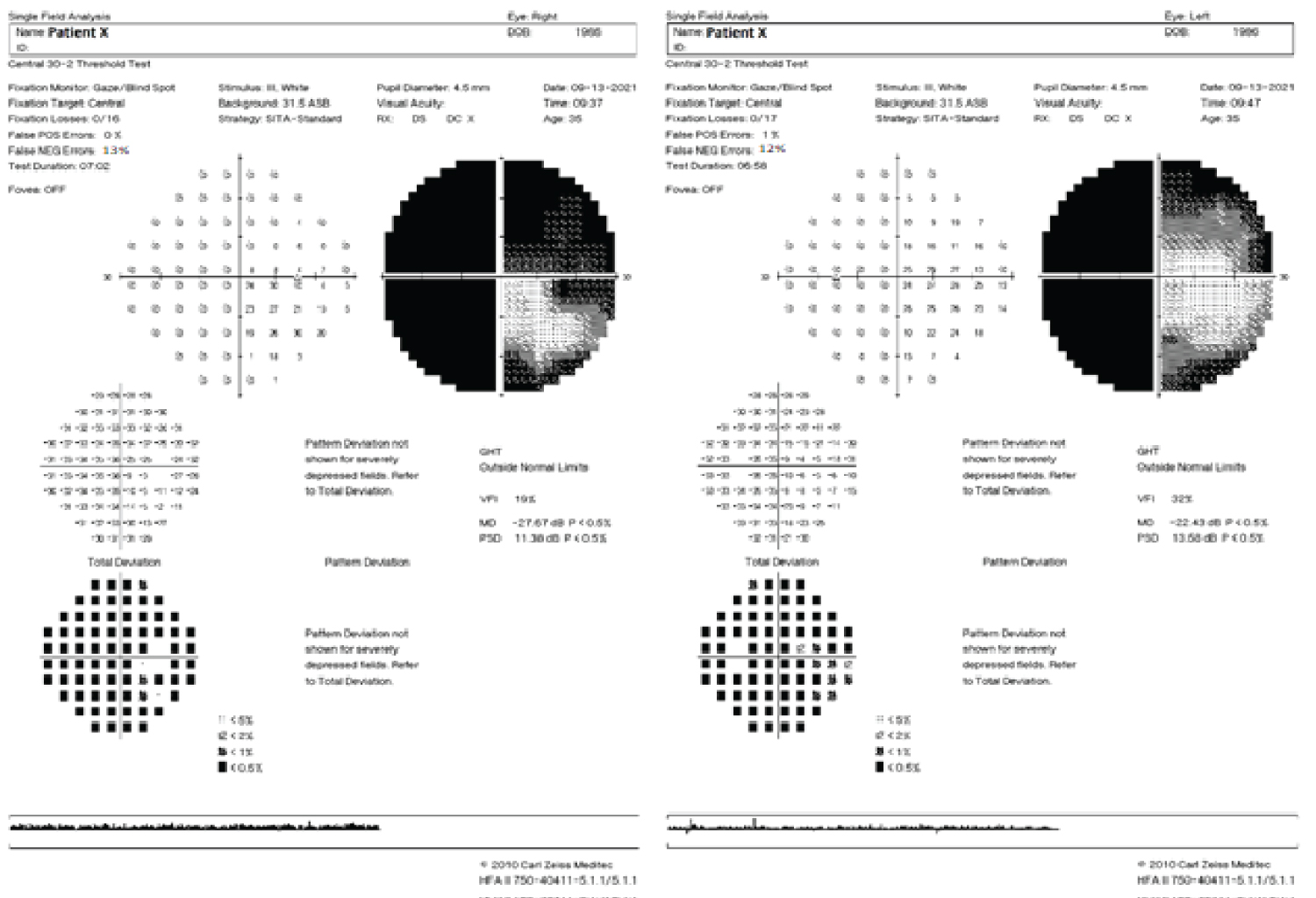 Figure 4: 24-2 Humphrey Visual Field Test: OU Report, September 2021.
View Figure 4
Figure 4: 24-2 Humphrey Visual Field Test: OU Report, September 2021.
View Figure 4
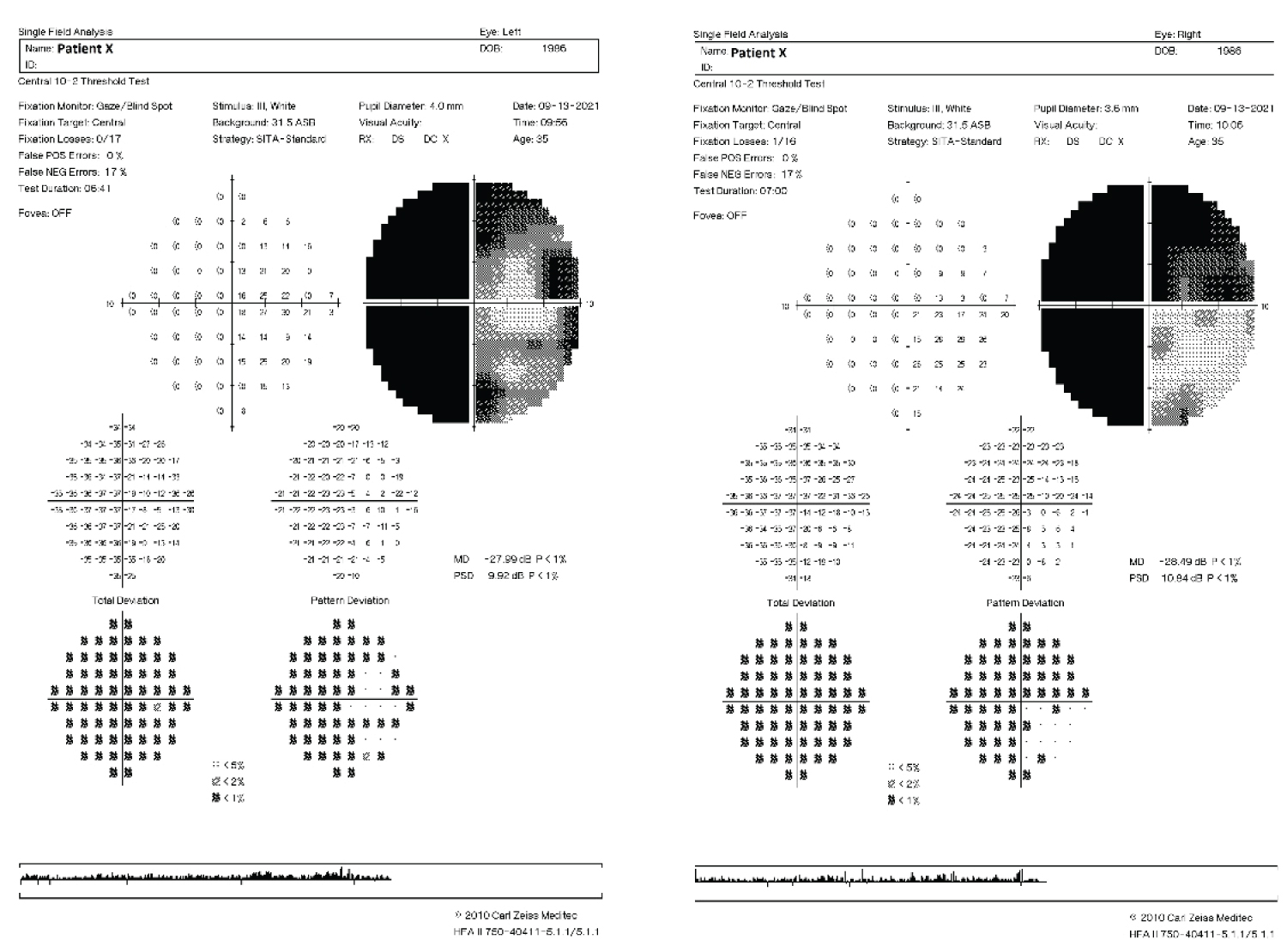 Figure 5: 10-2 Humphrey Visual Field Test: OU Report, September 2021.
View Figure 5
Figure 5: 10-2 Humphrey Visual Field Test: OU Report, September 2021.
View Figure 5
Vision was reduced in both eyes, in comparison to initial visit in March, 2021. Presenting Right Eye scored 20/118 and Left Eye 20/80 on a Snellen chart located 20ft away from patient. Using a near Snellen chart, at 40 cm; intermittent diplopia was recorded with a score of 20/100.
Cover Test- No movement found at distance or nearby.
Patient X became severely light sensitive, and Refraction could not have been achieved. Auto-Refraction was conducted, however the computed calculated Rx given did not affect the patients’ quality of vision.
No abnormalities were observed on anterior or posterior eye; with slit lamp bio microscopy and OCT images.
Clinical Tests and Observations:
Colour Vision: Tritan Colour Vision Defect
Stereopsis: 300’’
Visual Acuity Distance: OD 20/118
OS 20/80
Cover-Test: No Movement found at distance or near
Maddox Rod: No Deviation
Headaches and recent Hair-Loss in Mid scalp region.
Based on the clinical onset, symptoms and observation the possible differential diagnoses are: Cerebral Venous Thrombosis, Multiple Sclerosis, Neuromyelitis Optica Spectrum Disorder, Primary Angitis of the CNS (PACNS).
Cerebral venous thrombosis (CVT): Cerebral vein thrombosis has been found to have a high degree of variability. With an acute, subacute, or chronic onset, CVT most often presents with new headache or as a syndrome of isolated intracranial hypertension. Additional manifestations include focal neurologic deficits, seizures, and/or encephalopathy [3].
In a review of 34,331 patients hospitalized with SARS-CoV-2 infection, the frequency of CVT was 0.08 percent. Rare reports describe thromboembolism including CVT associated with thrombocytopenia among patients immunized with the adenovirus-vector ChAdOx1nCov-19 (AstraZeneca COVID-19) and Ad26.COV2.S (Janssen COVID-19) vaccines. These cases of CVT have typically occurred in patients who are between 5 and 30 days post-vaccination. Inflammatory diseases can also cause CVT, including systemic lupus erythematosus, Behcet disease, granulomatosis with polyangiitis, thromboangiitis obliterans, inflammatory bowel disease, and sarcoidosis.
Neuromyelitis optica spectrum disorder: (NMOSD, formerly known as Devic's disease or Neuromyelitis optica [NMO]) Considered to be a group of inflammatory diseases of the Central Nervous System, CNS Neuromyelitis Optic Spectrum Disorders is characterized by the immune-mediated demyelination and axonal damage, primarily affecting the optic nerves as well as the spinal cord [4].
Signs and symptoms: Transverse myelitis often causes limb weakness, loss of sensation, and bladder dysfunction, with additional bilateral acute attacks or rapidly sequential optic neuritis which tends to lead to severe vision loss. The onset of seizures generally occur over a period of a few days, with varying degrees of recovery times; weeks or months [4,5].
Primary angitis of the CNS (PACNS): PACNS is the preferred term for vasculitis that is limited to the CNS. CNS vasculitis is considered secondary if it transpires in association with a systemic inflammatory disease such as systemic lupus erythematosus (SLE) or systemic vasculitis or even through an infectious process such as varicella zoster virus. PACNS mainly affects the small and medium arteries of the brain parenchyma, the spinal cord, and the leptomeninges, causing symptoms and signs of CNS dysfunction. Although there is no characteristic representation of PACNS, there are some scenarios that are very suspicious. PACNS should be suspected if stroke occurs more frequently in young patients without identifiable hypercoagulable or cardiovascular risk factors; in the development of cognitive dysfunction with or without headache; and for recurrent or persistent focal neurologic symptoms, abnormal cerebrovascular imaging associated with unexplained neurologic deficit or spinal cord dysfunction unrelated to systemic disease or other process [5].
Multiple sclerosis (MS): Considered to be the most frequent immune-mediated pattern, the central phenotypes of MS are those of progressive and relapsing-remitting disease. There are several clinical subtypes of MS. Clinically Isolated Syndrome, which represents the first outbreak of MS, Relapsing-remitting MS, Primary progressive MS and Secondary progressive MS [6]. In addition, these phenotypes are identified by assessing modified disease activity and disease progression over time. The activity of disease is determined by clinical relapse or radiological investigations of contrast-enhancing lesions and or new or clearly enlarged lesions on T2-weighted images. MS has no distinct clinical findings; however some common characteristics of the disease exists.
Common symptoms often include loss of sensation in the extremities or half of the face, unilateral loss of vision, acute or subacute motor weakness, diplopia, gait disturbances and balance problems, sensations similar to electric shocks that occur when the neck is bent. Presenting symptoms and signs can be consistent with a single lesion, monosymptomatic or polysymptomatic which is consistent with more than one lesion. Presentations due to cortical syndromes such as aphasia or visual field disorders are possible, but rare. These presentations are most likely associated with a large area of inflammation known as swelling MS due to its tendency to mimic neoplasms both clinically and radiologically [7].
Patient X, initially presented to the UWI Optometry Clinic for a glaucoma workup in March, 2021 with no ocular complaints. At this visit, a full panel glaucoma was done which ranged from Intraocular pressure, Central Corneal Thickness, Visual Field Testing as well as OCT imaging; with no significant or glaucomatous changes being observed. His presenting Visual Acuity was recorded to be 20/20 monocularly and binocularly. With no abnormalities being detected on the posterior eye and only dry eyes being detected on the anterior eye: Patient X was advised to use a lubricating eye ointment as well as to practice the 20-20-20 rule (Table 1).
Table 1: Pertinent details of Patient X. View Table 1
Shortly after visit, he was diagnosed with Covid-19; which was only confirmed after receiving his first dose of the Oxford-AstraZeneca vaccine. Being diagnosed with Covid-19 for approximately 2 months; with no hospitalization Patient X complains of headaches 3 months after Covid-19, myalgia and intermittent double vision which occurs monocularly and binocularly. Seen on an unscheduled follow-up at the UWI Optometry clinic it was seen that his visual field revealed an incongourous homonymous hemianopsia, which did not respect the vertical or horizontal midlines. Upon further evaluation, it was found that his vision dropped to 20/100 at distance peered with diplopia at near with there being no involvement of the Optic Nerve (No Relative Afferent Pupillary Defect) see Table A3 in the Appendix to view other preliminary tests conducted on Patient X, July 2021. OCT Imaging as well as Slit Lamp Bio-microscopy showed no retinal abnormalities. The SARS-CoV-2 virus which is the seventh known variant of the coronavirus that has been proven to infect humans, on a global scale. According to a study done Wu, et al. in 2003 results yielded that SARSCoV1; which infected about 8,000 patients found that they had very few neurological implications; mainly peripheral neuropathy and encephalitis [7,8]. Like SARS-CoV-1, current SARS-CoV-2 has been proven to have an impact on the neurological system in approximately 36.7% of patients, as stated by Mao, et al. Most coronaviruses are neurotrophic and other studies also theorize that SARS-CoV-2 is also neurotrophic [9]. It was also discovered that SARS-CoV-2 can be recognised in cerebrospinal fluid (CSF) by PCR testing. The main portal of entry for SARS-CoV-2 and other coronaviruses has been found to be that of the Angiotensin converting enzyme 2 (ACE) [7]. Although ACE2 receptors are present in the nervous system, alternative routes have been proposed to explain SARS-CoV-2 entry into the nervous system, including direct violation of the blood-brain, hypoxic injury, and immune-related injury [10].
However, in Patient X, the CSF was found to be 17 cmH2O along with having a D-Dimer value of 0.369, which are considered to be within the normal ranges. Patient X, was also cleared from Cardiology as no abnormalities were seen on a cardio reports. Haematology reports and results can be viewed in Tables A4-A5 in the Appendix section; which were obtained after PCR testing declared Patient; Negative from Covid-19. Additionally, in a study conducted by Chou, et al., at the University of Pittsburgh School of Medicine with 3,744 patients diagnosed with SARS-CoV-2 eighty two percent of the patients self-reported or had clinical features of neurological symptoms. From that group of patients, 4 out of 10 patients reported headaches along with 3 out of 10 self-reported their loss of smell and taste. Acute Encelopathy was the most commonly diagnosed, which affected approximately 50% of the sample size, followed by coma (17%) which was followed by strokes (6%) [1].
In the European Academy of Neurology Neuro-COVID Registry (ENERGY) study, which analysed three different cohorts; which included 3,055 Covid-19 patients irrrespestive of their neurological status, 475 Covid-19 Patients with confirmed neurological symptoms, and the ENERGY cohort which comprised of 214 patients hospitalized with Covid-19 who required the need for a neurological consult. This study concluded that any patient having any latent underlying neurological condition is more likely to have precipitating neurological findings after being diagnosed with Covid-19, by a two-fold. According to the study, neurological conditions could vary from abnormalities in the brain, spinal cord, Alzheimer and nerve disease just to name a few [11].
However, researchers at the Nottingham University Hospitals NHS Trust, UK, reported neurological syndrome was previously found to be a complication of Covid-19. The researchers indicated that if the link between these neurological events and the Oxford-AstraZeneca vaccine is causal, it is more than likely due to a cross-reactive immune response to the SARS-CoV-2 spike protein and components of the peripheral immune system. With rare outcomes of this, approximately 5.8 per million, the researchers indicated that the benefits of vaccination substantially outweighs the risk of this relatively rare outcome as well as the researchers warned that clinicians must be alert to this possible adverse event. They must definitely look for this rare neurological manifestation after administration of COVID-19 vaccines [12,13].
Patient X, as indicated is currently under the palliative care of a private Specialist Neurologist; where his initial treatment started off with dexamethasone at a dose of 6 mg and amitriptyline 25g orally for 2 weeks. On his follow-up visit, he was given Apo amitriptyline 20 mg along with amitriptyline 25g for 12 days. The patient’s initial complaints of headaches with blurred vision after being cleared from long Covid-19, promoted the urgent need for a multi-interdisciplinary team to provide the best care for the patient. Not only was the optometrist involved as the primary health care professional, but also the neurologist, radiologist and vascular surgeon [14,15].
Due to the clinical timeline of this report, the authors would like further studies to be urgently done for a comprehensive understanding of the neurological pathophysiology of COVID-19 and the possible consequences it poses to the visual system. This case reports do not aim to deter the general public from acquiring a vaccine for SARS-CoV-2.
The patient is still under the care of Neurology; however, the researchers found this report necessary for public knowledge as it contains crucial information for multiple medical disciplines.