To determine whether a normal visual field assessment at a referring optometric practice is predictive of a normal visual field assessment at the hospital eye service and therefore whether there is any need to repeat it prior to first hospital visit.
Between 1st January 2018 and 1st December 2018 all patients referred into Loughborough Community Hospital with a suspected diagnosis of glaucoma or ocular hypertension were booked for a visual field assessment prior to their initial new patient outpatient attendance. If the visual field test at the optician was documented as being "normal", "within normal limits", "no abnormality detected", or "OK" on the referral letter then the patient was included in the study population. These patients underwent a visual field assessment with a Humphrey's visual field analyser on a 24-2 SITA standard protocol. The outcome of the visual field test was documented including patient age, reliability indices, Mean Deviation and Pattern Standard Deviation. This data was statistically analysed by one of the authors.
Data on visual fields of 501 consecutive patients, 1002 eyes/visual field assessments were collected. The positive predictive value of a normal visual field at the patients referring optometrist was 97% for the right eye and 98% for the left eye. From all the visual field assessments the rate of a visual field where the glaucoma hemifield test (GHT) was outside normal limits (ONL) was 16% for the right eye and 7% for the left eye. There was very little observed association between the referral diagnosis, the IOP at referral, age of patient or the sex of the patient on the likelihood of having an abnormal visual field.
Our data suggests that, in the presence of a normal visual field assessment at the referring optometry practice, there is very little yield of positive findings when the visual field test is repeated prior to clinical assessment. Visual field tests should instead be targeted at those patients with an abnormal visual field test on referral and those with a clinical indication for the test.
Visual fields, Perimetry, Humphreys, Glaucoma, Ocular hypertension
The burden of glaucoma and ocular hypertension is ever increasing and Hospital Eye Services (HES) [1] in the UK are creaking under the burden. In a recent Looking Forward publication by the UKs Royal College of Ophthalmologists it was projected that by 2035, the number of people in the UK with glaucoma will rise by 44%. We are faced with an ever-ageing population demographic and therefore we will face challenges in meeting care requirements for these patient's ocular health. The suspicion of glaucoma and ocular hypertension are common reasons for referral to the HES and usually this in initiated from the patient's optometrist. The referring optometrist carries out tests such as tonometry, optic disc assessment and a visual field test.
Commonly patients presenting to the HES are required to undertake a further visual field assessment prior to their clinical assessment. In cases whereby the visual field test was abnormal at the optometric assessment the need for a repeat test is clear however when the visual field test at the referring optometrist was normal it calls into question the need to repeat this prior to the patients first attendance and clinical assessment.
This study aims at determining whether there is a need for routinely repeating a visual field assessment prior to a first clinic attendance when the referring optometrist felt that the visual fields were "normal" or "within normal limits".
Between 1st January 2018 and 1st December 2018 all patients referred into Loughborough Community Hospital with a suspected diagnosis of glaucoma or ocular hypertension were booked for a visual field assessment prior to their initial new patient outpatient attendance. Only patients directly referred in from their opticians were included. If the visual field test at the optician was documented as being "normal", "within normal limits", "no abnormality detected", or "OK" on the referral letter then the patient was included in the study population.
These patients underwent a visual field assessment with a Humphrey's visual field analyser on a 24-2 SITA standard protocol. The outcome of the visual field test was documented including patient age, reliability indices, Mean Deviation and Pattern Standard Deviation. The data was initially collected as part of a service evaluation project. This data was statistically analysed by one of the authors using t-tests, ANOVA and chi-square tests where appropriate to compare groups using Stata 15.
Data on visual fields of 501 consecutive patients, 1002 eyes/visual field assessments were collected. There were 218 (44%) men and 283 (56%) women included in the study with an average age for both of 60 years (sd = 11), ranging from 40-80 years old (Table 1). Any visual fields with a false negative or false positive of more than 20% were excluded from the analysis. If one eye failed both eyes were excluded. In total 6 patients were excluded.
Table 1: Patient characteristics, numbers represent count (%) unless stated otherwise. View Table 1
Glaucoma was the queried diagnosis for 173 (34.5%) of patients, OHT for 243 (48.5%) and for 85 (17.0%) the suspected diagnosis was unspecified. Intraocular pressure (IOP) on average was very similar for both eyes with a mean of 22.4 mmHg.
There were 112 (22.4%) patients with at least one eye outside normal limits, and 4 (0.80%) having both. For the right eye 81 (16.2%) patients were outside normal limits and for the left eye there were 35 (7.0%). Using a cut-off of less than -2Db for the mean deviation, 169 (33.8%) patients had at least one eye assessed with a mean deviation below -2Db, with 22 (4.4%) having both eyes. Using a cut-off of less than -3Db for the mean deviation, 21 (4.19%) patients had at least one eye assessed with a mean deviation below -3Db, with no patients having both eyes.
Only 2 patients had their right eye mean deviation less than -4Db, with values of -5.67Db and -6.75Db.
Using a cut-off of higher than 2Db for the pattern standard deviation, 218 (43.5%) patients had at least one eye assessed with a pattern standard deviation above 2Db, with 32 (6.4%) having both eyes. Using a cut-off of higher than 3Db for the pattern standard deviation, only 1 (0.20%) patient had at least one eye assessed with a pattern standard deviation above 3Db, with no patients having both eyes. There was one patient with a right eye pattern standard of 5.23Db.
There is a statistically significant difference between the mean left eye mean deviation and, in the mean, left eye pattern standard deviation in the diagnosis groups (Table 2). The OHT group have a mean left mean deviation higher than the glaucoma group (difference in means is 0.229dB (95% Bonferroni corrected CI: 0.019, 0.439)). The OHT group have a mean left pattern standard deviation higher than the unspecified group (difference in means is 0.235dB (95% Bonferroni corrected CI: 0.023, 0.447)).
Table 2: Mean deviation or pattern standard deviation for diagnosis category. View Table 2
Table 3 shows the mean and standard deviation intraocular pressure for each referred diagnosis category.
Table 3: Mean(sd) intraocular pressure for each referred diagnosis category. View Table 3
There are no statistically significant differences between the diagnosis categories in terms of the right or left eye outside the normal limits for the glaucoma hemifield test (GHT) (Table 4).
Table 4: Glaucoma hemifield test results for each referred diagnosis category. View Table 4
Table 5 shows that the mean of the mean deviation for patients with the right eye outside the normal limits is higher than for patients with their right eye inside the GHT normal limits (mean difference is 0.938 (95% CI: 0.723 to 1.154). The mean of the mean deviation for patients with the left eye outside the normal limits is higher than for patients with their left eye inside the normal limits (mean difference is 0.029 (95% CI: 0.213 to 0.271).
Table 5: Glaucoma hemifield test for mean deviation (MD) (mean(sd)). View Table 5
Table 6 shows the Glaucoma Hemifield Test outcomes related to pattern standard deviations. There is very little correlation between the intraocular pressure and mean deviation or pattern standard deviation for either eye (Table 7).
Table 6: Glaucoma hemifield test for mean deviation (MD) (mean(sd)). View Table 6
Table 7: Correlation between intraocular pressure and mean deviation and pattern standard deviation. View Table 7
Figure 1 and Figure 2 show the visual field mean deviation and pattern standard deviation figures by referral diagnosis respectively.
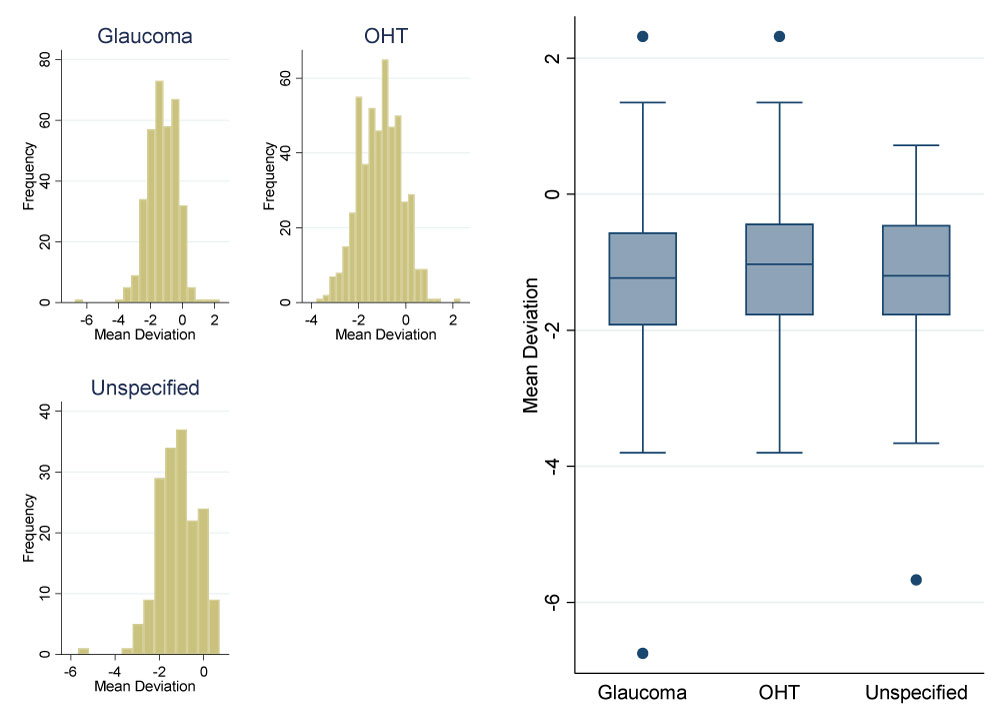 Figure 1: Mean deviation by referral diagnosis. View Figure 1
Figure 1: Mean deviation by referral diagnosis. View Figure 1
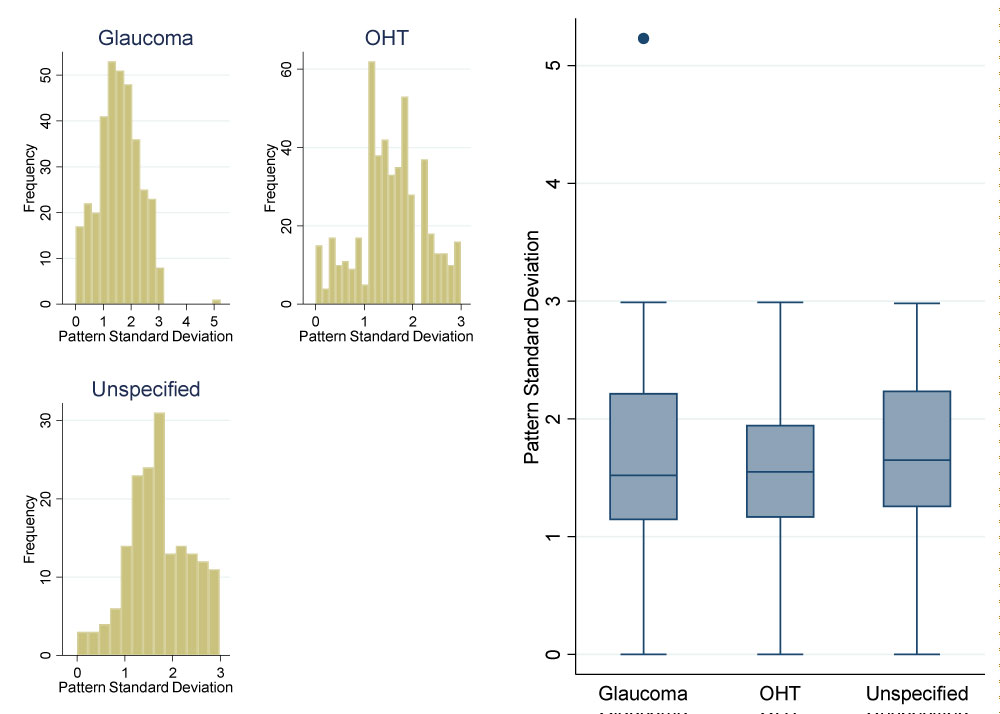 Figure 2: Pattern standard deviation by referral diagnosis. View Figure 2
Figure 2: Pattern standard deviation by referral diagnosis. View Figure 2
The Health Service is currently under strain and the large number of ocular hypertensive and glaucoma suspect patients being referred in is stretching hospital eye services. In an ideal world all patients referred in would have visual field assessments done however resources are finite and in the interests of equity of care it is important to direct those resources to patients who require it. Clearly patients who have an abnormal visual field at referral need a repeat visual field assessment and often this is normal when repeated.
The Way Forward project undertaken by the UKs Royal College of Ophthalmologists [1] predicts that from 2015 to 2035, the number of people in the UK with glaucoma will rise by 44% (22% rise from 2015 to 2025). This will be accompanied by a rise of 16% in the numbers with ocular hypertension (OHT), and 18% identified as glaucoma suspects.
These estimates are consistent with other projections; a 2009 study estimated we would see a 23% rise in the diagnosed cases of glaucoma in the UK between 2010 and 2020 [2,3]. The Way Forward estimates are for prevalence, not diagnosed cases. It is frequently quoted that 50% of prevalent glaucoma is undiagnosed so the workload may increase as diagnostic tests and screening by optometrists improves [4-9].
This study specifically did not aim to set limitations on the nature of the visual field test carried out at the referring optician to ensure the real-world applicability of our findings. Visual fields may have been via any number of commercially available visual field analysers. The primary end point was that the visual field assessment was deemed to be normal by the referring eye healthcare professional and therefore of no clinical concern. There was no requirement for the clinician seeing the patient to have sight of the visual field assessments carried out and indeed this was by design to avoid the need to scrutinise tests which would take up more time. In order to make the findings of this applicable to real world practice there was a necessity to rely upon the referring optometrist's clinical impression of the visual field test they carried out.
It is impossible to be specific and utilise mean deviation alone as a surrogate for normality. Each visual field needs to be assessed in association with all the clinical features of the patient however with limited resources targeting those who will yield diagnostically important information is of use. Outcomes with a low negative mean deviation are unlikely to have significant glaucomatous optic neuropathy. In the vast majority of these cases the repeat visual field within the Hospital Eye Service was low risk with minimal potential glaucomatous change (right eye 488 (97%), left eye 493 (98%)) (defined as a mean deviation better than -3.0dB) or within normal limits on GHT (right eye 420 (84%), left eye 466 (93%)). Of the 13 with a right eye visual field test which was abnormal (worse than -3dB) the range was -6.75 to -3.01 with a mean MD of -3.71. For the 8 patients with an abnormal left eye the range was -3.8 to -3.02 with a mean of -3.30dB. These represent minor degrees of visual loss and, if the visual field abnormality was related to a glaucomatous process, the examining clinician would have detected suspicious features on the optic nerve and then appropriately organised a visual field test at the hospital eye service. The study addresses reliable visual field tests and those cases where the reliability indices were poor were excluded. It would be anticipated that those patients who were inherently unreliable at the test would have had an abnormal visual field test at their optometry practice and therefore they would reasonably require a repeat assessment on referral to the HES.
Detecting progression is key and determining which patients are going to rapidly progress is vital. Typically, patients with established glaucoma will require frequent visual field tests in the early portion of their clinical management. If the patient did develop glaucoma, or their pre-perimetric glaucoma became perimetric, in the intervening time between referral from their optometrist, when their visual field was normal, to when they were assessed in the Ophthalmology service then the failure to repeat the test may delay the detection and commencement of treatment. This has to be balanced up against the release of capacity by not undertaking unnecessary visual field tests meaning that these patients in need can obtain visual fields rapidly and more frequently.
There was no correlation between the referral IOP or the suspected diagnosis when it was specified and an abnormal visual field test and therefore there is no clear way of determining which patients should be selected out for a repeat visual field test.
There has been significant work done on referral refinement schemes assessing patients again when their visual field is abnormal at referral however, to the authors knowledge, there has been no previous work assessing the outcomes of repeat visual field assessments solely targeting those who have a "normal" visual field assessment at referral utilising a deliberately broad and non-specific real world categorisation.
This study demonstrates that there is no need to repeat visual field tests at the hospital prior to clinical assessment if the referring optometrist has undertaken visual field tests and they are deemed by them to be normal. Clinical assessment by an ophthalmologist or allied professional will determine which cases do require repeat visual field tests and target those patients appropriately. This will result in relieving capacity problems on already stretched services and allow the visual field service to focus on patients with definite pathology requiring more frequent perimetric follow-up to detect and prevent conversion to glaucoma or progression.
I would like to thank the visual field technicians at Loughborough Community Hospital; Lianne Concannon, Karen Morely, and Heather Frealson.