Blood blister-like aneurysms (BBAs) have been described as small aneurysmal bulges, more frequently arising from non-branching sites on the supra-clinoid internal carotid artery (ICA). Their etiology is still controversial. In our case the association of the BBA, presenting with a severe subarachnoid bleeding, and extracranial ipsilateral ICA dissection in a patient with fibromuscular dysplasia, could suggest that both lesions were due to the same pathologic process. The aneurysm was treated in the acute phase with a flow-diverter stent. The patient was discharged symptoms free 24 days later. Control angiography performed 6 months later confirmed persistent aneurysm occlusion.
Blood blister-like aneurysms (BBAs) belong to a well-defined category of intracranial aneurysms, also known as "non-branching aneurysms", since they do not develop at the junction of two arteries. The most frequent location is the distal internal carotid artery (ICA) [1,2]. They are very rare with a frequency reported to vary from 0.3% to 1% of all aneurysms and affect predominantly women [3]. The prognosis, if untreated is very poor; on the other hand, treatment remains very challenging. The introduction of flow diverter stents (FDs) has improved clinical result of this very insidious disease [4,5]. We describe the endovascular treatment of a patient presenting with subarachnoid hemorrhage caused by a ruptured blood blister-like aneurysm arising from anterior wall of ICA, associated with dissection of the extra-cranial segment of the ICA. To our knowledge the present case is unique due to association of BBA with concomitant extracranial ipsilateral ICA dissection.
A 50-year-old woman was admitted to the emergency department of our Institution for a sudden headache and subsequent loss of consciousness. CT scan revealed diffuse subarachnoid hemorrhage (SAH) in basal cisterns and ventricles with moderate dilatation (Fisher grade 4). The CT angiography (CTA) demonstrated an extensive chronic dissection of extracranial right ICA with a double lumen beginning just after ICA bifurcation merging in a unique lumen approximately at the level of the skull base. No clear abnormalities of intracranial vessels were found (Figure 1a and Figure 1b). An angiography was performed confirming the extracranial ICA dissection and demonstrating a small wide neck aneurysm of the anteromedial wall of supra-clinoid right ICA, located between the posterior cerebral artery and the anterior choroidal artery, consistent with a BBA. Some dysplastic changes suggesting fibromuscular dysplasia (FMD) of contralateral extracranial ICA were also noticed (Figure 2a, Figure 2b, Figure 3a and Figure 3b).
 Figure 1: a) CT: Diffuse basal subarachnoid bleeding; b) CTA showing extensive dissection of the right ICA and mild signs of FMD of the left ICA.
View Figure 1
Figure 1: a) CT: Diffuse basal subarachnoid bleeding; b) CTA showing extensive dissection of the right ICA and mild signs of FMD of the left ICA.
View Figure 1
 Figure 2: a) Angiogram of the right common carotid artery: dissection of the ICA with the presence of a double lumen; arrowheads showing the lumen chosen to reach the intracranial sector; b) Intracranial ICA showing the blister aneurysm (arrow) on the anteromedial wall.
View Figure 2
Figure 2: a) Angiogram of the right common carotid artery: dissection of the ICA with the presence of a double lumen; arrowheads showing the lumen chosen to reach the intracranial sector; b) Intracranial ICA showing the blister aneurysm (arrow) on the anteromedial wall.
View Figure 2
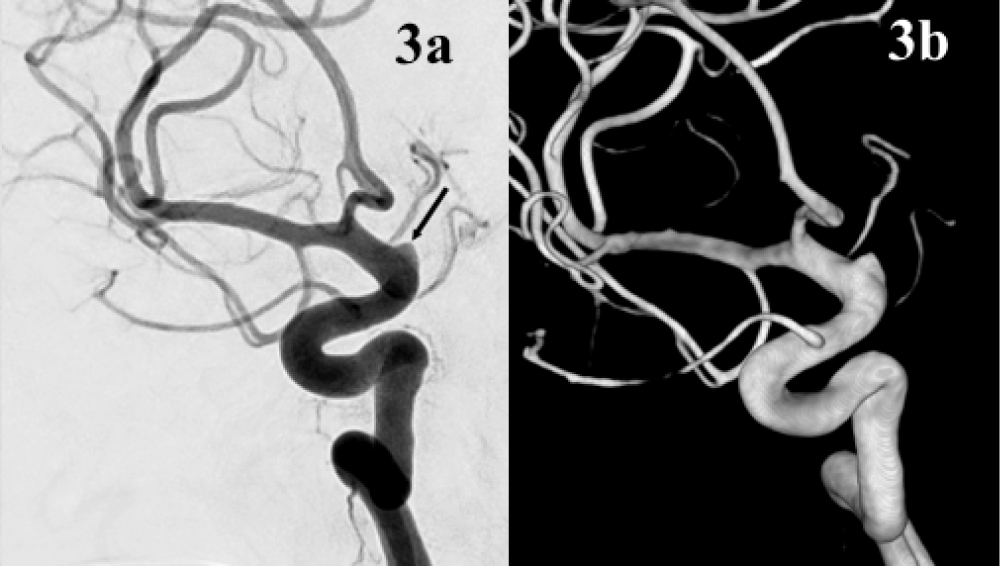 Figure 3: a,b) Angiogram, oblique view, and 3D Angiography better showing the typical shape of a blister aneurysm (arrow).
View Figure 3
Figure 3: a,b) Angiogram, oblique view, and 3D Angiography better showing the typical shape of a blister aneurysm (arrow).
View Figure 3
Despite the presence of extracranial ICA dissection, which might have increased treatment difficulty, after multidisciplinary consultation, the endovascular approach was chosen.
Before the treatment, considering the high risk of hydrocephalous and the possible need of antiplatelet therapy related to the eventual stent placement, an external ventricular drainage was positioned. A 6F long sheath was positioned at the origin of the right ICA, below the dissection. An intermediate catheter was carefully advanced through the true artery lumen up to the petrous segment, above the dissection. Then a FD (FRED, Microvention, Aliso Viejo, California, USA) was positioned from the proximal right middle cerebral artery (MCA) to the cavernous segment of ICA, covering the BBA (Figure 4). The procedure was performed under systemic heparinization (i.e. 70 UI/kg + heparin in flushing lines 5000 UI/l). Activating clotting time (ACT) was maintained between 220s and 260s for the entire duration of the procedure. Just before stent deployment 500 mg acetylsalicylic acid (ASA) was intravenously (i.v.) administered and i.v. infusion of Tirofiban was started and maintained for 12 hours. A 12 hours control CT scan excluded signs of hemorrhagic complications and a loading dose of 300 mg of clopidogrel was administered via nose-gastric probe. Double antiplatelet therapy (ASA 100 mg + Clopidogrel 75 mg) was therefore started and continued for 3 months followed by 9 months of single antiplatelet maintenance therapy.
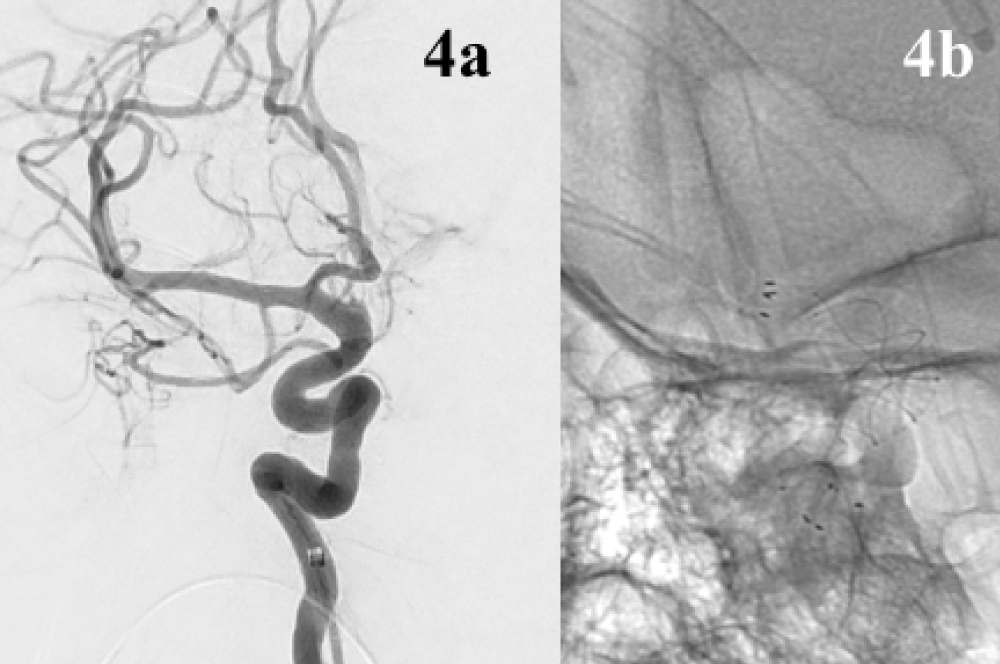 Figure 4: a,b) Immediately post-treatment angiogram, oblique views, indicating also the position of the stent.
View Figure 4
Figure 4: a,b) Immediately post-treatment angiogram, oblique views, indicating also the position of the stent.
View Figure 4
On 7th post-operative day the patient was symptoms free apart from a persistent headache. CT scan did not show re-bleeding or ischemic complications. On suspicion of vasospasm based on CTA, an angiography was performed revealing still injection of the aneurismal sac which also appeared increased in size (Figure 5). A shortening of distal end of stent, although still covering the aneurysm, was also noticed. An additional FD stent placement was discussed but a conservative management was eventually preferred, considering the positive clinical course. On 19th post-operative day a control angiogram showed complete exclusion of BBA without further changes of the stent (Figure 6). On 24th post-operative day the patient was discharged free of any neurological deficit (mRS 0). 3-months CTA followed by 6-months angiography (Figure 7) confirmed exclusion of the aneurysm and patency of the stent; the extracranial dissection was unchanged.
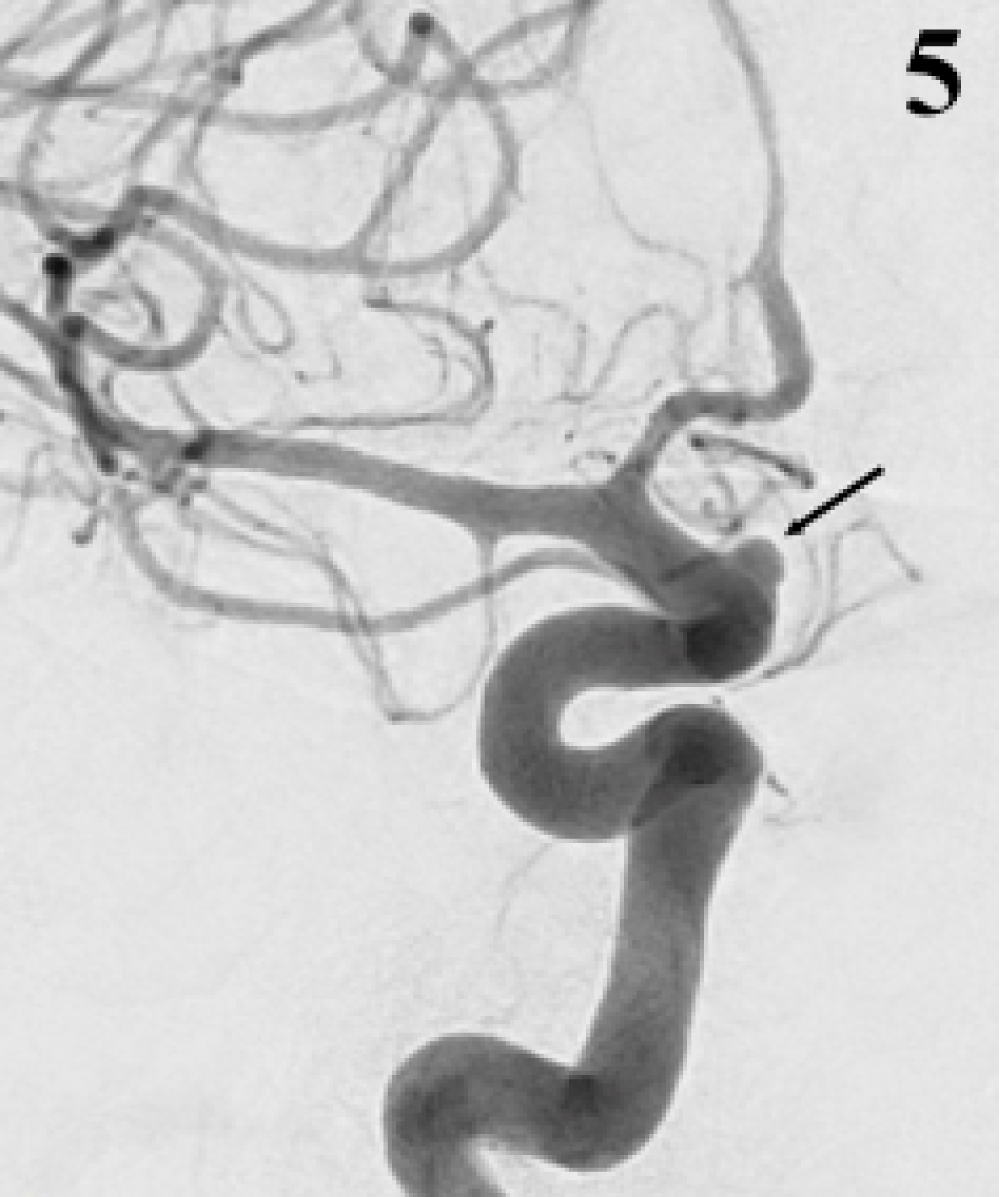 Figure 5: Control angiogram seven days later, showing the increasing volume of the aneurysm (arrow).
View Figure 5
Figure 5: Control angiogram seven days later, showing the increasing volume of the aneurysm (arrow).
View Figure 5
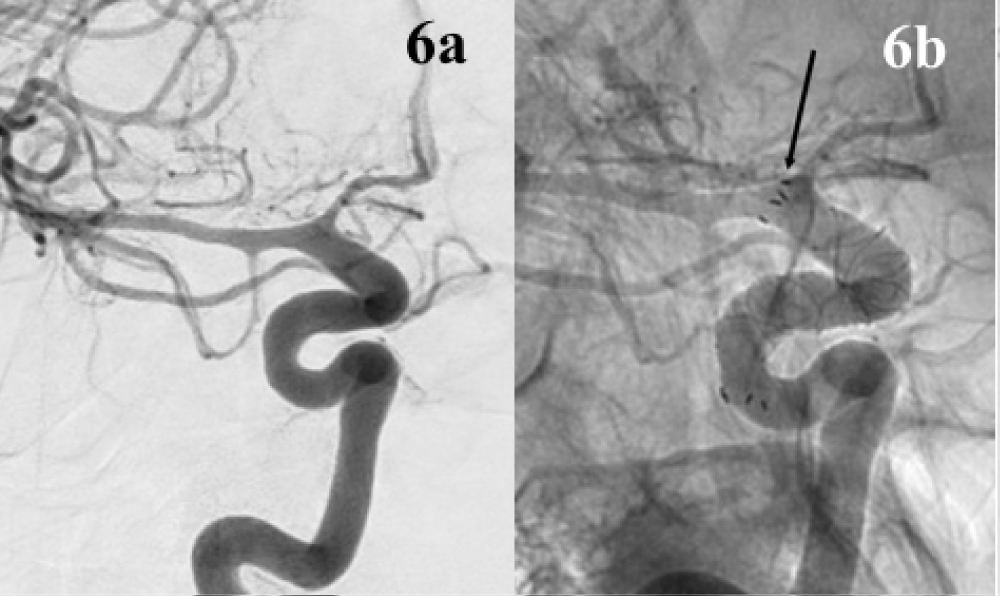 Figure 6: a,b) Control angiogram 24 days later, oblique views: The aneurysm has disappeared, there is a mild vasospasm; the stent covered completely the aneurysm in spite of the shortening of its distal end (arrow).
View Figure 6
Figure 6: a,b) Control angiogram 24 days later, oblique views: The aneurysm has disappeared, there is a mild vasospasm; the stent covered completely the aneurysm in spite of the shortening of its distal end (arrow).
View Figure 6
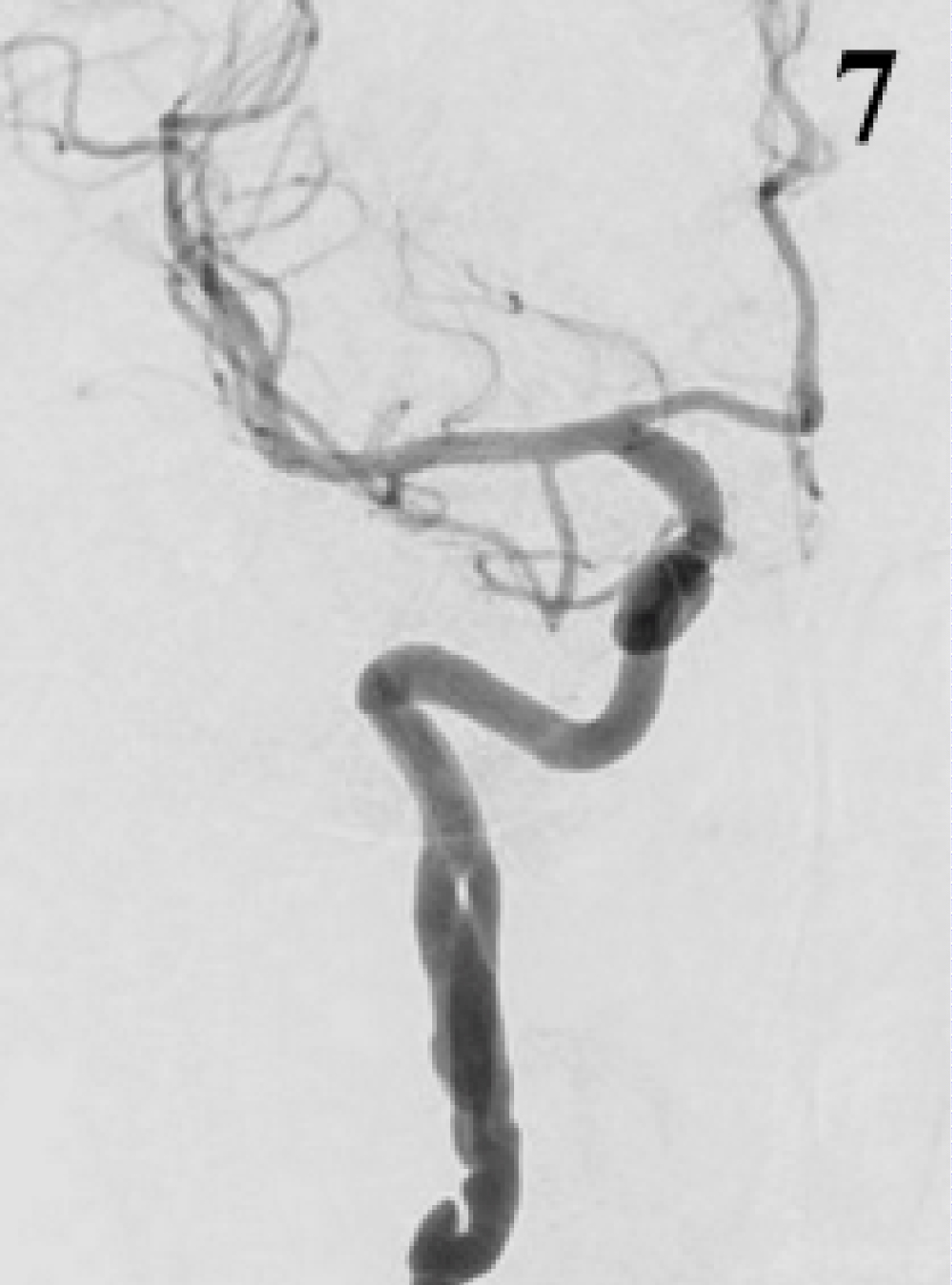 Figure 7: Control angiogram at 6 months, AP view: No more residual filling of aneurysm.
View Figure 7
Figure 7: Control angiogram at 6 months, AP view: No more residual filling of aneurysm.
View Figure 7
BBAs have been progressively become well-defined types of aneurysms, predominantly located on the anterior wall of ICA, even if other locations have been described [4-7]. The BBA appears as a small bulge of the wall sometimes difficult to recognize on angiogram. Later, within days or weeks, it grows to become a saccular lesion [8].
The treatment of BBA remains always very critical. Surgery with various approaches (ICA occlusion, wrapping, clipping) has been used [9,10]. Progressively, endovascular approach including endovascular parent artery occlusion and repairing techniques (stenting, stent-assisted coiling, balloon assisted coiling) [11] showed to be an alternative to surgery. Recently, the introduction of FD has further improved the results of the endovascular treatment as reported by many Authors [4,7,12,13]. The experience of the team involved play certainly an important role in the decision of the therapeutic strategy. In our department, since the introduction of FD, endovascular approach has become the first choice of treatment. In this case, the association of BBA with an extracranial dissection posed an additional difficulty to the endovascular treatment, because of the need to navigate the guidewire beyond the dissection in order the reach the aneurysm and the subsequent risk to get into the false lumen and to further damage the. On the other hand, surgical management was similarly very challenging considering the location of the BBA and its well-known critical morphology and fragility. Follow-up was characterized by a rapid improvement of clinical conditions and progressive disappearance of the subarachnoid bleeding on CT. The slight increasing volume of the sac on control angiography a few days after the treatment was unexpected. Some Authors interpreted this as a sign of inadequate efficacy of the stent, suggesting additional stents in an overlapped way in order to obtain a more prominent effect of flow diversion [12]. However, there is no evidence that multiple stents are more effective than a single one in preventing re-bleeding. Furthermore, considering lack of clear knowledge concerning early evolutions of these aneurysms, the early "growing" just after stent positioning could be also a normal finding corresponding to remodeling of the clot. Moreover, an additional stent could even increase the risk of thromboembolic complications.
This case allows us to make a few considerations about the pathogenesis of a lesion that remains controversial. One hypothesis is that BBAs are pseudo-aneurysms due to a sub-adventitial dissection. Indeed, a few Authors have described on operating microscope, signs of dissections recognizable on the wall of the artery close to the aneurysm [3,8]. Histologic studies, however, have shown no evidence of dissection [14,15]. According to these last Authors, the lesion was not a dissection but an expression of a focal defect of the wall covered only by adventitia and fibrous tissue. The Authors suggested that an ulceration, similar to that occurring in atherosclerotic plaques, develops penetrating progressively into the wall of the artery. The pathologic process could be similar to the one leading to focal defects due to penetrating ulcer described in the descending aorta [16]. The association, in our case, of the BBA with a clear dissection of the extracranial ICA seems to suggest that, at least in this case, both the extracranial and the intracranial lesions could be linked to the same pathologic process. It is worth noticing that signs of mild FMD were visible on both ICA. Considering the frequency of dissection characterizing the FMD [4], it can be hypothesized that in our patient FMD was a favoring factor leading to dissection involving the extra-intracranial sector as etiology of the BBA.
In our case the BBA was associated with an additional extracranial ICA dissection, possible both expression of the same disease. From a technical point of view, an accurate angiographic study with 2D and 3D images may allow in these cases, to better understand the anatomy in order to achieve a safe advancing of the catheter through the dissected artery via the true lumen up to the aneurysm. Not necessarily the absence of immediate angiographic obliteration indicates inadequate flow diversion of the stent, requiring placement of additional devices. Our case suggests that in some cases it could only represent the normal clot evolution of this very insidious and not well-known disease.
The Institutional Review Board approved the study and waived informed consent based on the retrospective nature of the study.