Cheilitis, an inflammatory condition affecting the lips, presents with various etiologies and clinical manifestations. Early and accurate diagnosis of cheilitis is essential for appropriate treatment and management. Dermoscopy has emerged as a valuable diagnostic tool in dermatology, allowing for non-invasive visualization of skin structures. This review article aims to provide an in-depth understanding of dermoscopic findings in the context of cheilitis, including the identification of specific features associated with different types of cheilitis and the potential role of dermoscopy in guiding treatment decisions.
A cheilitis is an inflammation of the lips that may spread to the skin surrounding the lips and the oral mucosa. There are various manifestations of this disorder and it can be either transient, reversible, or persistent [1]. As the disease develops, several factors can contribute, including an atopic constitution, exposure to irritants or allergens, chronic sun exposure, and infection [2].
A proper diagnosis is needed to determine the exact type of cheilitis based on its characteristics, as it is difficult to identify this disease readily in practice [3].
Cheilitis consists of a variety of types, and there are no clear guidelines for classification [4,5]. A number of different types have been identified, including actinic, inflammatory (lichen or lupus disease), infectious (leishmaniasis or tuberculosis) and tumoral types.
Dermoscopy, a non-invasive imaging technique, has gained widespread acceptance in dermatology for its ability to provide detailed visualization of skin structures.
In recent years, the application of dermoscopy has extended to the diagnosis and management of various forms of cheilitis. The technique can help differentiate between different types of cheilitis based on specific dermoscopic features, guide treatment decisions, and monitor treatment progress. This review article aims to provide a comprehensive understanding of dermoscopic techniques and findings in the context of cheilitis, with a focus on the identification of features associated with different types of cheilitis and the potential role of dermoscopy in guiding treatment decisions.
This narrative analysis was constructed using data from PubMed, an online database of medical literature. Several key articles, including systematic reviews and guidelines from various societies, were identified.
The lips are composed of 3 parts:
- External portion: The white lip, a white lip that corresponds to the classic structure of the skin. The stratified and keratinized squamous epithelium covers the dermis, which contains the sebaceous processes and sweat glands.
- Intermediate portion: The dry red lip, or vermilion; it is a semi mucosa consisting of squamous, squamous, stratified and ortho keratotic transitional epithelium, without appendages or with heterotopic sebaceous glands (Fordycespots).
- Internal portion: The moist red lip: it is a free (or mobile) mucosa composed of non keratinized stratified squamous epithelium that extends inward with the vestibules. The underlying chorion contains accessory salivary glands.
The dermoscope has recently become an aid in the diagnosis of neoplastic and inflammatory skin diseases; however, mucoscopy is still in an early stage of development [6].
A better understanding of the dermoscopic patterns seen in this particular anatomical area can improve patient management [7].
The dermoscopic features described in the literature are the background color, the morphology and distribution of the vessels, scales, and other specific structures:
The background colors assessed were a combination of white (representing keratinization) and red (representing vascularity), or Blue-grey.
The morphology of the vessels is a very important semiological element: Linear-irregular, hairpin or dotted. The vessels can be mono or polymorphic. They can be diffusely, centrally or peripherally distributed.
The color of the scales varies between yellow and white. Their distribution can be central or peripheral, diffuse or patchy.
The main white structures observed are: White radial lines, Wickham striae, whitish areas without structure, rosettes, white circles.
Blood spots, erosion or ulceration, pigmented spots and globules, lupoid, tears are sometimes found.
Lichen planus (LP) as a chronic mucocutaneous disease presents in 6% of cases on the lips with irregular erythema (macula), erosions and Wickham's striae, particularly on the lower lip [3,8], which is histologically indicated by the typical signs of lichen (Civatte's corpus, infiltration of striated lymphocytes in the upper part of the dermis, etc.) [1].
LP cheilitis should be differentiated from other forms of cheilitis such as exfoliative cheilitis, actinic cheilitis, and discoid lupus erythematosus [9].
Dermoscopic findings in lichen planus cheilitis may include [10-12] (Figure 1):
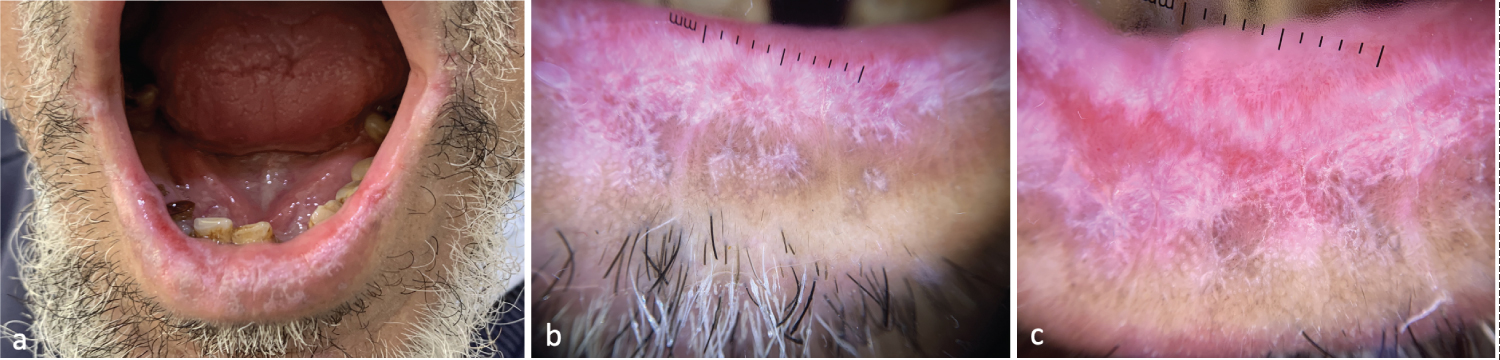 Figure 1: Dermoscopic Features of Lichen Planus Cheilitis - (a) Slightly erosive leukokeratotic plaque covering the entire lower lip; (b,c) Radial and leaf-like wickham striae, rosettes, brown pigmented spots, homogeneous hairpin and linear vessels.
View Figure 1
Figure 1: Dermoscopic Features of Lichen Planus Cheilitis - (a) Slightly erosive leukokeratotic plaque covering the entire lower lip; (b,c) Radial and leaf-like wickham striae, rosettes, brown pigmented spots, homogeneous hairpin and linear vessels.
View Figure 1
- Reticular white lines or plaques (Wickham's striae): One of the most characteristic dermoscopic features of lichen planus cheilitis is the presence of white lines or plaques with a reticular or lace-like pattern, corresponding to hyperkeratosis and hydropic degeneration of the basal cell layer in the epidermis. They can have different morphological patterns, the most common of which is the reticular pattern. 7 Other patterns described include circular, linear, radial, leaf venation like, annular and starry sky patterns.1,2,7,8.
- Erythema: Red or violaceous areas can be observed in lichen planus cheilitis, representing the underlying inflammation and vascular changes in the dermis.
- Central Erosions: These erosions may have irregular borders and can be surrounded by reticular wickham’s striae and hairpin vessels.
- Pigmentary changes: In some cases, lichen planus cheilitis may present with brown or gray-blue dots, globules, or structureless areas, which can be attributed to the presence of melanophages or melanin within the lesion.
- Vascular patterns: Although less common in lichen planus cheilitis, some cases may exhibit vascular structures, such as linear, hairpin or dotted vessels, in the inflamed areas.
Shekhar, et al. found in their descriptive study of labial LP dermoscopy in 12 patients that radial or leafy Wickham streaks were more specific for rosette-associated hairpin vessels [11].
Discoid lupus erythematosus (DLE) is a chronic cutaneous autoimmune disease, that usually affects the skin but can sometimes present with oral lesions affecting the lips, mainly the lower lip [1,13]. Labial DLE presents clinically as classic DLE plaques, or diffuse cheilitis, and presents as white plaques with central erythema, peripheral white streaks, and/or telangiectasia. Central atrophy or ulceration may be noted in long-standing lesions [14]. Because SLE can be aggressive, biopsy should be performed to detect malignant transformation [13].
Dermoscopic findings in labial discoid lupus erythematosus [7,13-15] (Figure 2):
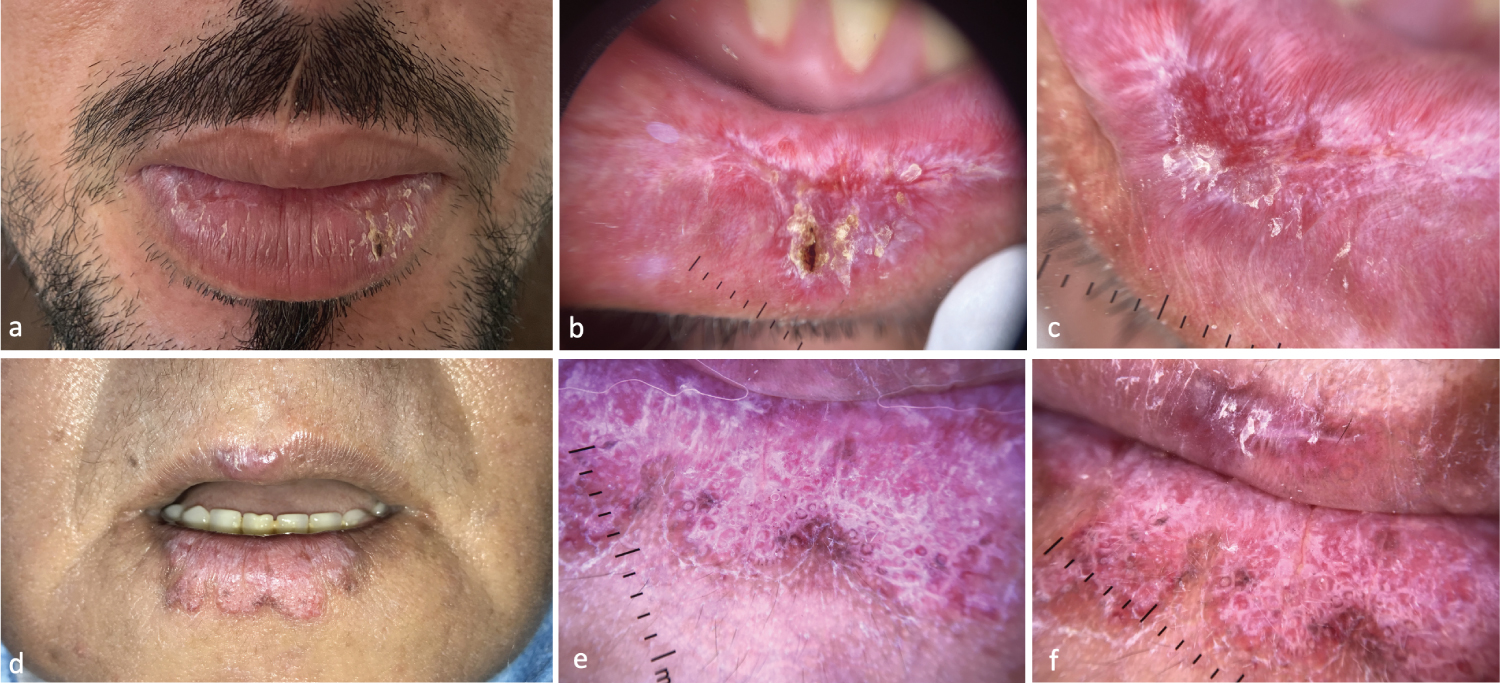 Figure 2: Dermoscopic Features of DLE Cheilitis - (a) Infiltrated dyschromic plaque centered by an erosion; (b,c) Central erosion with yellow crusts, surrounded by radial whitish structures, telangiectasias, hairpin vessels; (d) Well-limited leukokeratotic infiltrated plaque of the lower yeas; (e,f) Whitish pink background, follicular plugs, pigmented spots, peripheral linear vessels.
View Figure 2
Figure 2: Dermoscopic Features of DLE Cheilitis - (a) Infiltrated dyschromic plaque centered by an erosion; (b,c) Central erosion with yellow crusts, surrounded by radial whitish structures, telangiectasias, hairpin vessels; (d) Well-limited leukokeratotic infiltrated plaque of the lower yeas; (e,f) Whitish pink background, follicular plugs, pigmented spots, peripheral linear vessels.
View Figure 2
- Erythema: A diffuse red or violaceous background may be observed in labial DLE, reflecting the underlying inflammation and vascular changes in the dermis.
- Scaling: White or yellowish scales can be present, corresponding to the hyperkeratosis and parakeratosis typically seen in DLE.
- Follicular plugging: A characteristic finding in DLE, follicular plugging appears as white or yellowish keratotic plugs within hair follicles or sebaceous gland openings.
- Pigmentary changes: Labial DLE may present with pigmentary changes, such as brown, gray, or blue-gray dots, globules, or structureless areas. These changes can be attributed to the presence of melanophages, melanin incontinence, or post-inflammatory hyperpigmentation.
- Atrophy: As DLE progresses, atrophic changes can develop in the affected area, leading to the loss of normal lip architecture, such as the disappearance of the vermilion border and labial grooves.
- Vascular patterns: DLE may exhibit various vascular structures, such as linear, branching, or dotted vessels, which can be irregularly distributed within the lesion. These patterns reflect the angiogenesis and vascular changes associated with the inflammatory process.
- Telangiectasias: DLE can present with dilated, tortuous capillaries or telangiectasias, particularly in areas of atrophy or scarring.
In a case series (n = 7) of lip DLE described by Salah, et al. [15] most common dermoscopic features were telangiectasia, brown pigmented plaques, scales, white texture less areas, hemorrhagic plaques, and erosions.
Actinic cheilitis (AC), a potentially malignant lesion [16,17], is the most common and one of the most important disease processes affecting the lips [16]. AC is directly related to chronic UV exposure, AC may resemble the classic form of actinic keratosis with well-defined erythematous papules or scaly plaques; but there is often a diffuse, multifocal, heterogeneous lesion characterized by dry skin, scales, hyperkeratotic areas, or even atrophy [18]. Atrophy has been defined as deepening of the lips due to thin epidermis/dermis. It feels like sandpaper. Lip color may be altered (erythema or brown spots). The demarcation between the lip and the surrounding skin may be blurred. Tissue loss can occur in the form of vertical fissures or ulcerations. Plaque or hardening of the entire lip can be found. Visible areas of leukoplakia [19,20]. The diagnosis of CA is often clinical and dermatoscopy is not routinely performed prior to treatment. In terms of differential diagnosis, actinic cheilitis may resemble granulomatous cheilitis, SCC, or plasma cell cheilitis.
Dermoscopic findings associated with actinic cheilitis include the following features [19-21] (Figure 3):
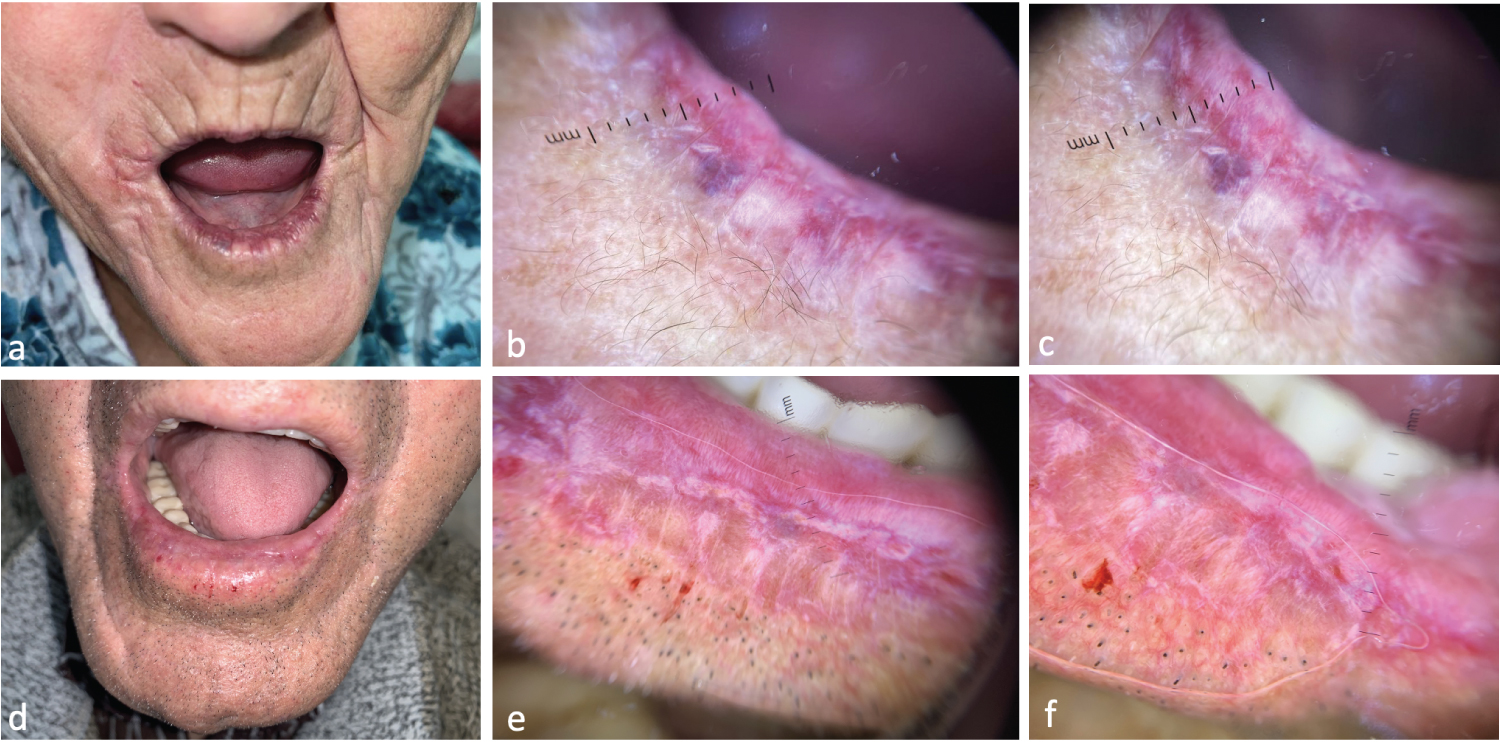 Figure 3: Dermoscopic Features of Actiniccheilitis - (a) Dry cheilitis with exaggerated radial wrinkles and erasure of vermilion; (b,c) White structureless areas, island-like whitish projections, linear telangiectasias, hemorrhagic suffusions, erasure of vermilion; (d) Leukokeratotic plaque of the lower yeast with absence of demarcation between vermilion and white yeast; (e,f) Island-like whitish projections, whitish areas without radially arranged structures, homogeneous polymorphic vx pattern of linear and hairpin vessels.
View Figure 3
Figure 3: Dermoscopic Features of Actiniccheilitis - (a) Dry cheilitis with exaggerated radial wrinkles and erasure of vermilion; (b,c) White structureless areas, island-like whitish projections, linear telangiectasias, hemorrhagic suffusions, erasure of vermilion; (d) Leukokeratotic plaque of the lower yeast with absence of demarcation between vermilion and white yeast; (e,f) Island-like whitish projections, whitish areas without radially arranged structures, homogeneous polymorphic vx pattern of linear and hairpin vessels.
View Figure 3
- Vascular patterns: Common patterns include linear-irregular vessels, dotted vessels, and occasionally hairpin vessels are noted. These vessels are generally distributed in homogeneously, with variable density and irregular spacing. In some cases of actinic cheilitis, pseudoglomerular vessels can be seen. These vessels are characterized by their tortuous, twisted appearance and can be indicative of a higher risk of malignant transformation.
- Pigmentary changes: AC may show varying degrees of pigmentation. Brown structureless areas, gray-blue structureless areas, and white structureless areas can be observed.
- Scaling and crusting: The presence of white scales and yellow crusts on the lip surface reflect the characteristic clinical presentation of dryness and desquamation associated with the condition.
- Atrophy and loss of lip architecture: Dermoscopy may reveal loss of the normal lip architecture, such as the disappearance of the well-defined vermilion border and labial grooves.
- Fissures and erosion.
- Leukoplakia: In some cases, actinic cheilitis may present with white patches or plaques on the lip surface, known as leukoplakia.
Squamous cell carcinoma (SCC) is the most common malignant tumor of the lip [22]. It is accounts for 12% of all cancers of the head and neck region, that affect frequently the lower lip. Clinically, keratotic AC plaques can progress to thickening and induration, nodule and rapid growth, and eventually ulcerate one or more of them, causing bleeding and pain.
Dermoscopic features of cutaneous SCC have been well described [22-24] (Figure 4):
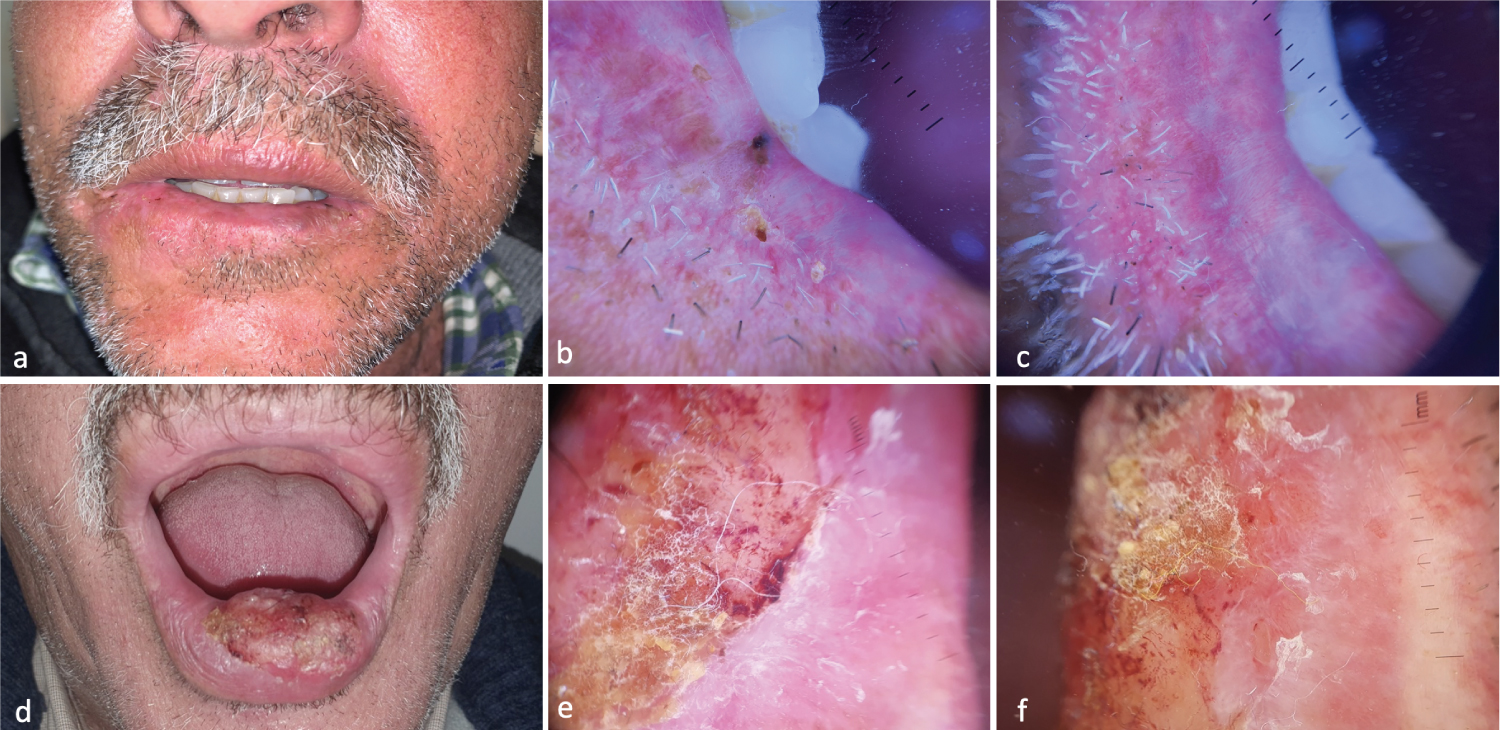 Figure 4: Dermoscopic Features of SCC Cheilitis - (a) Leukokeratotic plaque of the lower lip; (b,c) Central erosion, yellowish crusts, whitish areas without structures with hairpin vessels surrounded by whitish halo, irregular lineaments; (d) Yellowish exophytic nodule of the lower yeast with infiltrated base; (e,f) Central erosion with yellowish crusts, whitish areas without structure, polymorphic vascularization, hairpin vessels surrounded by a whitish halo.
View Figure 4
Figure 4: Dermoscopic Features of SCC Cheilitis - (a) Leukokeratotic plaque of the lower lip; (b,c) Central erosion, yellowish crusts, whitish areas without structures with hairpin vessels surrounded by whitish halo, irregular lineaments; (d) Yellowish exophytic nodule of the lower yeast with infiltrated base; (e,f) Central erosion with yellowish crusts, whitish areas without structure, polymorphic vascularization, hairpin vessels surrounded by a whitish halo.
View Figure 4
- Vascular patterns: One of the most characteristic dermoscopic features of SCC is the presence of polymorphous vascular structures. These can include hairpin vessels, glomerular, linear-irregular and dotted vessels. The vessels are often irregularly distributed and may vary in size and shape within the lesion.
- Perivascular white halo: Actinic cheilitis may exhibit perivascular white halos, which are light areas surrounding the vessels. These white halos are thought to result from dermal fibrosis or collagen deposition due to chronic sun damage. Their presence can be a useful diagnostic feature for differentiating SCC from other types of cheilitis.
- Ulceration and erosion with irregular borders.
- White structureless areas, white circle and rosettes are representing keratin, hyperkeratosis, or acanthosis. They are typically found at the periphery of the lesion and may have a yellowish hue.
- Scaling and crusting: SCC of the lip may exhibit yellow or brown crusts and white or yellow scales, reflecting the presence of keratin and parakeratosis.
- Fissures: Are linear breaks in the skin or mucosa, typically oriented perpendicularly to the vermilion border.
Moving to the dermoscopic analysis based on histological features of the lesions, Kumar, et al. [23], they observed that lip SCC may display characteristic findings according to the differentiation degree. In particular, the main difference among the three histological sub-groups was in the background; being whitish-yellow in well-differentiated lesions, pink in moderately-differentiated lesions, and red in poorly-differentiated lesions.
Mucocutaneous leishmaniasis (MCL), a protozoan infectious disease, is very rare in Iran despite the endemicity of both cutaneous and visceral forms. The lip is considered one of the extraordinary sites [25]. The condition presents with features such as nodules, plaques, ulcers, and crusting, often with a chronic and indolent course [26].
The diagnosis of MCL encompasses epidemiological, clinical and laboratory aspects. Usually, the combination of some of these elements is necessary for the final diagnosis. The lip involvement is very rare and may imitate orofacial granulomatosis such as Crohn’s disease, sarcoidosis, foreign body giant cell granuloma and Melkersson- Rosenthal syndrome [27]. MCL presents a variety of dermoscopic patterns that might cause difficulties during dermoscopic diagnosis.
Dermoscopic findings associated with leishmaniasis cheilitis may include [28,29] (Figure 5):
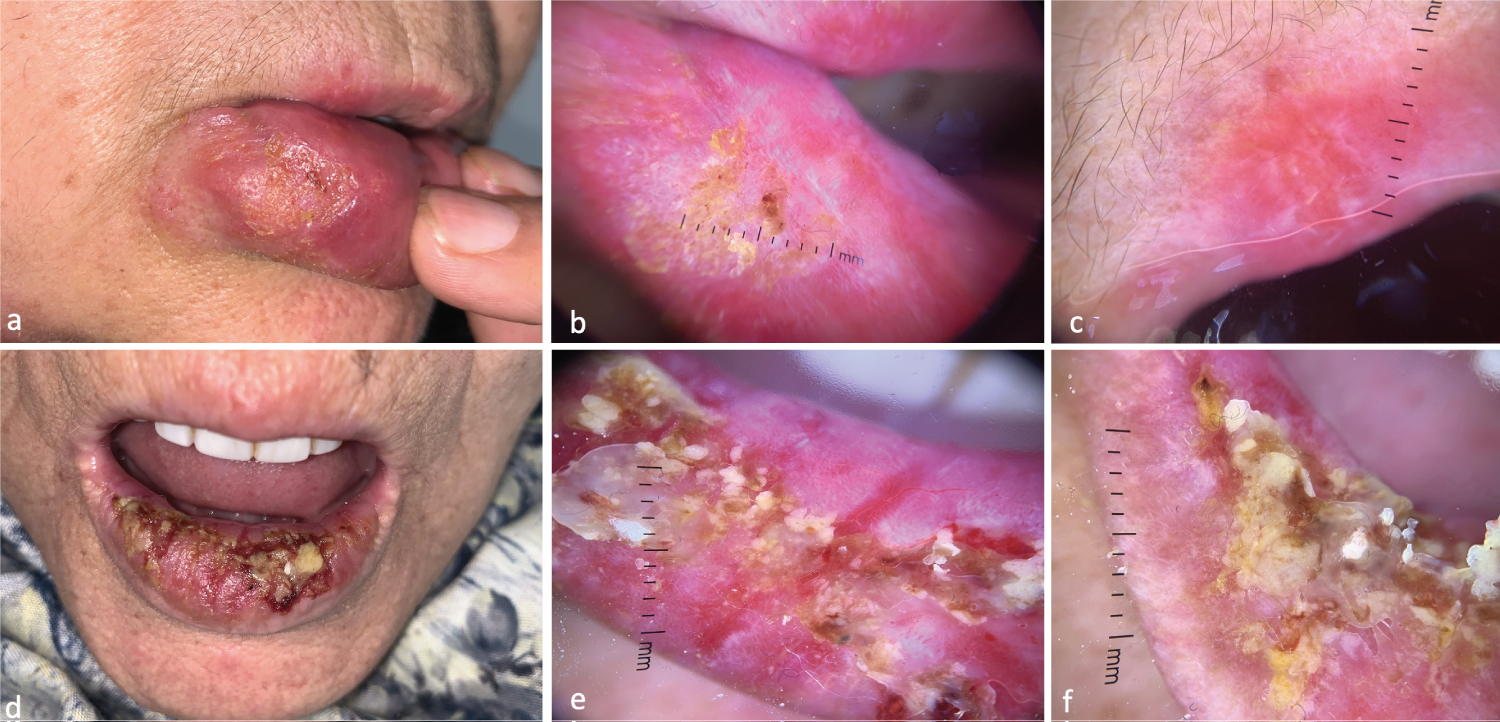 Figure 5: Dermoscopic Features of Leishmaniasis Cheilitis - (a) Macrocheilitis with unilateral erosive surface; (b,c) Yellow-orange background, lupid appearance of yellow scales, starburst appearance of polymorphic linear and dotted vessels; (d) Macrocheilitis with erosive surface occupying the whole lower lip; (e,f) Yellow-orange background, lupid appearance, yellow crusts, tears, polymorphic linear and dot-like vessels.
View Figure 5
Figure 5: Dermoscopic Features of Leishmaniasis Cheilitis - (a) Macrocheilitis with unilateral erosive surface; (b,c) Yellow-orange background, lupid appearance of yellow scales, starburst appearance of polymorphic linear and dotted vessels; (d) Macrocheilitis with erosive surface occupying the whole lower lip; (e,f) Yellow-orange background, lupid appearance, yellow crusts, tears, polymorphic linear and dot-like vessels.
View Figure 5
- Vascular patterns: Leishmaniasis cheilitis can present with various vascular structures, such as linear, branching, hairpin or coiled vessels. These vessels can be irregularly distributed and have an arborizing or serpentine appearance, reflecting the angiogenesis associated with the inflammatory process.
- Ulceration and erosion: Ulcers or erosions with well-defined or irregular borders.
- Yellowish or whitish nodules or plaques, which correspond to granulomatous inflammation and infiltration of the dermis by the Leishmania parasite.
- Yellow tears and white starburst-like patterns.
- Crusting: The presence of yellow or brown crusts may be observed in leishmaniasis cheilitis.
- Perilesional scaling.
- Perilesional erythema: Red or violaceous halo surrounding the lesion, indicating the inflammatory response to the infection.
Orificial tuberculosis (OT) is an extremely rare form of cutaneous tuberculosis (CT) [30], comprising 2% of CT and 0.1-1% of all clinical presentations of tuberculosis [31]. CT is seen especially in immune suppressed individuals and individuals with internal organ tuberculosis [30].
The oral lesions of tuberculosis may be classified into primary or secondary. In primary disease, the mouth is the initial site of infection without any focus of systemic tuberculosis. In secondary disease, CT develops secondary to internal organ tuberculosis as a result of autoinoculation [31,32].
In the oral cavity, the spectrum of lesions is extremely diverse, ranging from a painless or painful ulcer, erosion, erythematous patch, nodule and fissure either presenting singly or in multiples [31]. Dermoscopy can aid in the diagnosis and assessment of tuberculosis cheilitis by identifying specific features associated with the condition. However, it is essential to note that a definitive diagnosis requires laboratory confirmation through histopathology, acid-fast bacilli staining, or culture.
Dermoscopic findings associated with tuberculosis cheilitis may include [32,33] (Figure 6):
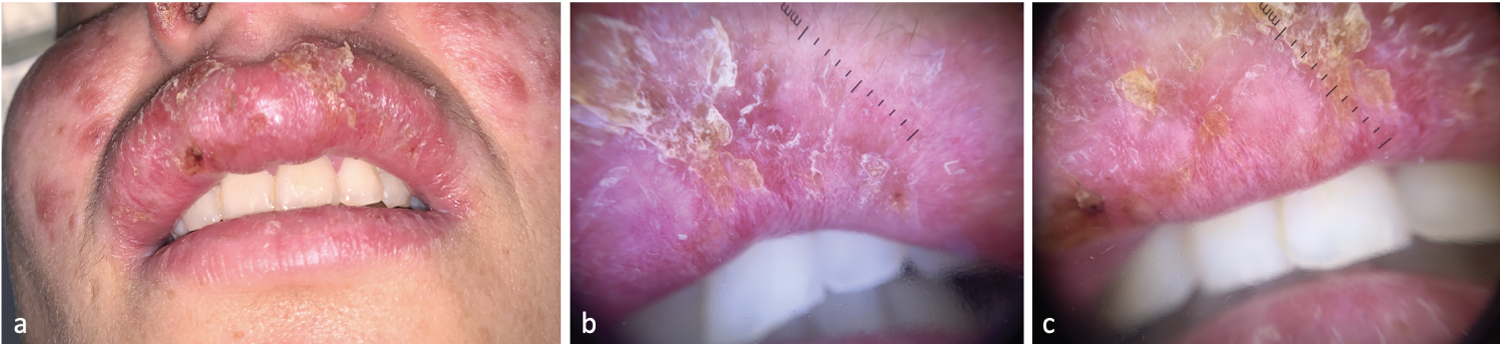 Figure 6: Dermoscopic Features of Tuberculosis Cheilitis - (a) Erosive macrocheilitis related to lupus vulgaris; (b,c) Yellow-orange background, lupoid appearance of yellow scales, polymorphous linear and dotted vessels with an irregular distribution.
View Figure 6
Figure 6: Dermoscopic Features of Tuberculosis Cheilitis - (a) Erosive macrocheilitis related to lupus vulgaris; (b,c) Yellow-orange background, lupoid appearance of yellow scales, polymorphous linear and dotted vessels with an irregular distribution.
View Figure 6
- Vascular patterns: Tuberculosis cheilitis can present with a variety of vascular structures. Linear, branching, or coiled vessels can be observed, often with an irregular distribution.
- Ulceration and erosion.
- Yellow or white nodules, which correspond to granulomatous inflammation and caseation necrosis. These nodules may be surrounded by a reddish or violaceous halo, reflecting the inflammatory process.
- Crusting: These crusts can be associated with the ulceration and tissue breakdown that occurs in the condition.
- Perilesional scaling may be seen in tuberculosis cheilitis, reflecting the involvement of the adjacent skin or mucosa.
An early and accurate diagnosis of cheilitis is crucial for several reasons. It is important to note that dermoscopic findings should always be considered in the context of the patient's clinical history, presentation, and risk factors. By identifying specific dermoscopic features, clinicians can enhance diagnostic accuracy, guide treatment decisions, and monitor treatment outcomes, ultimately improving patient care and reducing the risk of malignant transformation for certain cases.