Introduction: Dermatitis Herpetiformis is a chronic autoimmune blistering skin condition that is often associated with gluten-sensitive enteropathy. The primary lesion of DH is an erythematous papule, plaque, or, most commonly, a vesicle that can be pruritic. Most DH patients have an associated GI abnormality and a higher incidence of other autoimmune diseases, such as thyroid disease, insulin-dependent diabetes, lupus erythematosus, and vitiligo. In 70% of cases, patient with DH will require dapsone after being diagnosed and is usually needed for 1-3 years along with strict adherence to a gluten-free diet. A short course treatment of dapsone, however, along with diet modification could be sufficient to achieve disease control.
Case summary: We report a case of a 59-year-old male with a one week history of pruritic, multiple grouped vesicles initially on the upper back, gradually spreading to the entire back and bilateral extremities, no other associated signs and symptoms. Physical examination revealed multiple symmetric herpetiform groupings of erythematous papules and vesicles over the back and extremities. Skin biopsy and direct immunofluorescence were consistent with dermatitis herpetiformis. Patient was started on a gluten-free diet and dapsone 100 mg/tab once a day. After 4 weeks of dapsone, there was complete clearance of lesions. The patient was maintained on a strict gluten-free diet after dapsone was discontinued. There was no recurrence of lesions noted to this day.
Conclusion: The mechanism underlying DH is multifactorial. Exposure to gluten remains as the starting point that triggers the disease. A gluten-free diet is essential in the treatment since cutaneous and intestinal clinical manifestations are gluten-dependent, and improve with suspension of its intake. Benefits such as improvement of the intestinal mucosal atrophy, reduced risk of lymphoma and improved malabsorptive syndrome are usually noticed. Dapsone can help in alleviating symptoms while waiting for the benefit of diet modification to take effect. Although the duration of dapsone treatment may last for years in majority of cases, a number of patients may achieve clearance and disease control with a shorter course of dapsone treatment as long as a strict gluten-free diet is maintained. Future investigations will further clarify relevant cellular and molecular pathways of the immune systems in DH and elucidate on the varying response to dapsone treatment.
Dermatitis herpetiformis, Vesicles, Dapsone
Dermatitis Herpetiformis (DH) is a relatively rare disease. It is more prevalent in Scandinavian countries and in the United Kingdom. Studies conducted found an incidence of 11.5 to 19.6 affected individuals per 100,000. It affects predominantly Caucasians as compared to African-Americans or Asians. DH is characterized by often being associated to Celiac Disease [1-13].
DH may occur at all ages, but most cases affect young adults, between 15-40 years-old. It has a slight male predominance with a male to female ratio of 3:2. In younger individuals, ratio tend to be reversed with female prevalence [8].
The objective of this case is to have a case of DH that presents with multiple clusters of vesicles around the body which successfully achieved clearance of lesions and significant long term disease control after initiating immediate diet modification and a shorter, 4-week course of dapsone. DH can mimic different disease entities of inflammatory, infectious and autoimmune etiology. A thorough history, physical exam and judicious work-up can lead to a prompt diagnosis and appropriate management.
We describe a case of a 59-year-old male who presented with multiples papules and vesicles on the trunk and extremities associated with severe pruritus.
History revealed that 7 days prior, patient had onset of multiple pruritic papules and vesicles over the back associated with severe pruritus. Lesion gradually spread throughout the entire back, chest and bilateral upper and lower extremities. Patient denied any co-morbidities or allergies to food or medications. On initial dermatological consult, multiple symmetric herpetiform groupings of erythematous papules and vesicles over the back and bilateral arms, elbows, legs and knees with occasional areas of erosions and excoriations (Figure 1).
 Figure 1: Cutaneous examination findings: Multiple symmetric herpetiform groupings of erythematous papules and vesicles over the trunk and extremities.
View Figure 1
Figure 1: Cutaneous examination findings: Multiple symmetric herpetiform groupings of erythematous papules and vesicles over the trunk and extremities.
View Figure 1
Laboratory examinations include complete blood count which revealed mild leukocytosis with neutrophilic predominance. Tzanck smear was done and did not reveal multinucleated giant cells.
Skin punch biopsy revealed subepidermal cleft containing fibrin and neutrophils. There was also note of dermal edema and diffuse neutrophilic inflammatory infiltrates (Figure 2). Direct immunofluorescent studies revealed IgA deposits on the suprapapillary tips (Figure 3).
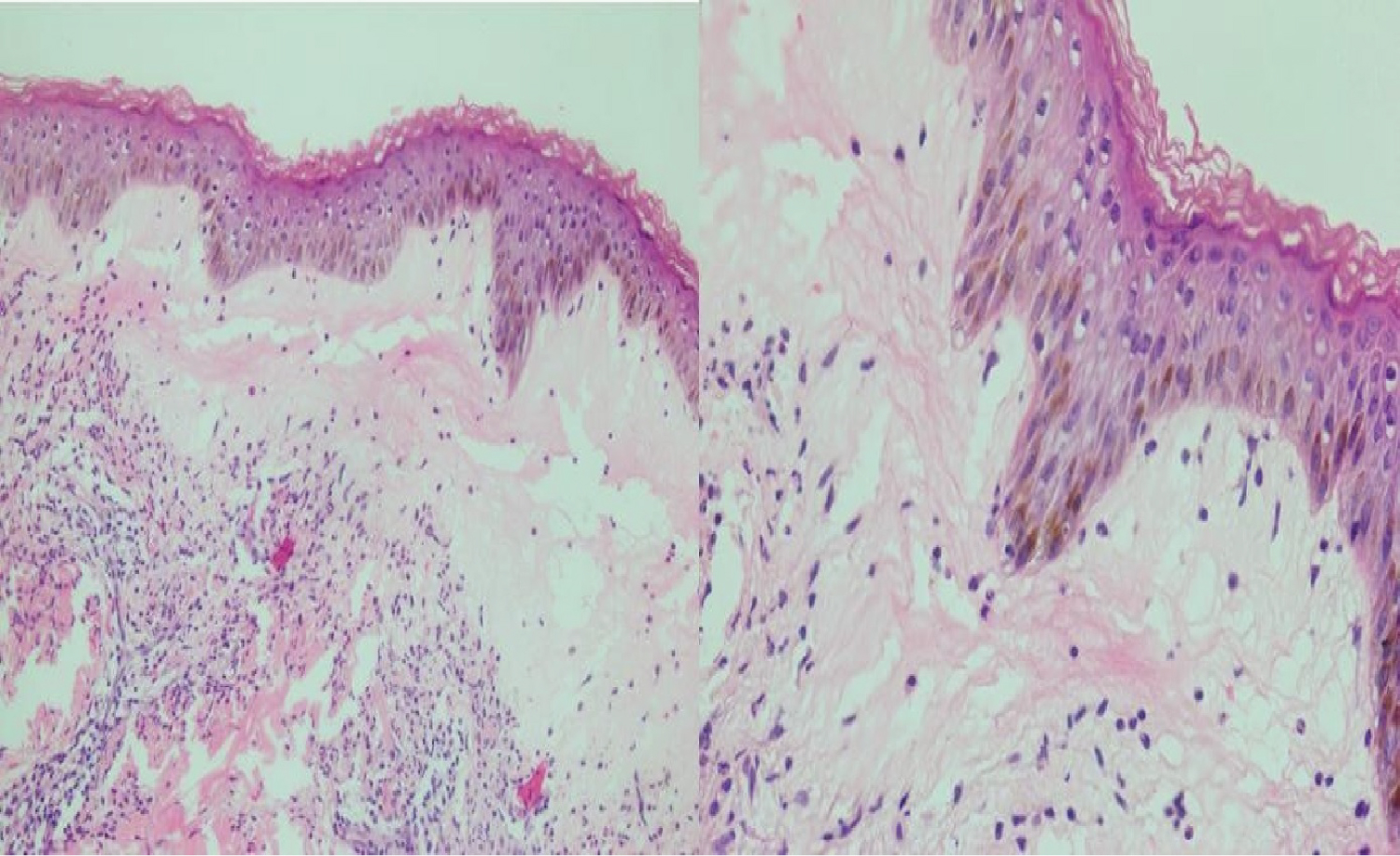 Figure 2: Histopathologic findings: Section shows a basket woven stratum corneum overlying an acanthotic and spongiotic epidermis with focal vacuolar changes and basement membrane zone thickening. Focal subepidermal cleft is also noted containing fibrin and neutrophils. The dermis reveals superficial dermal edema with diffuse inflammatory infiltrates, predominantly neutrophils with few eosinophils.
View Figure 2
Figure 2: Histopathologic findings: Section shows a basket woven stratum corneum overlying an acanthotic and spongiotic epidermis with focal vacuolar changes and basement membrane zone thickening. Focal subepidermal cleft is also noted containing fibrin and neutrophils. The dermis reveals superficial dermal edema with diffuse inflammatory infiltrates, predominantly neutrophils with few eosinophils.
View Figure 2
 Figure 3: Direct Immunofluorescence: Deposits of IgA on the suprapapillary tips. No abnormal deposits of IgG, IgM, C3, or Fibrinogen.
View Figure 3
Figure 3: Direct Immunofluorescence: Deposits of IgA on the suprapapillary tips. No abnormal deposits of IgG, IgM, C3, or Fibrinogen.
View Figure 3
Patient was immediately started on a strict gluten-free diet. After determination of G6PD levels, patient was started on Dapsone 100 mg daily and generous antihistamine to manage associated pruritus.
After four weeks of strict gluten-free diet and Dapsone, there was note of clearance of lesions on the entire body with minimal to no pruritus (Figure 4). Patient was maintained on strict gluten-free diet. However, patient arbitrarily discontinued Dapsone treatment after achieving lesion clearance after 4 weeks. Follow up examination 1 month after last Dapsone intake revealed no recurrence of lesions and symptoms. Patient was closely monitored thereafter for recurrence of lesion. Notably, there is no note of recurrence of lesions to this day for over a year.
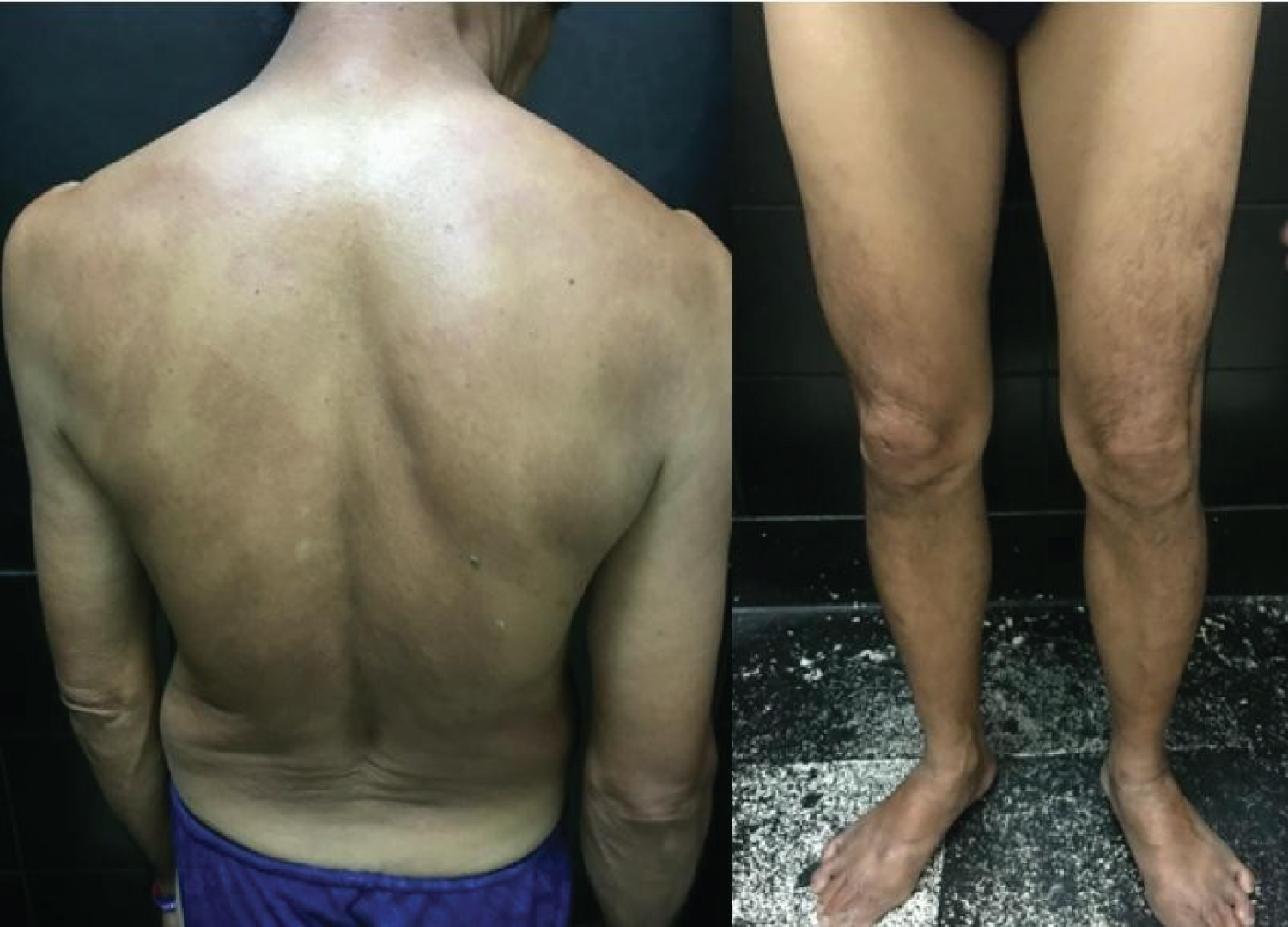 Figure 4: After 4 weeks of dapsone: Noted complete clearance of lesions.
View Figure 4
Figure 4: After 4 weeks of dapsone: Noted complete clearance of lesions.
View Figure 4
The pathophysiology of DH involves genetic factors such as HLA predisposition, environmental triggers ad dysregulation of the immune system [2].
Virtually all patients with DH carry either HLA DQ2 or HLA DQ8 haplotypes, as in Celiac Disease (CD). These alleles are inherited and the presence of both alleles provides sensitivity close to 100%. Individuals who do not carry the alleles have the diagnosis of CD but not DH [1,3,12].
The major environmental factor that triggers the disease is the exposure to gluten. Gluten is a glycosylated storage protein of cereals such as wheat, rye and barley. It is composed of two peptides, gliadin and glutenin. The disease pathogenesis is being linked to gliadin. Gliadins are the alcohol soluble part of gluten which is only partially digested in the gut because of peptides that are resistant to digestion. These digestion-resistant peptides can only be modified by tissue transglutaminase (TTG) in two ways that include deamidation and transamidation. Neoantigens are created in this process. Anti-TTG antibodies may, by cross-reaction, recognize epidermal transglutaminase (ETG), leading to the onset of IgA deposits [1-13].
An inflammatory infiltrate composed of neutrophils can be found in skin lesions of DH, usually in the papillary dermis, where IgA deposits occur. The importance of IL-8 in the neutrophilic influx has been recently studied which is a potent neutrophil activator [1,4-6].
Lesions of DH appear as grouped vesicles on an erythematous base predominantly on the elbows, knees and buttocks. Severe cases may have a generalized distribution. Lesions may be associated with intense burning sensation and pruritus, some none at all. Most patients can predict the appearance of lesions as it is preceded by stinging, burning or itching at least 8-12 hours prior. Mucous membrane affectations are rare [2-4].
All patients with DH have sensitivity to gluten, but only a small portion presents with symptoms suggestive of CD. A percentage of patients may present with some degree of steatorrhea, diarrhea, cramps, malabsorption and iron deficiency anemia. Recent studies have reported significant increase in non-Hodgkin lymphoma and GI lymphomas among patients with DH. Other associated conditions include autoimmune diseases such as thyroid disease, insulin-dependent diabetes, lupus erythematosus, Sjogren syndrome and vitiligo [10,11].
A skin biopsy must be obtained from an erythematous area near the vesicle, where neutrophilic microabscesses may be identified. Biopsy of vesicular lesions will show subepidermal blisters making it difficult to differentiate from other bullous diseases. Early lesions may show collection of neutrophils and some eosinophils before the appearance of vesicles. These are called Pierard micro abscesses, which is characteristic but not pathognomonic. As the lesions get older, there is an increase in number of eosinophils and fragment of neutrophils can be observed. Because of the possibility of numerous differential diagnoses it is ideal to perform a direct immunofluorescence. For this purpose, a biopsy should be taken on the perilesional, apparently unaffected skin up to 1 cm away from a lesion. Granular IgA deposits in the dermal papillae are observed. Deposits of complement fraction 3 may be present in half the cases [4].
Investigation of anti-TTG and anti-TGE anti- bodies, antiendomysial antibody and more recently, deamidated anti-gliadin showed good diagnostic, although not always available.
The mainstays of treatment are a gluten-free diet and drug therapy with sulfonamides or dapsone. A gluten-free diet is considered the treatment of choice for patients with CD or DH since both diseases are gluten-dependent. Not only does a gluten-free diet provide gastrointestinal benefits, it also provides cutaneous ones. Improvement may take up to two years if only gluten-free therapy is instituted. Most patients receiving drug treatment often experience abatement of symptoms as early as 3 hours after first intake and no longer experience eruptions after 2 days of treatment. The commonly used dose is 100 mg per day with maintenance dose of 1 mg/kg/day. The goal is to keep the patient under clinical control for 1 to 2 years until the benefit of diet is achieved, some patients may take as long as 2-3 years to achieve the full benefit of diet modification. The mean time for cessation of Dapsone therapy is 25 months. Suspension of dapsone without gluten-free diet will lead to recurrences. The case presented a patient with DH treated with dapsone and arbitrarily discontinued medical treatment after 4 weeks but continued with the strict gluten-free diet. Sulfonamides can also be used in acute phase of the disease with dose ranges of 500 mg to 4.5 g daily. Follow-up is required to confirm diagnosis through response in the diet and also managing complications. Patients should be evaluated every 6 to 12 months for diet adherence, development of associated diseases especially possible evolution to lymphoma [12,13].
Research especially about the pathogenesis of DH showed that it is not simply a bullous cutaneous disease but a cutaneous-intestinal disorder caused by gluten hypersensitivity. Exposure to gluten is the triggering point of a not yet fully elucidated inflammatory process. Lesions of DH tend to be very pruritic and most commonly seen on the elbows, knees and buttocks. A number of diseases may be associated with DH which may require additional work-up and screening. Direct immunofluorescence is the gold standard test to confirm a diagnosis. A gluten-free diet is essential in the treatment and Dapsone remains the primary drug of choice. The duration of dapsone treatment may take years to achieve disease control. However, a number of patients may achieve disease control in a shorter amount of time, in this case, four weeks of Dapsone. This varying response to medical treatment, specifically dapsone, is a good avenue for further investigation and study.