Eccrine syringofibroadenoma is a rare adnexal tumor of sweat glands, with different clinical presentations. It is mainly found at the extremities, but also occurs on the trunk, the nail pulp, or the eyelids. The microscopic examination shows anastomosing cords of cuboidal cells deriving from the epidermis, infiltrating the dermis and separated by a fibrovascular stroma. There are five subtypes among which reactive eccrine syringofibroadenoma, associated with lesions such as chronic ulcer, The evolution is mostly benign.The main treatment is the surgery. Herein we reported a case of reactive eccrine syringofibroadenoma, associated with chronic leg ulcer.
Reactive syringofibroadenoma, Ulcer, Adnexal tumor
Eccrine syringofibroadenoma (ESFA) is a very rare adnexal tumor [1-5]. It develops at the expense of the acrosyriringium of the eccrine sweat glands [2-4]. This tumor was described for the first time in 1963 by Mascaro [1]. The clinical presentations are quite variable from one patient to another, while the histological findings are very characteristic [6]. There are 5 clinical subtypes reported in the literature [2-5]. The last subtype, the eccrine reaction syringofibroadenoma, was added in 1997 by French [7]. Indeed, certain forms of this nosological entity occur as a result of inflammatory dermatoses such as chronic leg ulcers or venous stasis. However, they can also be associated with squamous cell carcinoma. We report a case of reactive eccrine syringofibroadenoma in a chronic leg ulcer setting.
55-year-old patient, hypertensive and compliant with treatment, come to consult for multiple cutaneous nodules of the leg and left foot with ulcers, profuse oozing, nauseating and associated with a burning sensation. The patient is not diabetic.
On physical examination of the left lower limb, multiple coalescing, ulcerative, warty pinkish nodules are observed, present primarily on the dorsal and lateral surfaces of the left foot. They are not very painful on palpation and have a firm consistency (Figure 1). The skin is hyperpigmented and indurated. There is no loss of sensitivity.
 Figure 1: Macroscopic image showing multiple coalescing pinkish, ulcerative, warty-looking nodules (star) on an ulcerated background (arrow) a) Lateral face; b) Dorsal face.
View Figure 1
Figure 1: Macroscopic image showing multiple coalescing pinkish, ulcerative, warty-looking nodules (star) on an ulcerated background (arrow) a) Lateral face; b) Dorsal face.
View Figure 1
The course is marked by a progressive extension of the lesions.
A Doppler ultrasound of the limb is performed and revealed atherosclerosis with proximal stenosis, as well as valve insufficiency of the superficial veins.
The biopsy shows acanthosis, orthokeratotic hyperkeratosis, and benign epithelial proliferation made up of thin anastomotic cords of cuboid cells originating from the epidermis and infiltrating the deep dermis (Figure 2a and Figure 2b). There are numerous blood vessels, most of which are surrounded by a marked inflammatory lympho-plasma cell infiltrate.
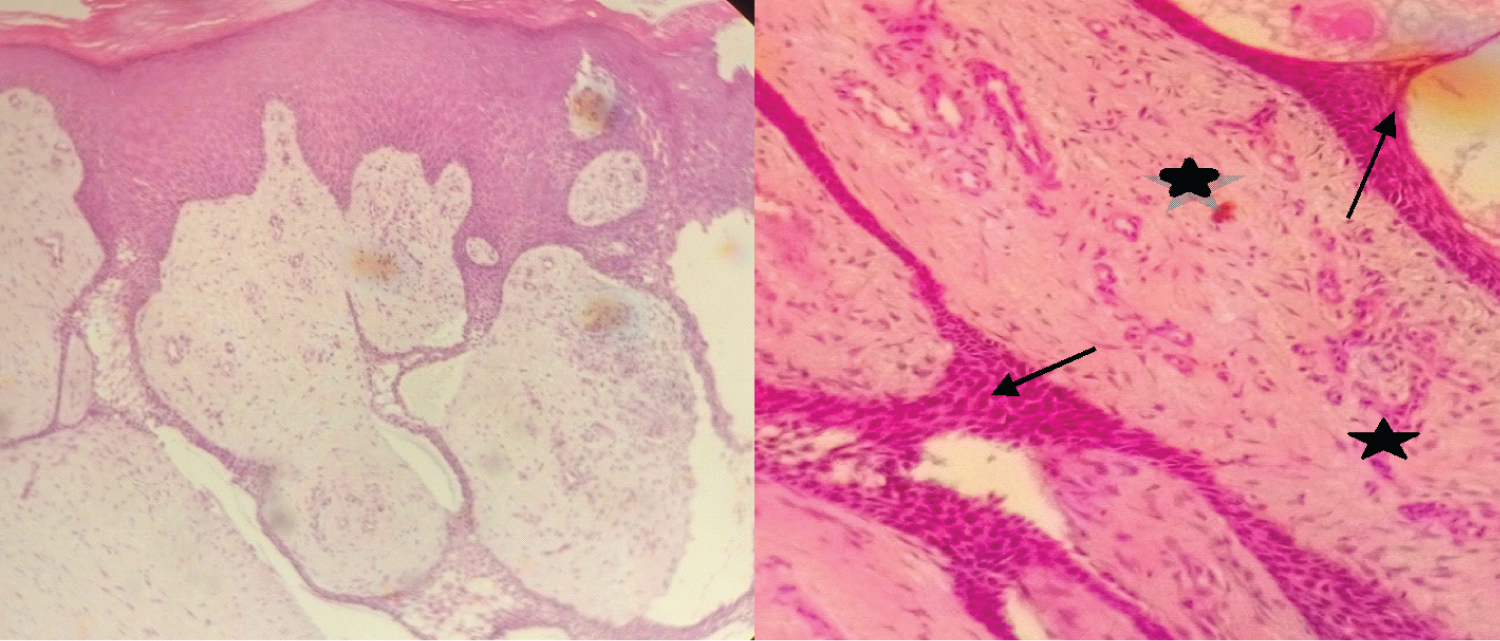 Figure 2: Microscopic examination a) Epithelial cords originating from the acanthotic and hyperkeratotic epidermis, forming anastomoses and infiltrating the dermis (HE, objective 10); b) Cords of cuboid cells (arrows) separated by a fibrovascular stroma (stars) (HE, objective 40).
View Figure 2
Figure 2: Microscopic examination a) Epithelial cords originating from the acanthotic and hyperkeratotic epidermis, forming anastomoses and infiltrating the dermis (HE, objective 10); b) Cords of cuboid cells (arrows) separated by a fibrovascular stroma (stars) (HE, objective 40).
View Figure 2
On immunohistochemistry, there is positivity for epithelial membrane antigen (EMA), for the S-100 protein and for pancytokeratins. There is a negativity for the Bcl 2 protein.
Based on the above evidence, the diagnosis of reactive eccrine syringofibroadenoma is made.
The patient is referred to a specialized service where surgical management was considered.
Eccrine syringofibroadenoma (ESFA) is a very rare benign tumor of the sweat glands, which develops mainly in patients over 60 years of age [2,8,9]. Our patient is 55-years-old and is therefore slightly below this average. Some authors report similar ages in their work: 55 years [10] and 52 years [6]. However, some mention cases that have occurred in patients aged 37 [11], or even 31 years [12].
We do not find any correlation between the occurrence of SFAE and high blood pressure.
In our case, the lesion is located at the extremities, which is the main location in the majority of cases [2,6,11,13]. Other locations are the back, abdomen, buttocks, face, and rarely the nail pulp [3,8], the eyelids [14], and the perianal region [12].
The clinical manifestations are variable. It can appear as macules, papules, nodules or plaques [4,9,11,15]. The nodules and plaques can take on a budding and warty appearance as in our patient, or even a hyperkeratotic appearance [13,16].
SFAE is divided into 5 clinical subtypes: Solitary SFAE; Multiple ESFA; Multiple ESFA associated with ectodermal dysplasia; Linear unilateral ESFA; Reactive ESFA associated with inflammatory or neoplastic dermatoses such as chronic ulcer, erosive lichen planus, bullous pemphigoid, venous stasis, or even squamous cell carcinoma [2,8,9,11]. Our case falls into the fifth group. Indeed, the ulcer is the site of constant tissue remodeling and repair which can lead to epithelial changes and eccrine ductal proliferation, thus resulting in ESFA. Some authors prefer to speak of eccrine syringofibroadenomatosis, in order to underline the reactive nature of this type of ESFA [17].
On histological examination, thin epithelial cords made up of cuboid cells are observed, anastomosing irregularly and infiltrating the superficial dermis. These cords are attached to the epidermis which is almost always hyperkeratotic and acanthotic, as in our case [6,10,14,18-20]. Perivascular infiltrate consisting of lymphocytes, plasma cells and sometimes mast cells is usual [10,15]. In contrast to our study, small eccrine ducts are frequently found within the cords [2,5,9,15,17]. The immunohistochemical study shows a positivity for the epithelial membrane antigen (EMA), for the carcinoembryonic antigen (CEA) [13,18], CK6 and CK 19 [10], and the S-100 protein [8]. In our study we observed positivity for EMA, PS-100 and pan-cytokeratins, as well as negativity for the Bcl 2 protein.
The main differential diagnosis suggested is Pinkus fibroepithelial tumor, which is characterized by the presence of more basophilic cells, separated by retraction slits from a much more cellular stroma, rich in papillary fibroblasts [21]. The immunohistochemistry shows a positivity for cytokeratins 20 (CK20), Bcl 2 and the P53 protein [22].
The course of SFAE is usually mild [5,11,14], as in our patient. Cases of spontaneous involution have been reported, as well as cases of malignant transformation into syringofibrocarcinoma and eccrine porocarcinoma [5,17].
Treatment of SFAE depends on the number, location and resectability of the lesions [2,8,23]. Surgical excision is the treatment of choice, unfortunately our patient could not benefit from it due to lack of financial means. His condition is nevertheless stable.
Other therapeutic means can be used such as cryotherapy, electrodesiccation, radiotherapy, with more or less favorable outcomes [2,14,23].
We have reported a case of reactive syringofibroadenoma in the context of a chronic leg ulcer. It is an infrequent pathology with a benign character, whose treatment of choice remains surgical excision. The interest is the mastery of clinical and paraclinical criteria in order to make an adequate diagnosis.
The authors declare no conflicts of interest.
None.