Background: High incidence of paederus insect dermatitis between peacekeepers.
The aim: Of our work is to determine the epidemiological and clinical profile of this dermatitis with a review of the literature for the last 10 years, and shed light on this pathology to better prevent it, especially with peacekeepers and transients coming from non-endemic countries.
Material and method: Retrospective epidemiological study of patient records from December 2020 to June 2021 concerning patients with paederus dermatitis at MONUSCO Level 2 Hospital in Bunia Democratic Republic of Congo and other level one hospitals of Ndoromo Camp, Kichanga and Butembo, with review of the literature for the last 10 years from the PubMed, Clinical Key and Cochrane databases.
Results: 52 patients presented to MONUSCO Level 2 Hospital in Bunia and other level one hospital for skin and/or mucous membrane lesions following crushing on the paederus insect. In 13 cases (25%) the incident was unrecognized. The age was 24 to 42 years with an average of 34 and all male.
Clinically burn pain in 94.2% cases with intense pruritus in 65% cases. Clinical examination found lesions such as macular and papillary erythema in all cases, bubbles 17.3%, vesicles 26.9%; mainly involving the neck (34 cases), the face (08 cases), the arm (5 cases) the eye (5 cases) the torso (4 cases) and other regions. Five patients had periorbital involvement mimicking orbital cellulitis in three cases (Figure 6) with periorbital edema and conjunctivitis. Some patients have one or more site of lesion, different functional signs and lesions on physical examination. All the patients were afebrile and did not present any symptoms favoring pathology.
The interrogation revealed ignorance of this insect as well as the dermatitis it can cause in 73% of cases.
The treatment was especially with local antibiotics and steroids. Three patients used honey as self-medication.
The outcome under treatment was favorable in 67.3% of cases, with hyperpigmentation-type sequelae in 32.6% of cases.
Conclusion: Paederus dermatitis is a little serious condition due to the possibility of orbital involvement and the cutaneous sequelae they can cause. It should be considered in the differential diagnosis of periocular infections and preseptal cellulitis.
However, prevention remains the key to avoiding high incidence rates, especially among peacekeepers and transients coming from non-endemic countries.
Dermatitis linearis, Paederus, Periorbital pseudo-cellulitis
Paederus dermatitis is contact dermatitis secondary to crushing on the skin and mucous membranes of an insect which is the paederus belonging to the staphilinidae family.
The insect is present in several countries but especially abundant in tropical countries. It is often overlooked by peacekeepers from non-endemic countries, explaining the high rate of paeredus dermatitis in this population especially during the dry season.
The clinic is dominated by the burning sensation with itching, erythema and skin vesicles or bubbles on examination, in ocular involvement conjunctivitis is the most common with sometimes lesions of periorbital pseudo-cellulitis [1-3].
The treatment is based on the application of cold wet compresses, oral antihistamines and topical steroids [3-6] antibiotics can be considered for the preventive treatment of secondary bacterial infections.
The outcome is often favorable, some sequelae such as skin hyperpigmentation may persist for a month or more.
Prevention is essential by many means: raising the awareness of the population, not crushing the insect on the skin, wearing protective clothing, applying repellents and using mosquito nets as well as a good environmental hygiene [7].
Retrospective epidemiological study of patients records from December 2020 to June 2021 concerning patients with paederus dermatitis at MONUSCO Level 2 Hospital in Bunia Democratic Republic of Congo and other level one hospitals of Ndoromo Camp, Kichanga and Butembo. A survey form was completed for each patient. Statistical analyses were performed using SPSS software version 27.0. The review of the literature for the last 10 years from the PubMed, Clinical Key and Cochrane databases.
Beetles are the largest order of insects. Adults and larvae of a few species occasionally bite without being harmful; some species secrete chemicals substances that can irritate the skin and eyes of humans and other animals. Beetles can cause also inhalational allergies, and some species act as intermediate hosts for helminths that cause pathology in domestic and wild animals [8].
The order coleoptera is divided into four suborders: Archostemata, adephaga, myxophaga, and polyphaga, the largest suborder, encompassing 90% of beetle families, composed of species with diverse feeding habits. Beetles are currently grouped in about 165 families [8].
More than 380,000 species of beetles have been described fewer than 100 species worldwide are known to be of public health or veterinary importance; most of these are in the suborder polyphaga. The species that have the greatest impact on the health of humans and domestic animals are in the following families: Meloidae (blister beetles), oedemeridae (false blister beetles), staphylinidae (rove beetles), tenebrionidae (darkling beetles), dermestidae (larder beetles), and scarabaeidae (scarab or dung beetles) [8].
Staphylinidae (rove beetles) in the genus paederus (Figure 2) contain pederin (c25h45o9n), a toxin more potent than that of latrodectus spider venom and the most complex non-proteinaceous insect defensive secretion known. Pederin is synthesized by endosymbiotic gram-negative bacteria (pseudomonas species) occurring in female paederus spp. The beetles, which are mostly 7 to13 mm long, are found in north, central, and south America; Europe; Africa; Asia; and Australasia (Figure 3) [9].
 Figure 1: Neck damage and hand-carried chest involvement.
View Figure 1
Figure 1: Neck damage and hand-carried chest involvement.
View Figure 1
 Figure 2: Adult beetles in the genus paederus are small, soft bodied and are roughly1 cm (1/4 to 3/4 inch) in length. They are dark orange in color with their head, front wings and the tip of their abdomen colored black. Their short front wings have a blue/green iridescent sheen to them when viewed under higher magnification [11]. View Figure 2
Figure 2: Adult beetles in the genus paederus are small, soft bodied and are roughly1 cm (1/4 to 3/4 inch) in length. They are dark orange in color with their head, front wings and the tip of their abdomen colored black. Their short front wings have a blue/green iridescent sheen to them when viewed under higher magnification [11]. View Figure 2
 Figure 3: Geographical distribution of cases of paederus vesicant dermatitis [9]. View Figure 3
Figure 3: Geographical distribution of cases of paederus vesicant dermatitis [9]. View Figure 3
They are much more brightly colored than other rove beetles, with metallic blue- or green-colored elytra and many with bright orange or red on the pronotum and the basal segments of the abdomen. These bright colors may be an example of aposematism, a warning signal to potential predators (Figure 2) [10].
A defensive function for pederin has not been demonstrated. At least 20 of the more than 600 described species of paederus have been associated with paederus dermatitis. Most cases of dermatitis have involved tropical species, including paederus fuscipes, paederus Sabaeus, paederus Cruenticollis, paederus Australis, paederus Signaticornis, paederus Columbinus and paederus Brasiliensis [8].
Pederin contacts human skin only when a beetle is crushed over it. Because of their general appearance or misunderstandings about their etiology, the resulting skin lesions have been called dermatitis linearis, spider-lick (India and Sri lanka), and whiplash dermatitis [8].
Rove beetles live in vegetable debris and under stones and other materials, such as leaf litter. Paederine staphylinids are most abundant in areas of moist soil, such as irrigated fields and other crop lands, where the adult beetles feed on various herbivorous insects. Consequently, agricultural workers and others working in fields and grassy areas are often affected. Because the beetles are attracted to lights, workers on brightly lit oil rigs and people occupying lighted dwellings in tropical areas are also commonly affected with what has been called night burn [8].
During the period between December 2020 and June 2021, 52 patients were presented to different health care structures of the MONUSCO in the DRC North Kivu Sector such as the Level 2 Hospital and other level 1 hospitals of Ndoromo Camp, Kichanga and Butembo for acute blistered skin lesions. These health care structures are destined to peacekeepers and united nations civilian personnel. All these patients were peacekeepers from different nationalities, all of them male. The age was 24 to 42 years with an average of 34 years, had presented skin and/or mucous membrane lesions following crushing on the paederus insect, happening at night in 94% cases. In 13 cases (25%) the incident of crushing voluntary the insect was unrecognized by the patient, it happened while sleeping. The interrogation revealed ignorance of this insect and the dermatitis it can cause in 73% of cases. Clinically burn pain in 94.2% cases with intense local pruritus in 65.4% of cases. Clinical examination found lesions such as macular and papillary erythema in all cases, vesicles in 26.9% and bubbles in 17.3% of cases (Table 1); mainly involving the neck (34 cases) (Figure 1), the face (08 cases) (Figure 4) the arm (5 cases) (Figure 5) the torso (4 cases) and other regions. Five patients had periorbital involvement mimicking orbital cellulitis (Figure 6) in three cases with periorbital edema and conjunctivitis (Table 1). Some patients have one or more site of lesion, different functional signs and lesions on physical examination. All the patients were afebrile and did not present any symptoms favoring another pathology. The treatment was especially with local antibiotics, steroids and antihistamines. Three patient used honey as self-medication. 8% of patients presented local superinfection (Figure 7). Time to total recovery was two weeks as an average. The outcome under treatment was favorable in 67.3% of cases, with hyperpigmentation-type sequealae in 32.6% of cases (Table 1).
 Figure 4: Neck and face damage. View Figure 4
Figure 4: Neck and face damage. View Figure 4
 Figure 5: Linear paederus dermatitis. View Figure 5
Figure 5: Linear paederus dermatitis. View Figure 5
 Figure 6: Periorbital paederus dermatitis mimicking cellulitis. View Figure 6
Figure 6: Periorbital paederus dermatitis mimicking cellulitis. View Figure 6
 Figure 7: Superinfected lesion on the side of the neck. View Figure 7
Figure 7: Superinfected lesion on the side of the neck. View Figure 7
Table 1: Epidemiological, clinical and evaluative features of the patients. Some patients have one or more site of lesion, different functional signs and lesions on physical examination. View Table 1
Some patients have one or more site of lesion, different functional signs and lesions on physical examination.
Symptoms begin within 24 to 48 hours, with burning and itching, and then develop into erythema and edematous lesions [5,12,13]. Vesicles appear toward the center of the plaque and often become pustular. Clinical symptoms are classified from mild to severe, they progress from an erythematous phase to a vesicular phase then a squamous phase [1]. Mild cases manifest only the erythematous phase with slight erythema beginning at 24 hours and resolving after 48 hours. Moderate cases manifest erythema and pruritus beginning at 24 hours, followed by a vesicular stage with blisters at 48 hours and gradually enlarging to maximal development at 96 hours. The squamous stage takes place during the next 7 to 10 days, characterized by drying out and umbilication of the vesicles, which then exfoliate and leave hyperpigmented scars that persist for a month or more. Severe cases are like moderate cases but have more extensive skin involvement, and additional symptoms such as fever, neuralgia, arthralgia, and vomiting [3]. Secondary infections, rhinitis, tympanitis, and ocular injury have also been reported [1,2]. The most affected regions are exposed areas of the body such as the neck, face, and arms [5,6,8]. The palms of the hands and soles of the feet are spared [1]. And this opens the question on the hypothesis of non-interaction of the skin of these regions with pederin toxin. Ocular and genital symptoms have been attributed to transfer of the toxin by fingers [6]. The human eye is very sensitive to the paederus toxins. Contact may happen as a result of toxin transfer from fingers or directly from the insect. Pain and lacrimation are immediate, followed by erythema and edema and in some cases blurry visual. Periocular and periorbital lesions are typical in these cases, which may progress to conjunctivitis, keratitis, and temporary vision loss [2,3].
In our series, the diagnosis was retained by epidemiological criteria with the notion of crushing the insect on the skin and the clinical presentation of the lesions with kiss-shaped lesions as well as the exposed regions and by eliminating differential diagnosis. Most of them were mild and moderate cases affecting the neck face and arm and some cases had periorbital involvement mimicking orbital cellulitis.
The main differential diagnoses to be eliminated are:
• Phytophotodermatitis [14]
• Acute allergic dermatitis,
• Thermal burns,
• Chemical burns,
• Herpes zoster,
• Herpes simplex,
• And bullous impetigo [4,15,16]
Other entities that must be considered are
• Cutaneous larva migrans [17]
• Dermatitis herpetiformis [18]
• Pemphigus foliaceus [19]
• Moth-related urticarial [21]
Wash with soap and water to remove pederin toxin. Then apply cold wet compresses, oral antihistamines and topical steroids [3-6]. Antibiotics can be considered for the preventive treatment of secondary bacterial infections. Iodine tinctures have been shown to destroy pederin and have been used to treat linear dermatitis; however, once the reaction develops, its application may be too late. According to our experience, patients usually show different signs and symptoms, and treatment must be individualized. Calamine, alcohol, menthol and other cooling agents can temporarily relieve itching, and burning emollients can also significantly relieve itching. Antihistamines can be used to relieve itching. Corticosteroids have multiple mechanisms of action on the skin, such as inhibiting the release of histamine and inhibiting mast cells. For cycles of 7 to 10 days, moderate to high-potency corticosteroids are preferred. Systemic treatment is only suitable for severe cases or cases that are resistant to local intervention. Although systemic corticosteroids are excellent anti-inflammatory drugs, they cannot immediately relieve itching, so they need to be used in combination with antihistamines.
Primary prevention consists of raising public awareness during outbreaks and reducing the use of artificial lights at night. Also several authors advocate the use of mosquito nets [3,4,12,13].
In our series the treatment was especially with local antibiotics and steroids combination with antihistamines sometimes needed. The outcome under treatment was favorable in 67.3% of cases, with hyperpigmentation-type sequealae in 32.6% of cases.
Prophylactic measures consist of:
▪ Avoiding contact with the insect by reducing night light on the terraces especially fluorescent lights, closing windows and using mosquito nets (Figure 8) during periods of risk.
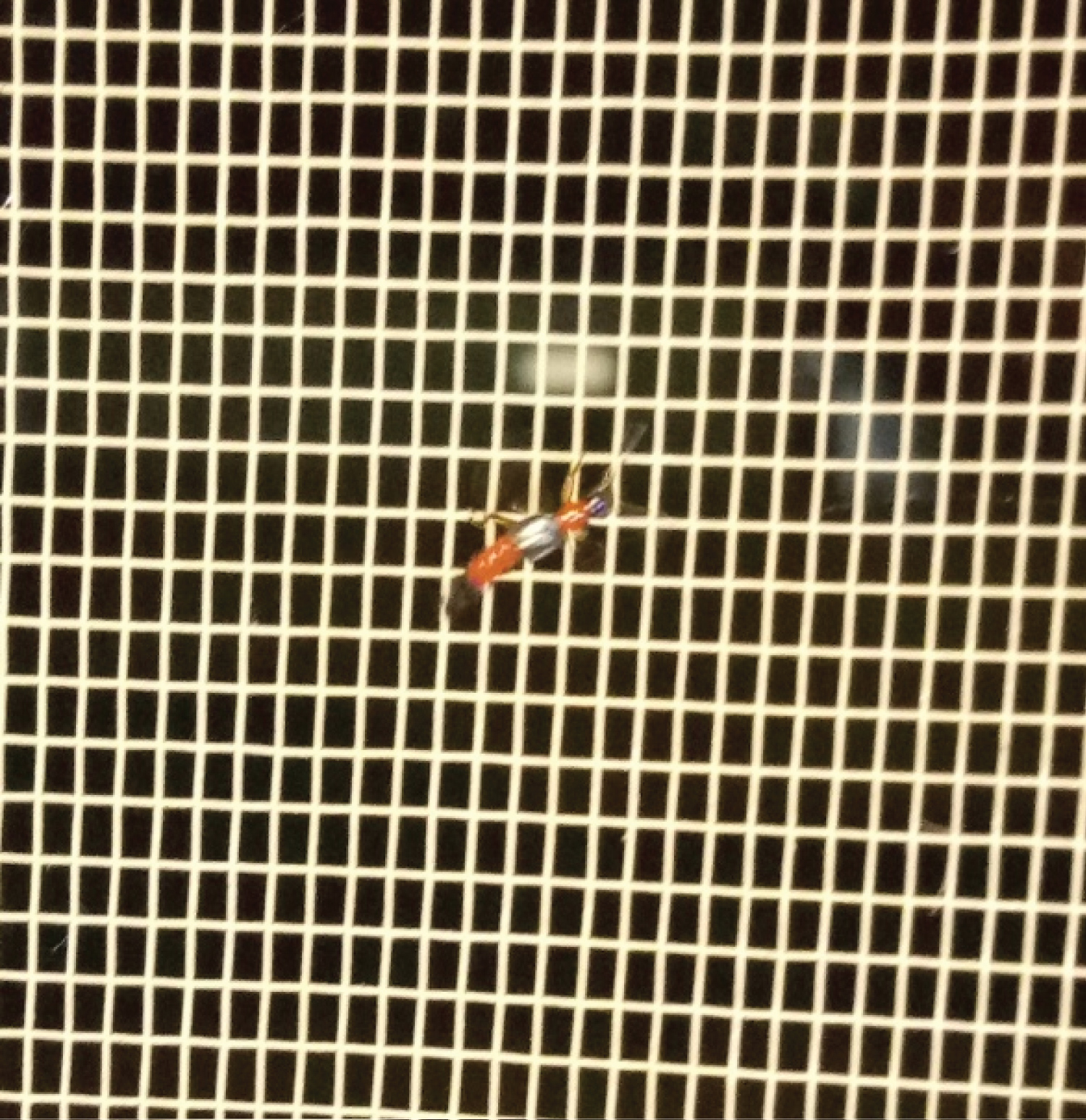 Figure 8: Paederus on the mosquito net. View Figure 8
Figure 8: Paederus on the mosquito net. View Figure 8
▪ The use of permethrin-based insecticide may be recommended.
▪ The insect should not be crushed on the skin, as a sweep of the hand or a breath is enough to drive the insect away without crushing it.
Pederin, also present in a marine sponge, is believed to block mitosis by inhibiting protein and DNA synthesis, without affecting that of RNA. This antimitotic property should be explored [9].
Paederus dermatitis is a little serious condition due to the possibility of orbital involvement and the cutaneous sequealae they can cause it should be considered in the differential diagnosis of periocular infections and preseptal cellulitis.
However, prevention remains the key to avoiding high incidence rates, especially among peacekeepers and transients coming from non-endemic countries.
None.
None.
We would like to thank the patients who allowed us to report this article with their clinical photographs.
The data that support the findings of this study are available from the corresponding author upon reasonable request.