Scar hypertrophy and keloid transformation very often present the cause of contracture. All current options for medical treatment of contracture have failed to give an immediate or near-time relief.
In this case series we implemented a jet-injection method for intralesional delivery of hyaluronic acid and successfully achieved relief of surgical and burn scar contractures.
The liquid jet permits an easy and tolerable penetration of hyaluronic acid into firm scar tissue. Biomolecular effect of HA and pressure impact of the jet synergistically contributes to reverse formation of scar tissue. Our approach was effective and safe for relief of the burn scar contractures in a few treatment sessions.
Scar hypertrophy and keloid transformation very often present the cause of contracture. It is one of the most feared sequala of burn and traumatic skin injuries. All current options for medical treatment of contracture have failed to give an immediate or near-time relief. We implemented a jet-injection treatment method successfully used in the last 10 years in clinical settings for skin remodeling and rejuvenation [1,2]. The needle-free injection modality utilizes a high-pressure jet of liquid for administration of therapeutic materials through spherical intradermal dispersion within an ø1 cm area around every skin injection point. This is case series of invalidating contractual cases treated with jet-injected hyaluronic acid.
A 54-year-old female patient suffering from a burn scar contracture involving the left axilla, upper left limb, and left lateral chest and breast was referred to a private plastic surgery clinic in order to release some mild contractures and possibly improve the look of the scar. The scar had been caused by a deep scalding injury at the age of three and involved 10% of her body surface. The initial treatment included repeated split-thickness skin grafts. During late childhood and adulthood, she underwent 21 contracture-releasing surgical interventions. The patient was reluctant to undergo further surgery in order to improve the scar appearance and extend range of motion.
At referral, she presented a 20° limitation in extending the left shoulder, with the scar spreading from the left breast through the axilla and inner arm, and reaching the left cubital fossa. Some parts of the scar were hypertrophic, as seen in Figure 1. Her Vancouver Scar Scale (VSS) was 9.
Prior to treatment, the entire scar surface was hydrated with an occlusive application of aqueous moisturizer. The patient received single treatment with hyaluronic acid (HA) filler injections administered by a pneumatic jet injection system (EnerJet2.0, PerfAction Technologies, Rehovot, Israel). The filler (Profhilo, IBSA Farmaceutical, Lodi, Italy) consists of the low molecular weight (80-100 Kda) and high molecular weight (1100-1400 Kda) HA fractions and the total concentration of 32 mg of HA. Two ml of Profhilo were diluted with sterile normal saline at 1:8 ratio resulting in the HA concentration of 3.5 mg/ml in the output solution. Each injection contained 80 μl of the solution, delivered at 25-30% pressure on the EnerJet pressure scale. A total of 16 ml of the diluted HA was injected in the identified scar lesions as a 1-cm grid covering the scar surface. The treatment was well tolerated by the patient, who reported minimal injection pain and no side effects afterwards. No other post-treatment measures were prescribed.
At 3 months, the patient began to show progressive improvement as the scar became more pliable and softer. Eighteen months after the single HA treatment, she showed improvement in the scar appearance and joint articulations and was very satisfied with the results. She also had a full range of motion in her left shoulder and cubital joints. The scar softened and was visually flatter. The color in the treated area has been normalized to the surrounding skin level (Figure 1); her post-treatment VSS score decreased to 3.
 Figure 1: Photo images of burn scar patient (a) Pre-treatment; (b) One year after the treatment.
View Figure 1
Figure 1: Photo images of burn scar patient (a) Pre-treatment; (b) One year after the treatment.
View Figure 1
A 36-years-old male was referred to a local clinic for the treatment of a scar in the front neck. Patient had a cervical spine surgery for a vertebra fractured in the car accident 2 years ago. Post-surgical scar restricts movement of his head and is accompanied by constant pruritus. No therapy was received prior to current treatment. At assessment, hypertrophic scar appears to limit backward extension of the neck to 25° (Figure 2).
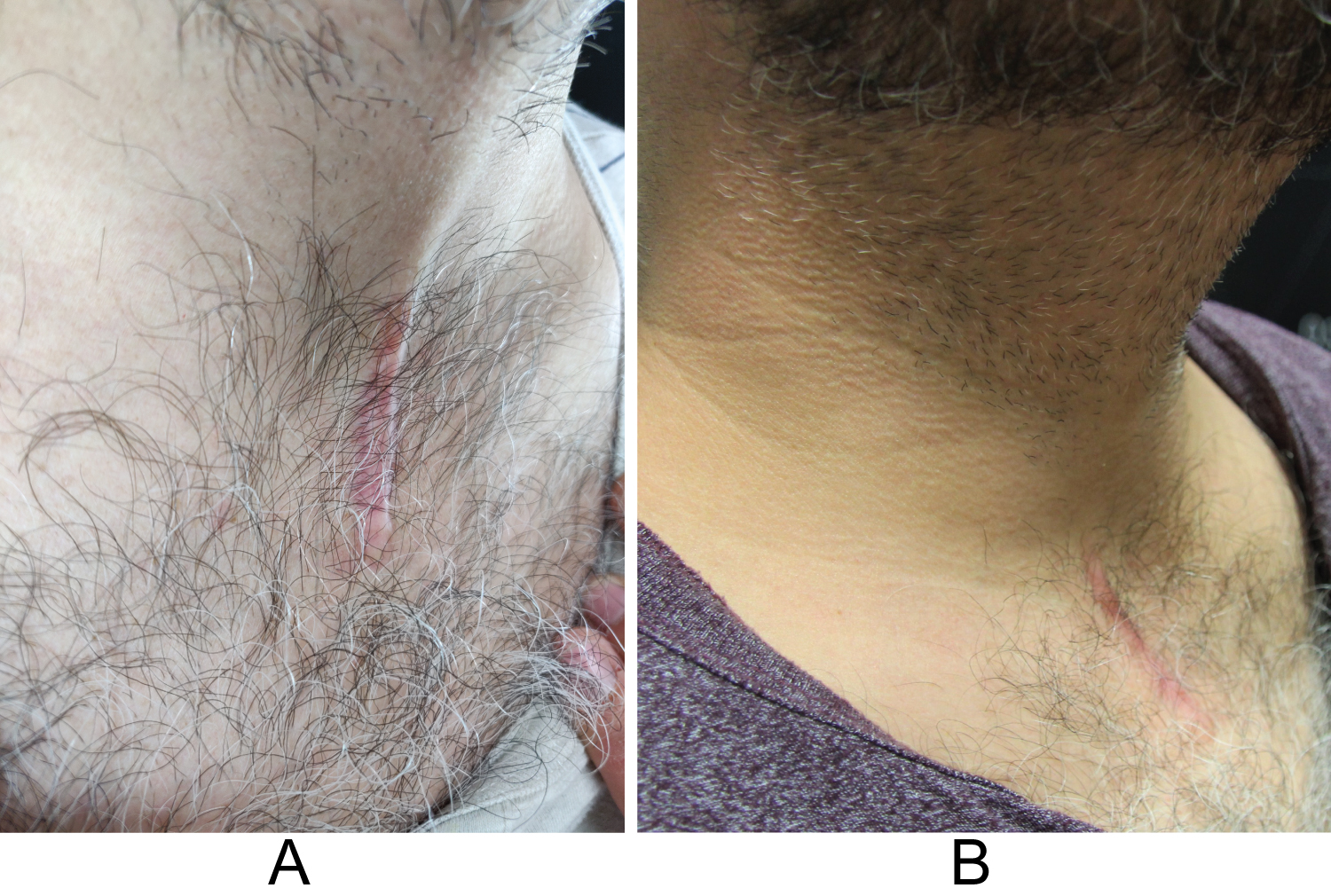 Figure 2: Photo images of surgical scar patient (a) Pre-treatment; (b) Three months after the treatment.
View Figure 2
Figure 2: Photo images of surgical scar patient (a) Pre-treatment; (b) Three months after the treatment.
View Figure 2
Patient received three series of monthly injections of HA filler (Profhilo, IBSA Farmaceutical, Lodi, Italy) using the EnerJet device. As in the Case 1, viscosity of HA gel was lowered by mixing with normal saline at 1:8 ratio to the final HA concentration of 3.5 mg/ml. Prior to treatment, the scar was prepared by applying hydrating moisturizer for 30 minutes. Each injection point received 80 μl of the solution at 30% setting on the pressure scale. Patient reported minimal discomfort during treatment that did not require any anesthesia. No side effects were documented.
The itching subsided after the first treatment and without return thereafter. A gradual softening and flattening of the scar progressively took place during the next 3 months. At the follow-up assessment 6 months after the last treatment, the range of head extension increased to 55°. VSS score decreased from 11 at baseline to 6 post-treatment.
We described two cases of scar contracture successfully treated with pneumatically injected hyaluronic acid. HA was administered as a single (Case 1) or multiple treatments (Case 2) and resulted in improved scars' texture, laxity and appearance.
Current medical management of hypertrophic scar deformities targets atrophy and softening of the scars, and includes silicone gel sheeting and intralesional injections of corticosteroids. Fractional ablative lasers have been reported to be also beneficial [3].
Previous attempts at surgical and non-surgical treatment of the first patient were not able to prevent the development of the secondary contracture that impaired the functional abilities of the injured upper limb and shoulder. A secondary concern was the uncomfortable rigidity of left mammary scarring that the patient found particularly disturbing. The second patient did not receive any prior treatment for relieving stiffness and limited mobility of his neck and head.
Hypertrophic scars are characterized by decreased expression of hyaluronic acid along with hyper proliferation and abnormal deposition of extracellular matrix (ECM) [4].
However, recent studies demonstrated ability of externally administered HA to reverse proliferation activity in the scars. Hoffman [5] showed decrease of fibroblasts overproduction, growth factor expression, and extracellular matrix deposition in keloid scars after administration of high molecular weight HA to keloid fibroblast cultures. Hyaluronic acid exhibited ability to promote recruitment of matrix metalloproteinase group of enzymes toward hydrolization and breakdown of excessive ECM [6].
Increase in hyaluronan level diminishes the phenotype conversion of fibroblasts into the scar-forming myofibroblasts which could prevent fibrotic proliferation in the scar. The bio-modulatory mechanism of hyaluronic acid normalizes fibroblast activity instead of the non-particular suppression of cell activity by steroids [7].
When applied topically to scar, external HA will not penetrate beyond the stratum corneum. Jet injection mechanism, however, allows liquid HA to penetrate the scar and be dispersed inside it in multiple directions. The kinetic energy of pressurized jet delivers effective infiltration and a homogenous biodistribution of the drug reaching all layers of the skin [8]. Beside direct injury to scar, exogenous mechanical tension has been suggested to "increases the expression of procollagen type I and tissue inhibitors of metalloproteinase in dermal fibroblasts, which improve skin wound healing" [9].
Once the liquid jet forcefully penetrates the scar, it causes instant blanching of the injected area, i.e. pressure "suffocation" of excessive local vascularization present in hypertrophic scars [10]. An instant shut down of excessive microcirculation at the injection point gradually reduces scar perfusion to a normal level. Local hypoxia by physical pressure further induces regeneration of fibroblasts, suppresses collagen production, and accelerates collagen dismantling [11].
Jet injections of HA previously demonstrated clinical efficiency for remodeling of the scar tissue. Hyaluronic acid injected into atrophic acne scar raised the scar depression and improved the skin texture [12,13]. Kim, et al. [14] successfully achieved flattening of keloid scars to significant patient satisfaction with multiple pneumatic injections of HA. Unlike other treatments which suppress the abnormal cellular tissue activity, jet-injected HA has a normalizing effect. That could explain the lack of adverse events in comparison to the frequent atrophy caused by steroid injections.
Hypertrophic scars are greatly influenced by dehydration associated with decreased level of natural hyaluronan and other glycosaminoglycans [5]. The absence of proper hydration causes constant irritation and repeated scratching that further prevent normal scar healing.
Reinmuller [15] observed cease of itching and pain in patients with hypertrophic scars after needle injections of HA. In this aspect, jet-injection of HA is more beneficial as it provides hydration not only to superficial, but also to deeper layers of the scar - as seen with relief of exhausting itching in Case 2.
We concluded that liquid jet permits an easy and tolerable penetration of hyaluronic acid into firm scar tissue. Biomolecular effect of HA and pressure impact of the jet synergistically contributes to reverse formation of scar tissue. Our approach was effective and safe for relief of the burn scar contractures in a few treatment sessions.
None.
Both authors declared that there are no conflicts of interest.
Both authors states that they equally contributed to the clinical content and preparation of this manuscript.