Lupus miliaris disseminatus faciei (LMDF) is a rare benign dermatosis, of unknown etiology and treatment often disappointing.
An 18-year-old patient presented with lupoid papulonodular lesions in the face. The diagnosis of disseminated lupus of the face was retained after eliminating other diagnoses including sarcoidosis, syphilis and leprosy. An antibacillary treatment was started without improvement for 3 months with onset of lesions. A 0.5 mg/kg/day isotretinoin treatment was started with improvement of the lesions. Thereafter, the patient benefited from 6 sessions of injection of platelet-rich plasma (PRP) with sagging scars.
LMDF is an enigmatic entity, still controversial even though it is widely recognized. Some consider it an entity in its own right whose etiopathogenesis remains to be elucidated.
Lupus miliaris disseminatus faciei, Isotretinoin, Treatment, Platelet rich plasma, Diagnosis
Lupus miliaris disseminatus faciei (LMDF) is a rare benign dermatosis, of unknown etiology and treatment often disappointing.
We report a new case of LMDF treated successfully with isotretinoin and injection of platelet rich plasma.
An 18-year-old man presented with 4 months history of asymptomatic, reddish-raised lesions over the face and earlobes. The lesions initially appeared on the chin and left side of the neck, which progressively involved his forehead, the cheeks, earlobes, upper eyelids (Figure 1). On examination, multiple, erythematous, firm papules and nodules of size ranging from 0.5 to 2 cm were seen on forehead, upper eyelids, malar region, nose, beard area, chin, earlobes. There was no cervical lymphadenopathy. Tuberculin test was negative. Chest X-ray was unremarkable. Venereal disease research laboratory (VDRL) test was non-reactive. Biopsy from a representative skin nodule showed mild epidermal hyperplasia and granulomatous reaction pattern in the dermis. Granulomas were composed of epithelioid cells; plenty of Langhan's and foreign body giant cells surrounded by a lymphocytic cuff. Extensive caseous necrosis was seen in the center of multiple granulomas (Figure 2). Stain for acid-fast bacilli and fungi were negative. A final diagnosis of lupus miliaris disseminatus faciei was made based on the above-mentioned features.
 Figure 1: Lupoid papulonodular lesions on the face and the outer ear. View Figure 1
Figure 1: Lupoid papulonodular lesions on the face and the outer ear. View Figure 1
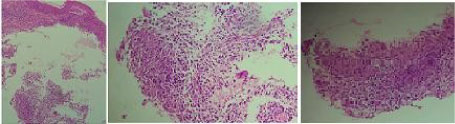 Figure 2: Cutaneous biospy showing a thinned orthokeratotic epidermis, the dermis was the site of epithelio gigantocellular granulomas with a draft of eosinophilic necrosis. View Figure 2
Figure 2: Cutaneous biospy showing a thinned orthokeratotic epidermis, the dermis was the site of epithelio gigantocellular granulomas with a draft of eosinophilic necrosis. View Figure 2
A trial of anti-tubercular therapy with the combination rifampin-isoniazid-pyrazinamide-ethambutol (4 tablets a day) was given for 2 months without improvement rather he had developed some new lesions on the arms. He was treated with isotretinoin 0.5 mg/kg/d. We note an improvement of the facial lesions with atrophic scars. He was treated with intradermal injection of platelet rich plasma every 4 weeks for 6 months. We note a good improvement of the scars (Figure 3).
 Figure 3: Improvement of the lesions with atrophic scars.
View Figure 3
Figure 3: Improvement of the lesions with atrophic scars.
View Figure 3
LMDF typically occurs as symmetrically distributed eruptions in the center of the face [1]. The lower portions of the eyelids, the lower portions of the forehead, the nasolabial folds, the cheeks, and the perioral areas are preferentially involved, but occasionally more widespread dissemination occurs.
Therapy is difficult with variable efficacy and several therapeutic modalities: Dapsone, doxycycline, minocycline, isotretinoin, clofazimine, isoniazid, and corticosteroids have been used to effectively induce remission [2,3]. Topical agents like psoralen with ultraviolet A therapy (PUVA), erythromycin and metronidazole have also been used [2]. Considering LMDF a condition related to rosacea, it may be worthwhile trying oral nicomide containing nicotinamide and zinc, which has been found to be an effective therapy in rosacea [4]. Topical tacrolimus may induce rosacea like dermatitis. A non ablatif fractional 1565 nm laser was effective in one case [5]. In our case, isotretinoin was effective on the lesions of LMDF. Platelet rich plasma injections were effective on the depressive scars.
Platelet-rich plasma (PRP) which contains large amounts of growth factors seems to be effective during the wound-healing process [6]. A review showed the efficacy and safety of intradermal injection of PRP in atrophic scars [6].
LMDF is an enigmatic entity, still controversial even though it is widely recognized. A better understanding of etiopathogenic mechanisms would improve the management of these patients, especially since there is a significant aesthetic damage. Isotretinoin and platelet rich plasma may be a useful tool in the treatment of LMDF.
None.
All the authors contributed for the acquisition, analysis, interpretation of data for the work; and drafting the work or revising it critically for important intellectual content; and the final approval of the version to be published; and the agreement to be accountable for all aspects of the work.