Paraneoplastic pemphigus is a very rare disease. However, it has been described in many countries. It most often affects middle-aged adults, but a few pediatric cases have also been reported. We report the clinical case of a patient being followed for colon cancer who developed erythematous plaques topped by clear and hemorrhagic bullae. Our patient was undergoing treatment with oral corticosteroids and chemotherapy. Paraneoplastic pemphigus was first described in 1990. Since then, numerous cases have been reported, confirming the validity of this new entity.
Paraneoplastic pemphigus, Bullous dermatosis, Systemic treatment
Paraneoplastic pemphigus is a rare cutaneous-mucosal autoimmune disease with underlying neoplasia. It is under-individualized as a different form of pemphigus compared to pemphigus vulgaris and pemphigus superficialis [1]. Paraneoplastic pemphigus is currently considered a heterogeneous mucocutaneous syndrome comprising at least 5 clinical and immunological variants: pemphigus-like, bullous pemphigoid-like, erythema multiforme-like, Graff-versus-host disease-like, lichen planus-like, and possible systemic involvement [1]. The most frequent association is with lymphoid proliferations (non-Hodgkin's lymphoma, chronic lymphocytic leukemia and Waldenström's disease, thymoma, Castleman's tumor), but other tumor types have been described (sarcoma, colonic and pancreatic adenocarcinoma, Hodgkin's disease, etc). Non-hematological pathologies are sometimes found (thymoma, carcinoma, sarcoma) [1,2]. We describe the case of a patient with paraneoplastic pemphigus bullosa-like associated with a colon tumor.
A 57-year-old woman, operated in 2017 for appendicular plastron; ileocaecal resection, with anapath in favor of colon adenocarcinoma, further excision in 2020: Right hemicolectomy. The patient developed erythematous plaques overlying clear and hemorrhagic bullae, associated with dark macules and post-bullous eruptions on the front arms, abdomen, back and a few lesions on the lower limbs (Figure 1, Figure 2 and Figure 3) for two months. A skin biopsy was performed, and histological examination revealed a sub-epidermal detachment resulting in bullae containing serous fluid and numerous eosinophilic polynuclear (Figure 4). The roof of these bullae is made up of an epidermis free of acantholysis and necrosis. Direct immune fluorescence (DIF) showed the presence of IgG and C3 intercellular deposits, creating a "lattice-like" appearance in the lower part of the epidermis. The patient was treated with oral corticosteroids and chemotherapy.
 Figure 1: Erythematous plaques surmounting bullae with clear and haemorrhagic content, associated with dark macules and post-bullous eruptions on the front arm and abdomen.
View Figure 1
Figure 1: Erythematous plaques surmounting bullae with clear and haemorrhagic content, associated with dark macules and post-bullous eruptions on the front arm and abdomen.
View Figure 1
 Figure 2: Erythematous plaques surmounting bullae with clear and haemorrhagic content, associated with dark macules and post-bullous eruptions on the abdomen.
View Figure 2
Figure 2: Erythematous plaques surmounting bullae with clear and haemorrhagic content, associated with dark macules and post-bullous eruptions on the abdomen.
View Figure 2
 Figure 3: Vesicles with clear, haemorrhagic content, associated with dark macules and post-bullous eruptions on the back.
View Figure 3
Figure 3: Vesicles with clear, haemorrhagic content, associated with dark macules and post-bullous eruptions on the back.
View Figure 3
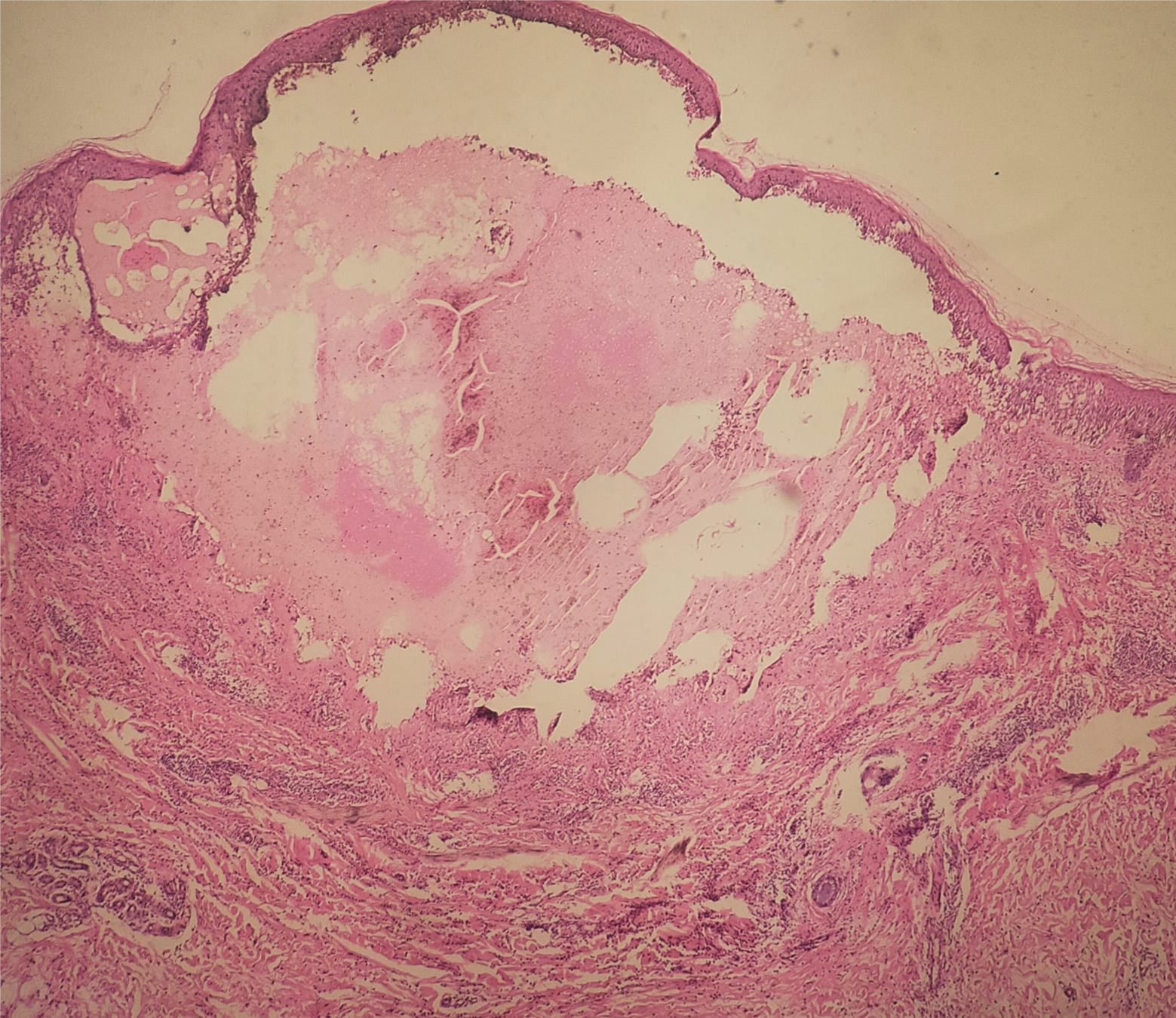 Figure 4: Subepidermal detachment.
View Figure 4
Figure 4: Subepidermal detachment.
View Figure 4
Paraneoplastic dermatoses do not result from the direct extension of cancer, but their presence is suggestive of an underlying tumor whose development always precedes cutaneous manifestations [1]. The eruption is characterized by its polymorphism, roughly combining signs of pemphigus, erythema multiforme and bullous pemphigoid. The evolution of the dermatosis parallels that of the cancer, with regression when the cancer is in remission, and resumption of evolution in the event of recurrence of the neoplasia [2]. Solid tumors (most commonly breast, lung and skin, but all organs can be affected: Liver, ovary, uterus, urinary tract, esophagus, stomach, pancreas, rectum, carcinoid tumor, nervous system, muscle, etc.) are most often associated with pemphigus vulgaris, more rarely with superficial pemphigus and exceptionally with paraneoplastic pemphigus [1]. Pemphigoid-like paraneoplastic pemphigus is an autoimmune bullous dermatosis characterized by the clinical manifestations of pemphigoid and the histology of pemphigus. Treatment is poorly codified, and data on therapeutic efficacy are based on clinical cases or case series, and on a conceptual analogy with pemphigus vulgaris. Therapeutic management involves treating the pemphigus as well as identifying and treating the underlying neoplasia. Early treatment of the tumor is a priority.
Paraneoplastic pemphigus is almost always associated with tumour proliferation, usually malignant, usually preceding the discovery of pemphigus. The prognosis of the disease is extremely poor, both because of the associated cancer and because of the severity and resistance to treatment of the mucosal lesions [3,4]. Death occurs on average 9 months after diagnosis of the disease, most often due to sepsis and respiratory failure. However, several cases of prolonged survival have been reported, with mortality lower than that classically reported [3]. Treatment of the tumour or associated hemopathy is the first stage of therapy, but is rarely sufficient. Specific treatment of pemphigus is always associated with.