Background: Behaviour change programmes have demonstrated diabetes risk-reduction benefits. Studies on diabetes preventive lifestyle activities largely focus on middle-aged/older adults. We investigated non-diabetic young adults' risk of developing Type 2 diabetes mellitus, and their attitudes and behaviours towards preventive lifestyle activities.
Methods: A descriptive cross-sectional study on non-diabetic, young adults living in Middle Eastern countries. Data was collected and analyzed electronically.
Results: Mean diabetes risk score was ̄x = 2.8 (SD ± 1.3), and 92.6% demonstrated a low risk of developing diabetes. About 88.1% agreed on the importance of maintaining a healthy lifestyle at a young age, and 92.9% thought a healthy lifestyle would help them to stay healthy. Weekly 38.0% and another 38.0% ate fruits and vegetables respectively on 2 to 3 days only. Additionally, 85.0% indicated that their work did not involve vigorous-intensity activity, 54.9% walked or used a bicycle for at least 10 minutes, and 74.2% did not do vigorous-intensity sports/fitness/recreational activities for at least 10 minutes continuously. There was a weak and negative correlation between age and diabetes risk score (r = -0.1), and BMI was positively correlated with diabetes risk score (r = 0.63).
Discussion: The participants mostly demonstrated a low risk of developing Type 2 diabetes, were overweight on average, and did not meet the recommended lifestyle practices. The reported positive attitude towards preventive lifestyle measures did not correspond to their collective reported lifestyle behaviours/practices.
Conclusion: Healthcare professionals need to focus on the practical (behavioural) aspects of healthy lifestyle modification educational activities for young adult patients.
Diabetes Mellitus (DM) is a chronic condition characterized by high blood sugar levels because the body either does not make enough insulin or the insulin is not functioning effectively even if available in sufficient quantities [1]. The initial scenario classically depicts Type I diabetes while the latter is characteristic of Type 2 diabetes mellitus. It is a disease with global epidemiological significance. According to the 2021 report of the International Diabetes Federation [2], about 537 million adults aged 20-79 years are living with diabetes mellitus globally, and this number is projected to rise to 643 million people by 2030, and 783 million people by 2045. In addition, the IDF reported that diabetes mellitus was responsible for 6.7 million deaths in 2021. It was similarly reported that in the Middle East and North Africa (MENA) region, one in six adults (about 73 million people) are living with diabetes mellitus, and this number is also projected to rise to 95 million people by 2030 and 136 million people by 2045.
A systematic review of existing studies on the estimate of prevalence of type 2 diabetes mellitus among men (18 years and above) in the Middle East, in both urban and rural areas showed a high prevalence: Bahrain (33.60%), Saudi Arabia (29.10%), United Arab Emirates (UAE; 25.83%), and Kuwait (25.40%) while the others are Iran (9.90%) and Yemen (9.80%). The random pooled prevalence in the Gulf Cooperation Council (GCC) states was 24.0% compared to 16.0% in the non-GCC states. In GCC and non-GCC countries combined, it was 19%. A rising prevalence of the disease was identified in Bahrain, Saudi Arabia, UAE, and Kuwait [3].
The incidence of Type 2 diabetes mellitus is higher in specific groups or situations such as having prediabetes, being 45 years and older, being overweight, having a family history of type 2 diabetes, physical inactivity, or a history of gestational diabetes [4]. The effective role of lifestyle intervention activities such as dietary modification and exercise in the prevention or decreasing the incidence of diabetes mellitus and its complications among various groups of people have been demonstrated by numerous studies [5-8]. A recent study found an increase in premature mortality with increasing prevalence of obesity among a population [9]. Similarly, maintaining weight loss achieved through intensive lifestyle intervention might be beneficial in terms of lowering the risk of cardiovascular events as seen in a study among adults with overweight or obesity and Type 2 diabetes mellitus [10].
Most of the at-risk populations, which may include young adults, lack adequate knowledge of the disease, and/or the specific ways through which they can achieve and maintain optimal health through self-initiated or monitored preventive measures thus, the need for education aimed at enhancing their understanding [1]. An example of relevant programmes include behaviour change programs that have demonstrated diabetes risk-reduction benefits [11,12]. From another perspective, the Health Belief Model suggests that a person's belief in a personal threat of an illness or disease, together with a person's belief in the effectiveness of the recommended health behaviour or action will predict the likelihood the person will adopt the behaviour [13]. This indicates a possible role of personalised evidence as a means of inducing desirable changes in behaviour.
Studies on diabetes preventive lifestyle activities largely focused on middle-aged and older adults. Similarly, majority of the interventions were on knowledge and skills with less emphasis on behaviour change [14]. Therefore, the present study is aimed at investigating non-diabetic young adults' risk of developing Type 2 diabetes mellitus, their attitudes and behaviours towards preventive lifestyle activities, and the effect of personalized evidence (diabetes risk score) on their reported attitudes.
The study was designed as a descriptive cross-sectional survey. It was conducted virtually, and the process was entirely online. The sample of 218 involved non-diabetic young adults living in middle eastern countries. Inclusion criteria were non-diabetic, non-pregnant young adults aged 20-39 years, who gave consent to participate in the study. Young adults living with diabetes mellitus, or those who did not give consent, and middle aged and older adults were excluded from the study.
The study took place over an eight-week period from January 2022 to the end of February 2022. Data was collected through an electronic questionnaire which consisted of a combination of two instruments namely, the WHO STEPS questionnaire (modified) [15] and the American Diabetes Association (ADA) [16] diabetes mellitus risk calculator.
A call to participate in the study was posted on social media (Facebook and Whatsapp). Consent was first obtained from interested persons who clicked on the study link. The participants were required to first read the informed consent flyer and then give consent (or otherwise) to participate in the study by checking a box on the electronic questionnaire, before proceeding to fill the rest of the questionnaire. Refusal to give consent led to automatic submission of the unfilled form. Completed forms were submitted electronically.
The study involved two parts: assessment of the attitude and behaviour of the participants towards some preventive lifestyle measures; and calculation of their risk of developing diabetes mellitus, which was done by having the participants fill an electronic copy of the questionnaire (English and Arabic language versions), which contained attitude and behaviour/practice (a modified version of the WHO STEPS questionnaire) and the ADA diabetes risk calculator. At the end of data collection, diabetes risk score was calculated for all the participants. They were then privately sent their individual scores, along with a short, pre-recorded screencast lecture titled “Risk of Developing Diabetes and Role of Lifestyle in Diabetes Prevention”. There was no post-intervention data collection for attitude as originally planned following preliminary analysis of the pre-intervention attitudes of the respondents.
Data obtained from the study was first cleaned. Incomplete responses were removed from the pool. Thereafter, the diabetes risk calculation was done for all the participants (including those whose ages were above the specified limit). Afterwards, the responses submitted by those with age limits outside the specified limit were removed from the pool. The data was analysed using Google Sheets (spreadsheet). Frequency distribution and proportions of sociodemographic, diabetes risk score, attitude, and behaviour variables were determined. A correlational analysis was done to compare estimated diabetes risk with age and BMI respectively.
Post data analysis, the estimated diabetes risk scores as well as a short educational video on diabetes risk and the role of lifestyle in diabetes prevention were sent by email to all the study participants.
Ethical approval was obtained from the Institutional (Ethical) Review Board of the Kuwait University, Kuwait (Assigned code: KU-EXT-21-12-29).
There were a total of 4,847 clicks on the survey link with a total number of 243 responses (5% response rate). After data cleaning, 213 responses were analysed. The mean age of the study participants was 31.3 years (S.D ± 5.5), and 127 (59.6%) were male while 86 (40.4%) were female.
A total of 126 (59.2%) of the respondents had bachelor's degree, 63 (29.6%) had a master's degree, 20 (9.4%) had completed high school, 3 (1.4%) had completed middle school, while 1 (0.5%) had completed primary school education.
One hundred and ninety (89.2%) of the respondents are Arabians, 9 (4.2%) are other Asians, 7 (3.3%) Africans, 6 (2.8%) did not state their ethnicity, while 1 (0.5%) is European/Caucasian. In the sample, 125 (58.7%) reported being married, 85 (39.9%) were single, while 3 (1.4%) indicated divorced. Fifty (23.5%) of the respondents reside in Iraq, 43 (20.2%) in Yemen, 33 (15.5%) in Lebanon, 22 (10.3%) in Kuwait, and 19 (8.9%) in Palestine. Others were from Saudi Arabia, Jordan, Egypt, United Arab Emirates, Oman, and Bahrain.
In terms of occupational distribution, 50 (23.6%) are in the healthcare sector, 40 (18.9%) in teaching and/or research, 30 (14.2%) in the administrative sector, 24 (11.3%) reported that they were not working or are housewives, 17 (8.0%) students, 17 (8.0%) in the business/finance sector, while 15 (7.1%) worked in engineering/science. Eight (3.8%) of the respondents worked remotely from home or were social media experts, 7 (3.3%) in unclassified occupations while 4 (1.9%) were engaged in the legal profession (See Table 1).
Table 1: Demographic characteristics of the study participants. View Table 1
The mean body mass index (N = 202) was 26.5 (± 5.1) kg/m2. Eighty-one (40.1%) of the respondents had optimal BMI, 69 (34.2%) were overweight, 36 (17.8%) had mild obesity, 8 (4.0%) had moderate obesity, 3 (1.5%) had morbid obesity, while 5 (2.5%) were underweight. A total of 113 (55.9%) indicated that they had a positive family history of diabetes mellitus while 89 (44.1%) did not. The mean calculated diabetes risk score (N = 202) was 2.8 (SD ± 1.3). Based on the interpretation of the ADA diabetes risk calculator, 187 (92.60%) of the study participants had low risk of developing diabetes while 15 (7.4%) had high risk of developing the disease (Figure 1a, Figure 1b and Figure 1c).
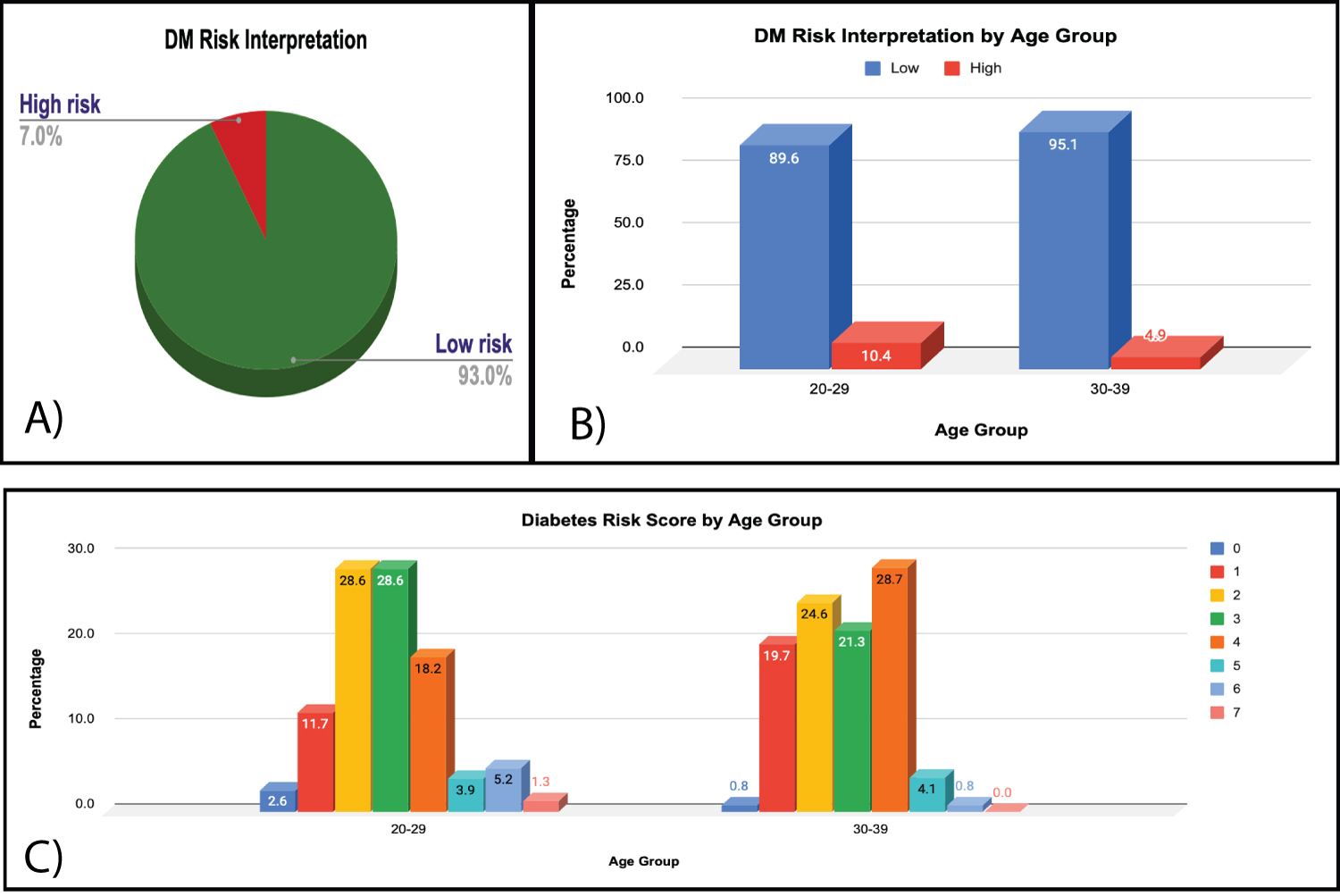 Figure 1: (a) DM risk interpretation; (b) DM risk interpretation by age group; (c) DM risk score by age group.
View Figure 1
Figure 1: (a) DM risk interpretation; (b) DM risk interpretation by age group; (c) DM risk score by age group.
View Figure 1
A total of 158 (74.2%) had checked their blood sugar with a health worker while 55 (25.8%) had never had their blood sugar checked. In all, 166 (77.9%) had never been told that their blood sugar was high while 47 (22.1%) had been told in the past that their blood sugar was high. In addition, 43 (21.3%) had ever been diagnosed with high blood pressure (hypertension).
With regards to attitude (N = 210), 185 (88.1%) agreed on the importance of maintaining a healthy lifestyle at a young age, 195 (92.9%) thought a healthy lifestyle would help them to stay healthy, and 180 (85.7%) disagreed that there was no need to maintain a healthy lifestyle at a young age (see Figure 2).
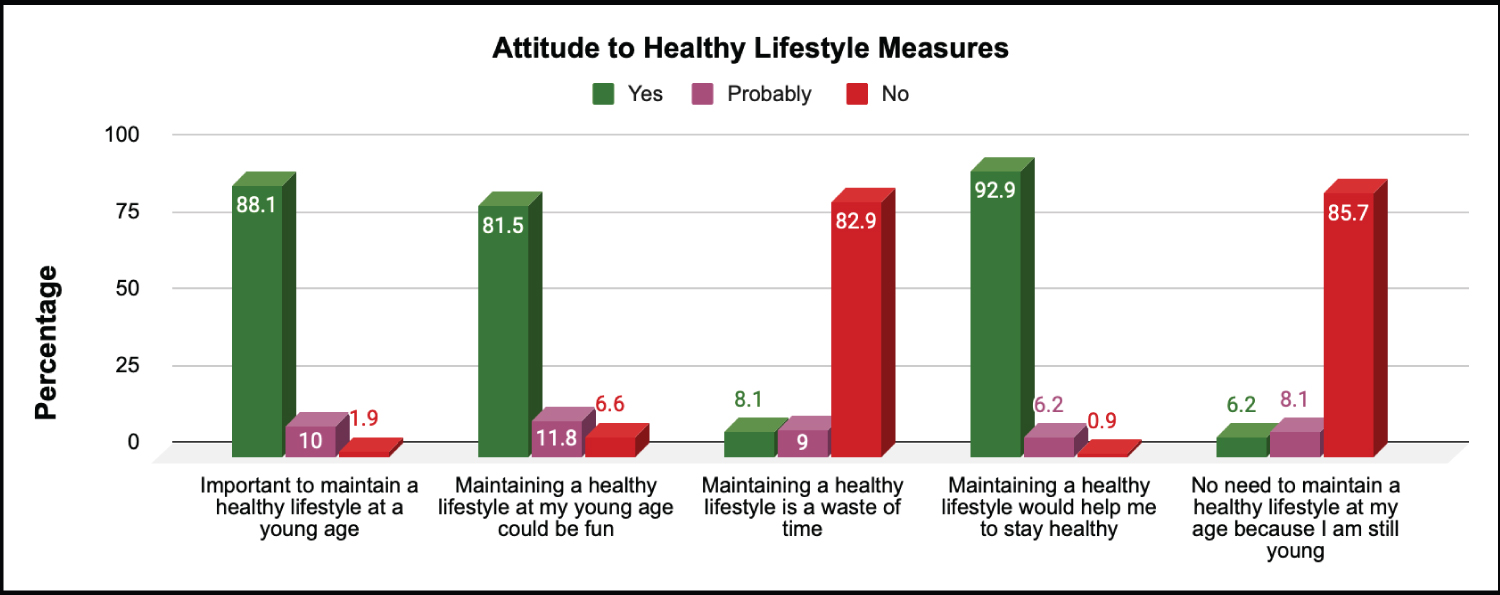 Figure 2: Attitude to healthy lifestyle measures.
View Figure 2
Figure 2: Attitude to healthy lifestyle measures.
View Figure 2
Concerning lifestyle behaviour (N = 213), in a week 81 (38.0%) of the respondents ate fruits on 2 to 3 days while 51 (23.9%) ate fruits on one day or not at all, 47 (22.1%) ate fruits on 4 to 5 days, and 34 (16.0%) ate fruits on 6 or all 7 days of the week. On the days fruits were eaten, 158 (72.8%) ate 1-2 fruit portions, 40 (18.8%) ate 3-5 fruit portions while 9 (4.2%) ate more than 5 portions per day. Eighty-one (38.0%) of the respondents ate vegetables 2-3 times per week, 67 (31.5%) ate vegetables 4-5 times while 46 (21.6%) ate vegetables on 6 days or all days of the week. On the days vegetables were eaten, 112 (52.6%) ate 2-3 portions, 62 (29.1%) ate one portion, 28 (13.1%) ate 4-5 portions, while 11 (5.2%) ate more than 5 portions (see Figure 3).
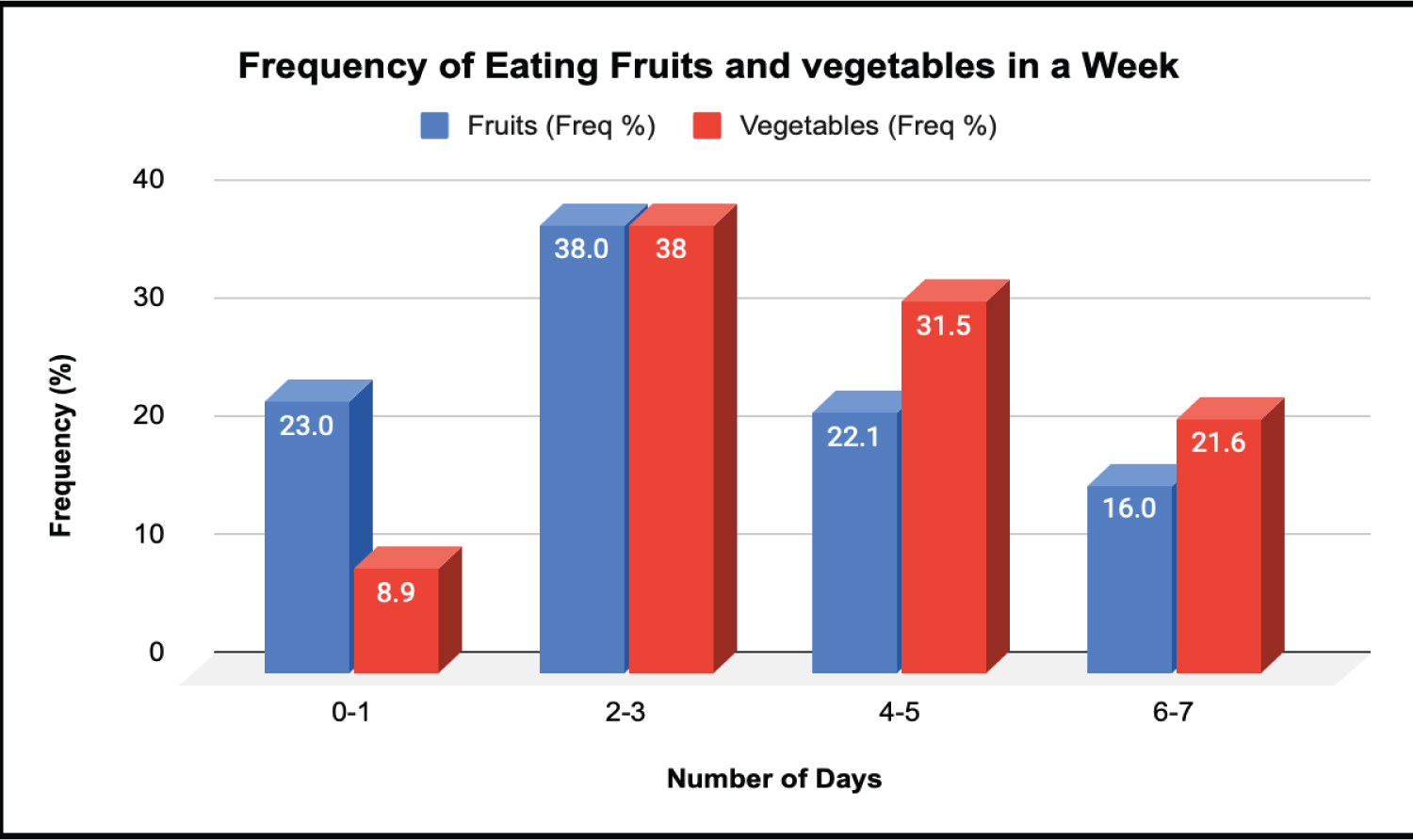 Figure 3: Frequency of eating fruits and vegetables in a week.
View Figure 3
Figure 3: Frequency of eating fruits and vegetables in a week.
View Figure 3
A total of 181 (85.0%) of the respondents indicated that their work did not typically involve vigorous-intensity activity that caused large increases in breathing or heart rate for at least 10 minutes continuously while 32 (15.0%) gave an affirmative response. Similarly, 151 (70.9%) indicated that their work involved doing vigorous intensity activities on 0 -1 days, 44 (20.7%) had the same on 2-3 days of the week, 12 (5.6%) on 4-5 days of the week, while 6 (2.8%) had same on 6-7 days of the week, and on such days, 157 (73.7%) of the respondents spent less than 30 minutes performing vigorous-intensity activities while 33 (15.5%) spent 30-60 minutes.
In all, 124 (58.2%) did not engage in work that involve moderate-intensity activity that causes small increases in breathing or heart rate for at least 10 minutes continuously, while 89 (41.8%) did. If done at all in a typical week, 97 (45.5%) indicated that they did moderate-intensity activities as part of their work on zero to one day, 74 (34.7%) on 2-3 days, and 132 (62.0%) were involved in this for less than 30 minutes per day while 56 (26.3%) for 30-60 minutes per day.
Among the respondents, 117 (54.9%) reported that they usually walked or used a bicycle (pedal cycle) for at least 10 minutes continuously to get to and from places while 96 (45.1%) indicated that they do not walk or use a bicycle for travel on a typical day. If done at all, in a typical week, 77 (36.2%) did this for zero to one day, 57 (26.8%) for 2-3 days, 52 (24.4%) for 4-5 days, and 27 (12.7%) for 6-7 days. For each day, 139 (65.3%) spent less than 30 minutes, 58 (27.2%) spent 30-60 minutes, while 8 (3.8%) spent 61-90 minutes walking or cycling.
In the same vein, 158 (74.2%) indicated that they do not do any vigorous-intensity sports, fitness or recreational (leisure) activities that cause large increases in breathing or heart rate for at least 10 minutes continuously, while 55 (25.8%) indicated that they do. If done at all, in a typical week 150 (70.4%) did this for zero to one day, 42 (19.7%) did for 2-3 days, 18 (8.5%) for 4-5 days while 3 (1.4%) did for 6-7 days of the week. Meanwhile, 164 (77.0%) did for less than 30 minutes, 37 (17.4%) for 30-60 minutes, and 8 (3.8%) did for 61-90 minutes on any day.
It was found that 139 respondents (65.3%) indicated that they did not usually do any moderate-intensity sports, fitness or recreational (leisure) activities that cause a small increase in breathing or heart rate for at least 10 minutes continuously, while 74 (34.7%) indicated that they did. If done at all, in a typical week, 147 (69.0%) indicated that they did so on zero to 1 day of the week, 47 (22.1%) did so on 2 to 3 days of the week, 14 (6.6%) on 4 to 5 days of the week, while 5 (2.3%) did so on 6 to 7 days of the week. On the said days, 161 (75.6%) indicated that they spent less than 30 minutes, 40 (18.8%) spent 30-60 minutes, while 10 (4.7%) spent 61-90 minutes doing moderate-intensity sports, fitness or recreational (leisure) activities (see Figure 4 and Figure 5).
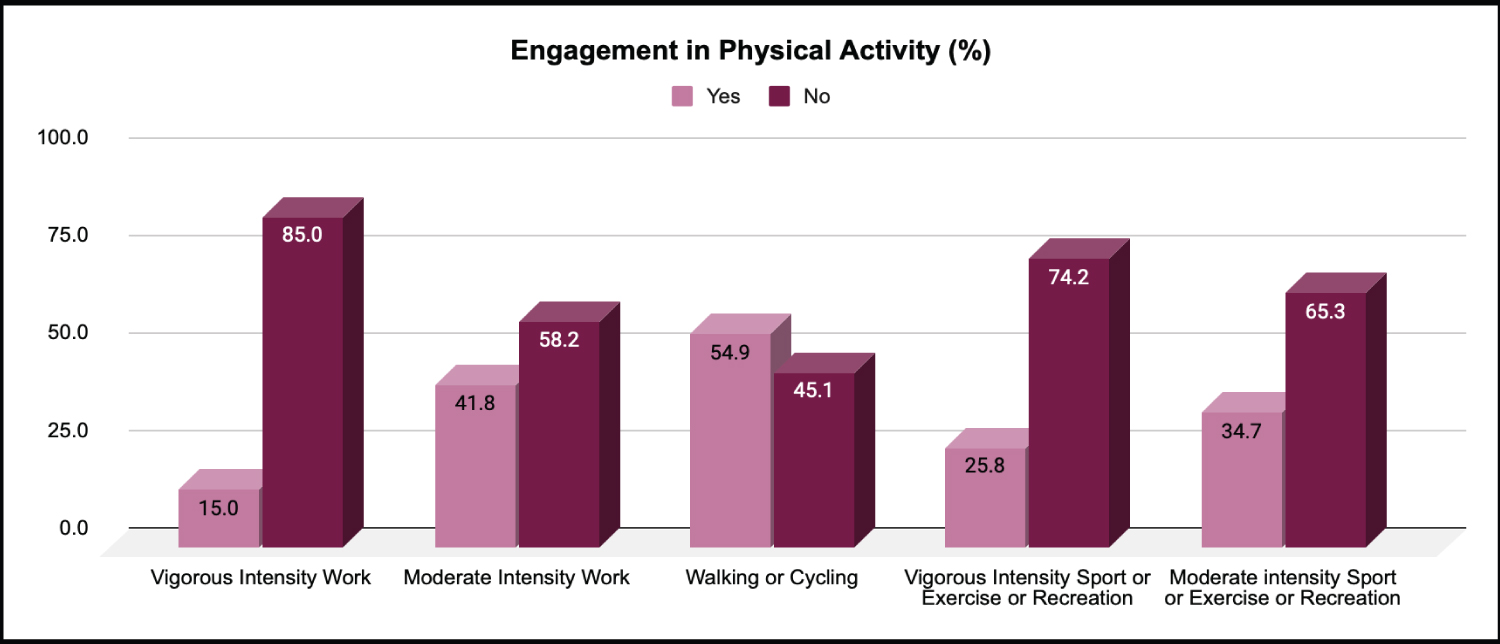 Figure 4: Engagement in physical activity.
View Figure 4
Figure 4: Engagement in physical activity.
View Figure 4
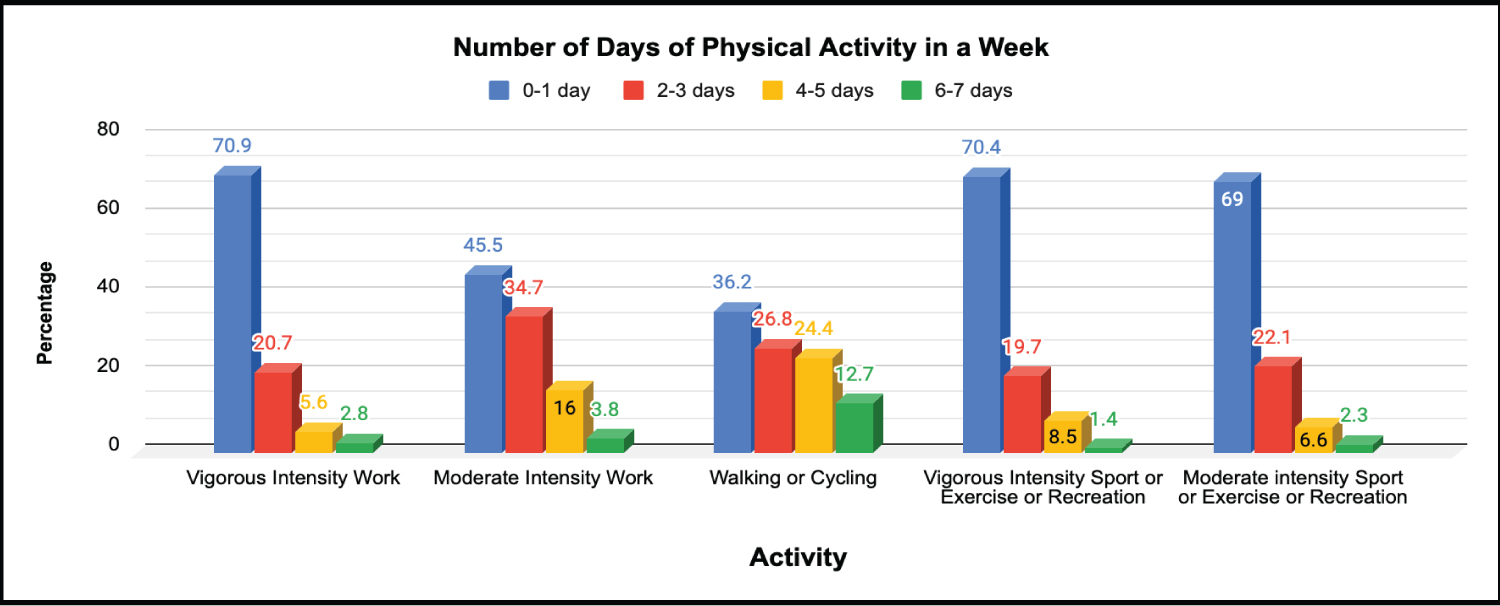 Figure 5: Number of days of physical activity in a week.
View Figure 5
Figure 5: Number of days of physical activity in a week.
View Figure 5
There was a weak and negative correlation between age and diabetes risk score (r = -0.1) while body mass index was positively correlated with diabetes risk score (r = 0.63).
Type 2 Diabetes is a preventable chronic condition that has become one of the leading causes of death globally [17]. The risk factors that are associated with this chronic condition can be managed individually or collectively with functional strategies. Although this study was not able to demonstrate it, the influence of personalised evidence on attitude and behaviour change generally has been supported by literature [13]. Majority of the participants, both in the 20-29 years and the 30-39 years age groups had low risk of developing Type 2 diabetes mellitus, and this corroborates current evidence that the risk of developing diabetes increases from age 45 years and above. However, the results showed that the respondents were overweight. Most of the participants were male and above 30 years of age.
Despite the reported positive attitude towards preventive lifestyle measures by most of the respondents, their collective attitudes did not correspond to their reported lifestyle behaviours/practices. The salient finding can negatively impact the possibility of achieving positive outcomes through individual or self-care management approaches as have been demonstrated [1]. For instance, since its introduction in England in 2016 the NHS Diabetes Prevention Programme (DPP), a national type 2 diabetes prevention programme targeted at persons with prediabetes, resulted in a reduced incidence of the disease [18]. Participants in the 9-12 month programme were 18 years and above, and were eligible for enrolment in the programme if a recent blood test showed a concentration of HbA1c within the range of 42-47 mmol/mol (6.0-6.4%) or fasting plasma glucose (FPG) level of 5.5-6.9 mmol/L, and then had to attend about 13 group-based behaviour change sessions which were said to have incorporated structured education on nutrition, physical activity and weight loss. In their evaluating impact of the NHS DPP programme on the incidence rates of type 2 diabetes mellitus, the researchers demonstrated significantly consistent lowering of the incidence rates at the various phases of the study. However, they suggested a longer follow-up to ascertain the sustenance of this observation or determine if the impact is actually a delay in the onset of the disease.
Findings from this study revealed that the respondents were overweight on average and did not meet the recommended lifestyle practices in all the parameters examined. For instance, unhealthy diet and lifestyle, high level of cholesterol, lack of exercise, and obesity or being overweight are among the preventable yet common risk factors associated with the incidence of diabetes mellitus [19]. Furthermore, evidence indicates that an active lifestyle lowers blood sugar levels [20,21]. The suboptimal level of healthy lifestyle behaviour/ practices may explain the overall prevalence of overweight among respondents in the present study. The positive attitude towards preventive lifestyle measures reported by the respondents in the present study may in the opinion of the researchers, be attributable to response bias due to an abundance of information about healthy lifestyle measures from social media.
Based on the reviewed literature, two possible ways to address the discrepancy between reported knowledge and the behaviour towards healthy lifestyle activities are apparent. The first suggested approach is a possible need to review existing patient and family educational intervention methods and adopt the methods of programmes with proven success, such as the Feel4Diabetes® Intervention programme [22]. The multi-centre (country) school and community-based programme approached diabetes prevention through promoting a healthy lifestyle and reducing obesity. The programme involved a combination of approaches that included counselling sessions, simple educational leaflets, and assisting the participants in setting “SMART” goals that were based on the programmes core goals. At the end of the first year, there was statistically significant evidence of a reduction in daily consumption of sugary drinks and sweets, reduced daily screen time, increased consumption of breakfast and fruits, and increased water intake.
The second approach involves targeted efforts to improve adherence to healthy lifestyle behaviours. This might entail adopting measures that will consciously motivate individuals to perform the desired healthy lifestyle activities, as demonstrated by the impact of the NHS DPP [18]. Examples of this approach are as utilised by Huo, et al. [23] in the Cardiovascular Health and Text Messaging (CHAT) and the CHAT-Diabetes Mellitus (CHAT-DM) studies. These are two ongoing trials with the goal of improving secondary prevention of coronary heart disease by means of simple and cost-effective messaging technologies among patients in China that are living with coronary heart disease, with or without diabetes mellitus. This is supported by previous studies that established that change in Body Mass Index (BMI) and level of physical activity are part of their primary outcomes. The simple method can also be extended to primary behavioural change-focused diabetes prevention activities for young adults.
Based on preliminary findings from this study, the influence of personalized evidence on the attitude and behaviour of the respondents towards healthy lifestyle activities was not measured. However, evidence from this study indicates that most young adults have desirable attitudes towards healthy lifestyle measures as recommended by current health guidelines. However, the attitudes did not align with their behaviours in terms of practising the recommended healthy lifestyle measures. The implication is an increased risk of developing Type 2 diabetes mellitus. Therefore, effective alignment of lifestyle behaviour with attitude would require modification of lifestyle practices or intervention education provided by physicians, psychologists, and other healthcare workers to young adult patients, in a bid to facilitate greater adoption of recommended healthy lifestyle behaviours, and ultimately prevent the onset and reduce the incidence or delay progression from pre-diabetes (high risk) to Type 2 diabetes mellitus.