Diagnosing the cause of abdominal pain in a young type 1 diabetic can be a challenging task and involves a wide array of differential diagnosis. Most commonly the pain is thought to be secondary to diabetic neuropathy. It becomes even more problematic if there is significant weight loss, if extensive investigations have not found any organic pathology and if the pain does not fit into any pattern of diabetic neuropathy.
We present such a case where a young 21-years-old female diabetic had lost 16 kgs in 6 months due to diffuse left sided abdominal pain with radiation to the back. It was also associated with a very poor diabetic control with a HbA1C of 150 mmol/l. Despite trying a wide variety and combination of different pain killers (Amitriptyline, Paracetamol, Codeine, Duloxetine, Pregabalin, TENS machine, oral Morphine and Tramadol), there was no relief and the patient continued to lose weight. The investigations which included Short Synacthen test, contrast CT of the abdomen/pelvis, MRI of the abdomen, capsule endoscopy, OGD (with normal duodenal biopsies) and MRI of the spine were all normal. Also anti TTG antibodies were negative.
She proceeded to have Left iliopsoas muscle block after liaising with the pain control team. This resulted in complete resolution of the pain. She began to regain the lost weight and her weight has remained stable at 49 kgs.
This was a case of iliopsoas syndrome masquerading as a surgical pathology.
Type 1 diabetes, Abdominal pain, Iliopsoas syndrome, Weight loss, Hidden prankster
The Differential diagnosis of abdominal pain in a patient with Type 1 Diabetes is wide. We present a medical case masquerading as surgical pathology in a young type 1 diabetic individual.
A young 21-years-old female type 1 diabetic patient had presented with significant weight loss (16 kgs over 6 months), decreased appetite, constipation, nausea and anxiety. The pain was diffuse affecting the whole left side of the abdomen with radiation to the back and persisting throughout the day. The pain character was throbbing, aching or stinging in nature. It was associated with nausea and constipation. The pain killers tried included Amitriptyline, Paracetamol, Codeine, Duloxetine, Pregabalin, TENS machine, oral Morphine and Tramadol but with no relief. She was being seen in the pain clinic and also by the dieticians. Diabetes control at presentation was suboptimal with a HbA1c of 150 mmol/mol. She was admitted and investigated for the abdominal pain and weight loss. Eating disorder was ruled out.
Clinical examination revealed non peritonitic left sided abdominal pain with normal bowel sounds along with touch dysesthesia. Surgical opinion was sought and Inflammatory bowel disorder was considered. The investigations which included Short Synacthen test, contrast CT of the abdomen/pelvis, MRI of the abdomen, capsule endoscopy, OGD (with normal duodenal biopsies) and MRI of the spine were all normal. Also anti TTG antibodies were negative.
She proceeded to have Left iliopsoas muscle block. This resulted in complete resolution of the pain and her weight has remained stable at 49 kgs.
This was a case of iliopsoas Syndrome masquerading as a surgical pathology.
Knowing the anatomy of the iliopsoas muscle is essential to understand the iliopsoas syndrome. The iliopsoas muscle is part of the inner hip muscle group and is the major flexor of the hip [1,2]. It is the combination of the psoas major and iliacus muscle. Both muscles have different areas of origin. It is the only muscle that connects the lumbar spine and the lower body.
Iliacus muscle extends from the upper two thirds of the iliac fossa, descends to attach to the tendon of psoas major. Some of the fibres of the iliacus muscle attaches directly to the lesser trochanter. The psoas major muscle originates from the first four lumbar vertebra, the costal process of the lumbar vertebra and from the twelfth thoracic vertebra. The psoas major muscle inserts into the lesser trochanter and is innervated dorsally by the genitofemoral nerve. Medial to the psoas major muscle lies the sympathetic trunk. Both muscles unify just above the inguinal ligament in the lateral pelvis. They travel through the muscular lacuna along with the femoral nerve [1]. The iliopsoas is a deep seated core muscle and is the strongest flexor of the hip joint. It is completely surrounded by the iliac fascia. It is important for walking, supporting the back, for maintaining upright posture due to its attachment along the spine and helps in extending the lumbar spine. It is innervates by the lumbar plexus [3] (Figure 1).
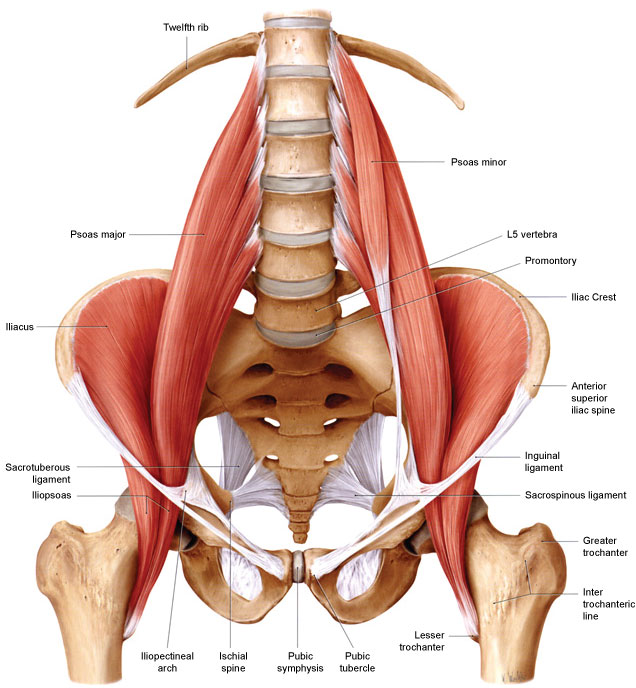 Figure 1: Iliopsoas muscle.
View Figure 1
Figure 1: Iliopsoas muscle.
View Figure 1
Iliopsoas syndrome is an under reported and under diagnosed medical problem. It is caused when there is damage to the iliopsoas muscle or when spasm results in the muscle when it is overworked or too weak to handle the stress imposed on it. Another reason for the dysfunction is when the muscle shortens on prolonged sitting, it gets adapted to the normal length making it difficult for the contractile units of the muscle i.e., namely the sarcomeres to get back to its normal length. A chronically contracted muscle can result in ischemia, trigger points which refer pain, distorted movement, compensation of other regional muscles and nerve entrapment (femoral nerve, the lateral femoral cutaneous nerve, the femoral branch of the genitofemoral nerves, the iliohypogastric nerve and the ilioinguinal nerve). The compensation of the other regional muscles can result in misalignment of the spine causing disc herniation typically at L4 - L5 and possible irritation of sciatic nerve.
It can be hard, difficult to diagnose condition and is often referred to as the hidden prankster [2]. As the muscle lies internally, it is accessible only through a small area on the surface namely the femoral triangle. The pain distribution is vast and it can be felt in the lower abdomen, groin, hips, buttocks, back and hip. It can also be part of the iliopsoas tendinitis due to repetitive use. Pain is usually experienced on standing from a sitting posture. There is usually no pain on standing, walking or lying down. Leg extension can worsen the pain as in driving [4].
Diagnosis can be made via ultrasound. MRI and CT scans have limited applications [5]. Treatment is mainly conservative in the form of stretching and hip rotation exercises. Iliopsoas muscle block as in our patient is a very successful in most patients. Other options include injections of muscle relaxant (Botulinum toxin type A) and steroids (methylprednisolone) [5].
I would like to thank Dr. Kofi oboubie, my consultant at the Royal Gwent Hospital who helped me in the preparations. I also take this opportunity to thank the patient who was very patient, engaging and very cooperative.
The authors declare that there is no conflict of interest.
None.