Deaths and disabilities due to the lack of proper Emergency Medical Rescue Services (EMRS) is a global public health concern, also in Dhaka city, Bangladesh. The study aimed at contributing to improve the EMRS in Dhaka city by assessing and identifying major shortcomings with possible solutions.
The study was conducted in July/August 2017, after analyzing medical and relevant records, a one week observational study was conducted in 4 purposively selected hospitals in Dhaka city. The Mode of transport to the emergency centre and delay times were determined by observing and assessing medical records of the incoming patients. Information on the management of incoming emergency calls and trips of the ambulances were also documented. Satisfaction and perceived experience with the services was investigated by in-depth interviews of 56 patients relatives. 23 EMRS providers and managers were interviewed for their perceptions and recommendations.
Our document analysis of 2 study hospitals in Dhaka showed that 45.9% of total deaths (N = 13707) in 2014 were due to cardiovascular diseases, road traffic incidents, other accidents, and suicides. During the observation in 4 study hospitals, only 11.3% of the 734 emergency patients used ambulances to get to hospital, while 63% used rickshaws/motor-rickshaws and 25.8% bus/car. 55.6% of emergency patients got to hospital after 60 minutes/later after start of symptoms (median delay 120 minutes; range: 40-2880 minutes). The median delay of ambulances (call to hospitalization) was 85 minutes (day-time 102 minutes; night 45 minutes). On emergency request only 23.6% of the 127 callers, a hospital ambulance was sent to the patient, while the other cases were not supported due to unavailability, long distance, and high fare issues of ambulance. Ambulances were used in only 10.7% of their available time for transporting patients. Ambulances were poorly equipped (unskilled driver, oxygen and rarely with first aid box). Satisfaction level about current services among patients relatives was low (only 1.8 on a scale of 4; N = 56). Major reasons of their not calling for an ambulance at emergencies were unavailability (67.3%) and unknowing phone number (51.9%). EMRS providers and managers complained about the poor structure of EMRS. Major concerns were: Policy deficit, corruption, no coordination centre with unique phone number, poor ambulance services, and traffic-jams.
To reduce the number of deaths and disabilities, Dhaka needs to upgrade and improve its EMRS through a step-by-step process of telephone assisted emergency first responders led pre-clinical care.
Emergency medical services, Pre-clinical care, Medical rescue services, Ambulance services, Bangladesh
Deaths, disabilities and human suffering due to the lack of proper Emergency Medical Rescue Services (EMRS) at emergency situations have become a global public health concern. In 2019, of the estimated 55.4 million global deaths, 73.6% were related to non-communicable diseases (NCDs), 18.4% were caused by communicable diseases (CDs) along with maternal, neonatal and nutritional problems, and 8.0% were due to injuries [1]. Many of these global deaths were in the category of emergency medical situations, particularly cardiovascular diseases (CVDs; 17.9 million deaths) and injuries (4.4 million deaths) including road traffic incidents (RTIs; 1.3 million deaths), that required immediate and efficient pre-clinical intervention [1,2].
The mortality was much higher in low, middle, and upper-middle income countries (80.7% of all deaths; 86.4% of all injuries and 92.3% of all RTIs; 77.0% of all NCDs and 81.6% of all CVDs; 93.1% of all CDs) than in high income countries (HICs) [1,2]. Many studies in the HICs showed that immediate resuscitation with efficient professional basic first aid and advanced life support pre-clinical care and rapid transportation from the scene of an incident to an appropriate hospital could provide timely and effective clinical care and could prevent a large numbers of deaths and disabilities [3-6]. In low and middle income countries (LIMICs), there is paucity of focus on emergency care in pre-hospital and intra-hospital health care settings, which are ill-equipped and unorganized to offer appropriate, immediate and efficient professional rescue care with first aid in emergency situations and resulting in a high burden of preventable deaths and disability [2,7-11].
In Bangladesh, of the total estimated country-wide deaths in 2019 (630.0 deaths per 100,000 population), 75.2% were related to NCDs (38.1% were with CVDs), 18.8% to CDs and 6.1% to injuries including RTIs (2.7%) respectively, and many of them occurred as medical emergency situations [1]. Stroke, ischaemic heart diseases and RTIs were the three reported top reasons for deaths and disabilities in Bangladesh [1,12-15]. The mortality rate due to Stroke, ischaemic heart diseases and RTIs were 82.3, 66.6 and 15.3 respectively per 100,000 populations, and these were causing additionally 1792.5, 1563.9 and 1062.9 disability-adjusted life years (DALYs) respectively per 100,000 population in Bangladesh in 2019 [1].
Bangladesh is the world's 8th densely populated country with 166.1 million populations in 2021 [16]. Dhaka, the capital city of Bangladesh, is one of the world's largest and most densely populated megacities with 20.3 million populations in 2021 [16]. The degree of mortality and morbidity due to NCDs, CDs, RTIs and other forms of accidents (e.g., building collapse, fire, gas explosion, occupational accidents) is rising in accordance with the process of urbanization, including the rapid increase of traffic [12,14,17,18].
EMRS care is supposed to offer high quality pre-clinical care to preserve and prevent deaths and disabilities from different medical emergencies [2,19-21]. An EMRS includes a primary system (pre-clinical care that is directly saving life outside the hospital) and a secondary system (transport of patients from one hospital to another) [19]. Modern pre-clinical care should have six stages of high quality pre-clinical care as shown in Figure 1 [19,22]. It should be operated by a coordination centre with a universal call number [2,19,21]. The process will start after receiving a phone call from the accident or emergency scene [2,19,21]. Then a rescue team equipped with supporting medical facilities will be deployed by the coordination centre to perform the rescue services [2,19-21]. The rescue team might be any of three types of teams or services: (1) Ambulance with paramedics, (2) Ambulance with emergency doctors and paramedics, and (3) Rescue team with helicopter [2,19,20]. The success and operational effectiveness of the system depends on the collective and collaborative action of the model Figure 1.
 Figure 1: Six key stages of a modern EMRS care [22].
View Figure 1
Figure 1: Six key stages of a modern EMRS care [22].
View Figure 1
In view of the outstanding importance of EMRS particularly in densely populated cities, it was the aim of the study to contribute to improving the existing EMRS by identifying major shortcomings in the current system in Dhaka city and identifying possible solutions. The specific objectives of our study were: (1) To analyze the mortality and morbidity due to different medical emergency situations; (2) To review and explore the current EMRS with their operational effectiveness and difficulties in Dhaka city; and (3) To assess the acceptance and perceived effectiveness of existing EMRS by EMRS providers and users.
The research was conducted in Dhaka city during July and August 2017 including a one-week observational study in each of four selected local hospitals (two public and two private). The hospitals were: Dhaka Medical College Hospital (DMCH), National Institute of Traumatology and Orthopaedic Rehabilitation (NITOR), Bangladesh Medical College Hospital (BMCH), and Ad-din Medical College Hospital. One additional hospital (Anowar Khan Modern Medical College Hospital) refused to participate.
For the selection of hospitals and study participants, purposive sampling techniques were applied. The sample size of in-depth interviews with relatives of emergency patients was 56 and with EMRS service providers and managers it was 23.
Local hospitals' medical records: The two private hospitals were not able to provide the one year mortality and admission records. In the two public hospitals their published mortality and admission data in 2015 were used which could be retrieved from the Bangladesh Health Bulletin 2016 [23,24].
Published and unpublished reports and articles: Relevant information, reports and articles were collected from different online sources (mainly Google Scholar and stakeholders' websites). Relevant key words on EMRS were employed: emergency, medical, rescue, ambulance, services, pre-clinical care, diseases, accidents and injuries, mortality, morbidity, Dhaka, Bangladesh.
Photo documentation: Photos were taken during the field work to visualize important EMRS issues.
Participant observations about EMRS: Participant observational measurements were conducted for one week in each hospital using an observational checklist to scrutinize the hospital's ambulance and emergency medical services. Each day one shift was covered followed by the cycle of morning, evening and night shift during the week. The numbers and details (e.g., medical reasons, means of transports, delay times, demographic data) of emergency patients who arrived at the emergency room were recorded during the shift. Incoming patients were observed and the notes by doctors and nurses were checked. During the working shift, the management of incoming emergency calls and deployment of hospital ambulances were observed and documented. The delay times (from incoming call to return of the ambulance) of medical rescue trips of the hospital ambulances were measured. In addition, the management and delay times of 17 purposively selected medical rescue operations (from incoming call to return of the hospital) that were transported by the hospital ambulance were observed and analyzed.
In-depth interviews with emergency patients' relatives: 56 interviews with relatives of emergency patients were carried out in a separate room of the hospital to know about their experience and perceptions of EMRS in Dhaka. After receiving informed consent the interview was conducted applying the data collection guidelines. The duration was on average about 30 minutes.
In-depth interviews with EMRS service providers and managers: 23 in-depth interviews with representatives of local hospitals and other organizations dealing with emergency operations in Dhaka city were conducted using interview guidelines. The duration of the interview ranged from 30 to 60 minutes. Potential service providers and managers were purposefully selected according to their importance and relevance and were contacted for an appointment for the interview.
Translation of the data collection forms: Data collection instruments were not translated in to the local language (Bengali) as the principal and assistant researchers speak the language.
A descriptive data analysis method was applied. Frequencies were computed with SPSS 18.0 and Microsoft Excel 2007. For the time analyses, the medians were computed because the data were not normally distributed.
This study was conducted in strict compliance with the ethical principles of the Nuremberg Code and the Declaration of Helsinki [25,26]. The study was approved by the Ethic Committee of Freiburg University, Germany (Approval No. 165/17) which was accepted by the participating hospitals in Bangladesh. Written informed consent was obtained from the participating hospital authorities and emergency patients' relatives. Whenever - in exceptional cases - a selected participant refused to continue the interview, it was ended immediately.
The two public hospitals in our study recorded in 2014 a total of 1,286,226 patient visits at outpatient department (915772, 71.2%) and emergency department (370454, 28.8%) [23,24]. Of all 16,0351 admitted patients in 2014 to the two public hospitals, 11.5% (18,381) were due to RTIs followed by CVDs (9,124, 5.7%), other accidents and injuries (7,343, 4.6%), suicidal attempts (3,817, 2.4%), and pregnancy complications (1,837, 1.2%) [23,24]. The remaining admissions (119849, 74.7%) were due to other non-communicable and communicable diseases [23,24].
The two public hospitals recorded in 2014 a total of 13,707 deaths. CVDs (16.6%) were the most frequent cause followed by RTIs (12.6%), other accidents and injuries (11.3%), and suicidal attempts (5.4%; Figure 2). These most frequent causes of deaths accounted for 45.9% (6296) of the total deaths. The remaining deaths (7411, 54.1%) were due to other non communicable and communicable diseases. Three percent of deaths occurred in under-fives; the male to female mortality ratio was 1.3:1.0 [23,24].
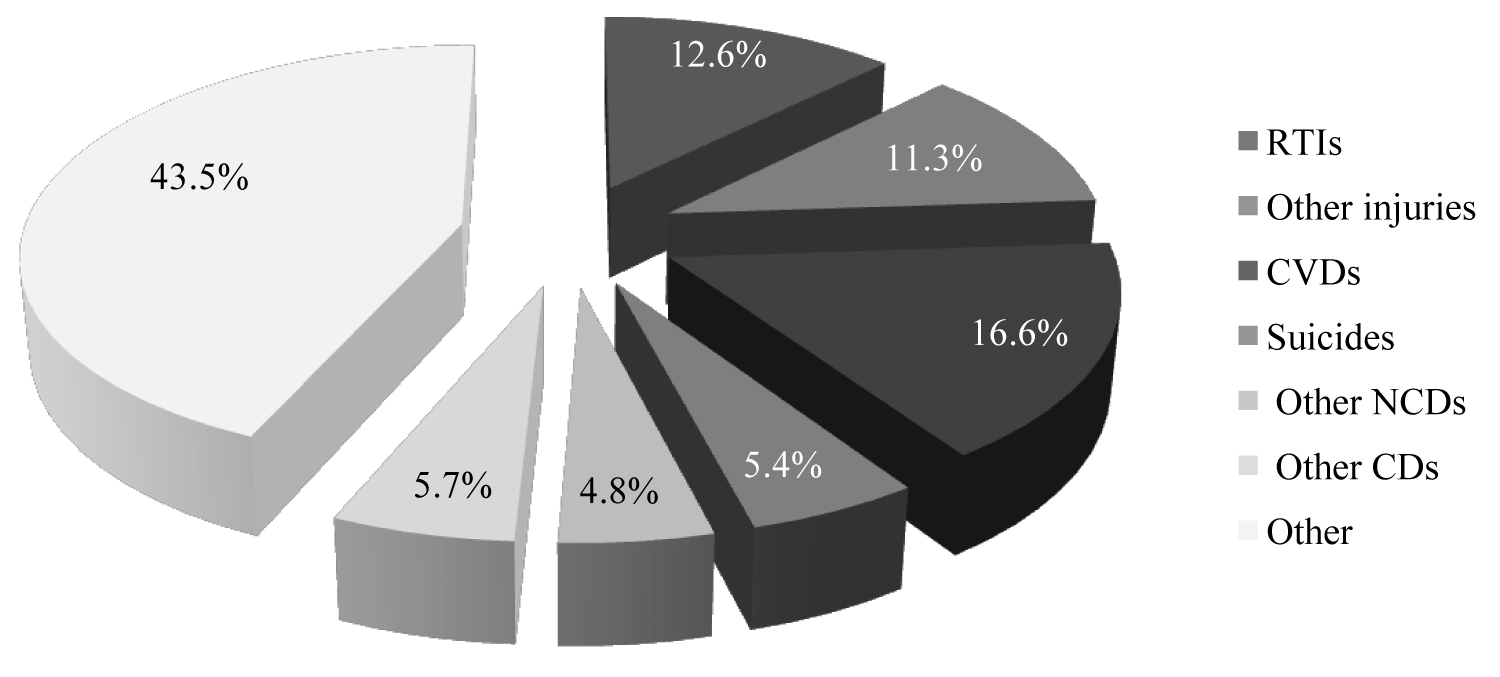 Figure 2: Causes of death (%) in two public hospitals in 2015 in Dhaka city (N = 13,707 deaths [23].
View Figure 2
Figure 2: Causes of death (%) in two public hospitals in 2015 in Dhaka city (N = 13,707 deaths [23].
View Figure 2
However, during the observation periods in July/August 2017, 1 shift per day, overall, 734 emergency patients were recorded in 4 hospitals. Reasons for coming to the emergency centre were different accidents and injuries (438; 59.7%), RTIs (139; 18.9%), and CDs (83; 11.3%) to be the most frequent causes for admission to emergency departments; other reasons were pregnancy complications (20, 2.7%), other NCDs (14, 1.9%), CVDs (13, 1.8%) and other medical emergencies (27, 3.7%). The male to female patient ratio was 1.98:1.00. 22.2% (163) of emergency patients were below 18-years-old, 74.8% (549) in the age group of 18-65 and 3% were over 65 years. The median age of emergency patients was 27.0 years (range: 1 to 90 years).
Emergency call services: Since 2017, the Government of Bangladesh (GoB; Bangladesh Police) has been launching the national emergency call centre with a universal phone number 999 to support people in urgent need with police, fire, ambulance and other services [27], but there was no central call centre with universal phone number on EMRS in Dhaka city. The individual hospitals were responsible for emergency call care including medical transport (ambulance) service. Only one hospital out of four had a call center but not with a universal phone number. GPS was used only for tracing the ambulance location. In the other three hospitals ambulance service were operated by the emergency department.
Hospital ambulance services: In Dhaka city the availability of ambulances was estimated to be 2.8 per 100,000 inhabitants (in total 53 ambulances in 4 hospitals; Table 1). According to our interviews with EMRS providers and own observations, the ambulances are equipped with a driver, oxygen and rarely with a first aid box, but with no other facilities and no paramedics or supporting staff (Photo 1). Ambulance drivers are not trained in emergency care.
 Photo 1: Equipment of ambulances (only oxygen, no other facilities; source: was taken during field work).
View Photo 1
Photo 1: Equipment of ambulances (only oxygen, no other facilities; source: was taken during field work).
View Photo 1
Table 1: Ambulance services and its use in 4 hospitals in Dhaka city, Bangladesh. View Table 1
The fare is fixed at a price corresponding to approximately 3.4 Euros in the public hospitals, while in private hospitals it was 3.4 to 10.3 Euros (based on distance; Table 2). Ambulance services have to be paid from out-of-pocket money as private or public insurance does not exist in the hospitals (see users' information about ambulance costs below).
Table 2: Cost estimates of ambulance services during 7 days in 4 hospitals in Dhaka city. View Table 2
Ambulance management costs (e.g., maintenance cost of ambulances, changing of oil filters, changing of filters or of the oxygen supply, salaries for ambulance drivers and other related staff) were collected from the study hospitals. Based on the operational costs and number of transported patients (either bringing emergency patients to hospitals or discharged patients home), it was estimated that per EMRS rescue operation the expenditure was about 8 Euros (Table 2). The transport cost was 19 Euros per emergency patient (for incoming patients and referrals).
Incoming emergency call services: During the four-week (1 shift per day) observation period in 4 study hospitals, we assessed a total of 127 incoming emergency calls searching for an ambulance in hospitals' call centre or/and emergency departments (Table 3). Frequent patients' medical reasons of these callers were: pregnancy complications (53, 41.7), RTIs and other accidents and injuries (35, 27.6%); CVDs (19, 15.0%), asthma (7, 5.5%), and other medical reasons (13, 10.2%). Only 23.6% (30) of the 127 callers received the hospital ambulance service. Additionally for 18.1% cases, only the information on private ambulance service was provided without sending a hospital ambulance. Major reasons for not deploying an ambulance to patient transport care of the 97 callers were: Unavailability (71.1%), long distance (43.3%), and high fare (29.9%).
Table 3: Management of incoming calls at medical emergencies during 7 days in 4 hospitals in Dhaka city, Bangladesh. View Table 3
Use of hospital ambulance services: The observational study also focusing at ambulance services showed that only one hospital was transporting the emergency patients with an ambulance. The other three hospitals used ambulances exclusively for transferring or discharging patients. In total only 0.5% of the emergency patients were transported by hospital ambulances (Table 1). Ambulances were used only for about 10.7% of their available time for transporting patients (either for bringing discharged patients home -58.5%- or for bringing them to another hospital -41.5%); 89.3% of the available ambulance time was used for other purposes (e.g., to transport hospital staff or to bring medicine, food or supplies) or the ambulances were just in-active in a garage.
Transport media to get to the hospitals' emergency department: The means of transport of 734 emergency patients were observed and recorded at the emergency room during 7 days, 1 shift per day, it was found that only 11.3% (83) of them came by ambulances and 88.7% (651) had used local transport (Figure 3). 62.9% (462) of emergency patients used rickshaws (273, 37.2%) or motor-rickshaws (189, 25.7%) to get to the hospital. The remaining 25.8% (189) of the emergency patients arrived in the hospital by car (112, 15.3%; own 12.0% and rent 3.3%) or bus (77, 10.5%).
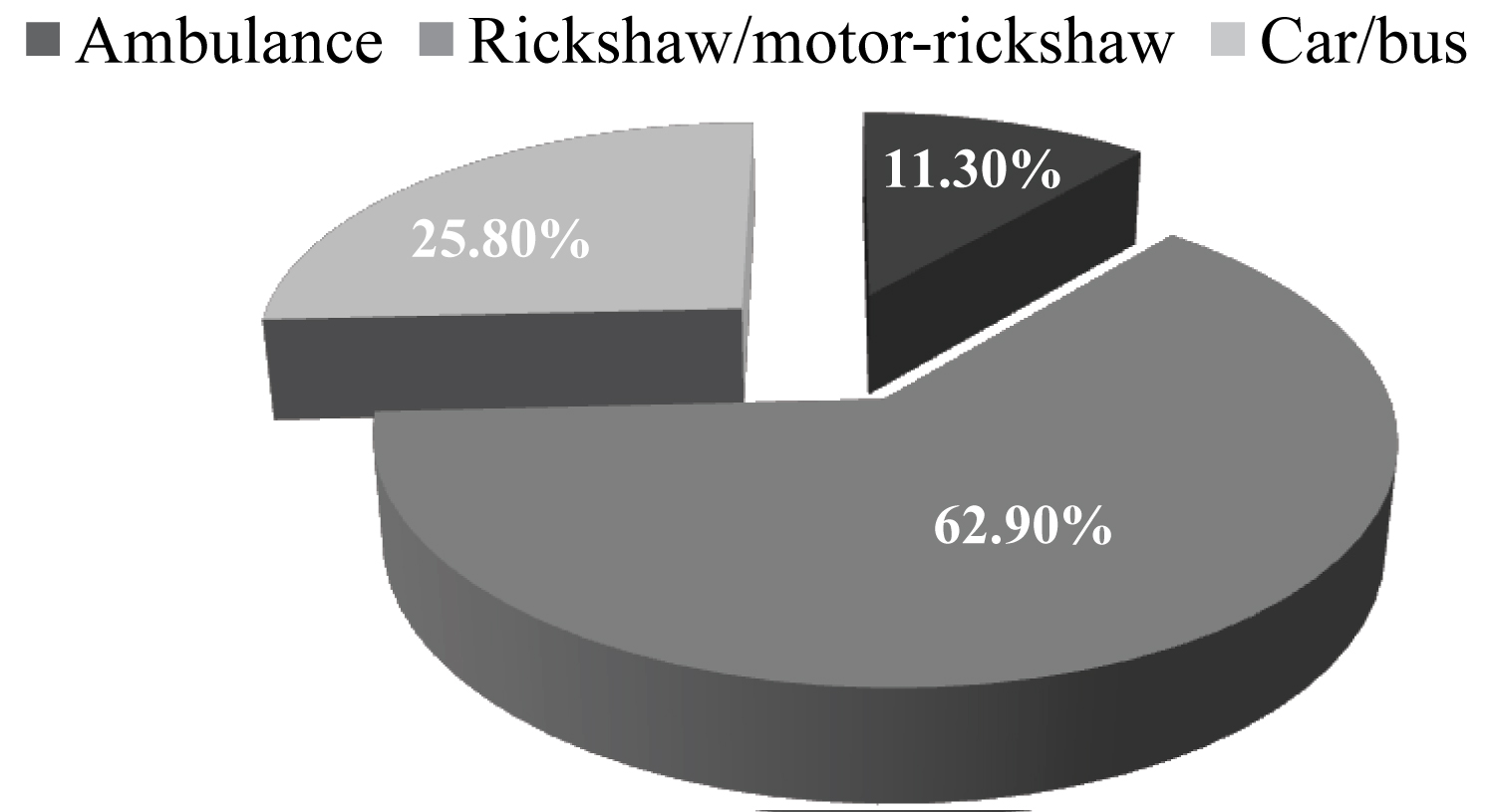 Figure 3: Type of transport used by emergency patients in study hospitals (N = 734).
View Figure 3
Figure 3: Type of transport used by emergency patients in study hospitals (N = 734).
View Figure 3
Of the 83 patients arrived at the hospitals by an ambulance, 32.5% (27) cases were transported by public institutions operated ambulances (e.g., public hospitals, fire service department) and 67.5% (56) by private institutions operated ambulances (e.g., private hospitals, private companies). 98.8% (82 out of 83) of the used ambulances were equipped with oxygen, but only in 8.4% (7) ambulance transports had the availability of additional medical equipment (e.g., basic wound dressing consumables, common drugs). The existed facilities were observed in use by patients only in 7.3% (6 out of 82) cases. None of the ambulances was equipped with specially trained medical staff. Ambulances were mainly used for patients with CVDs (e.g., heart attacks, strokes) or RTIs victims; Figure 4).
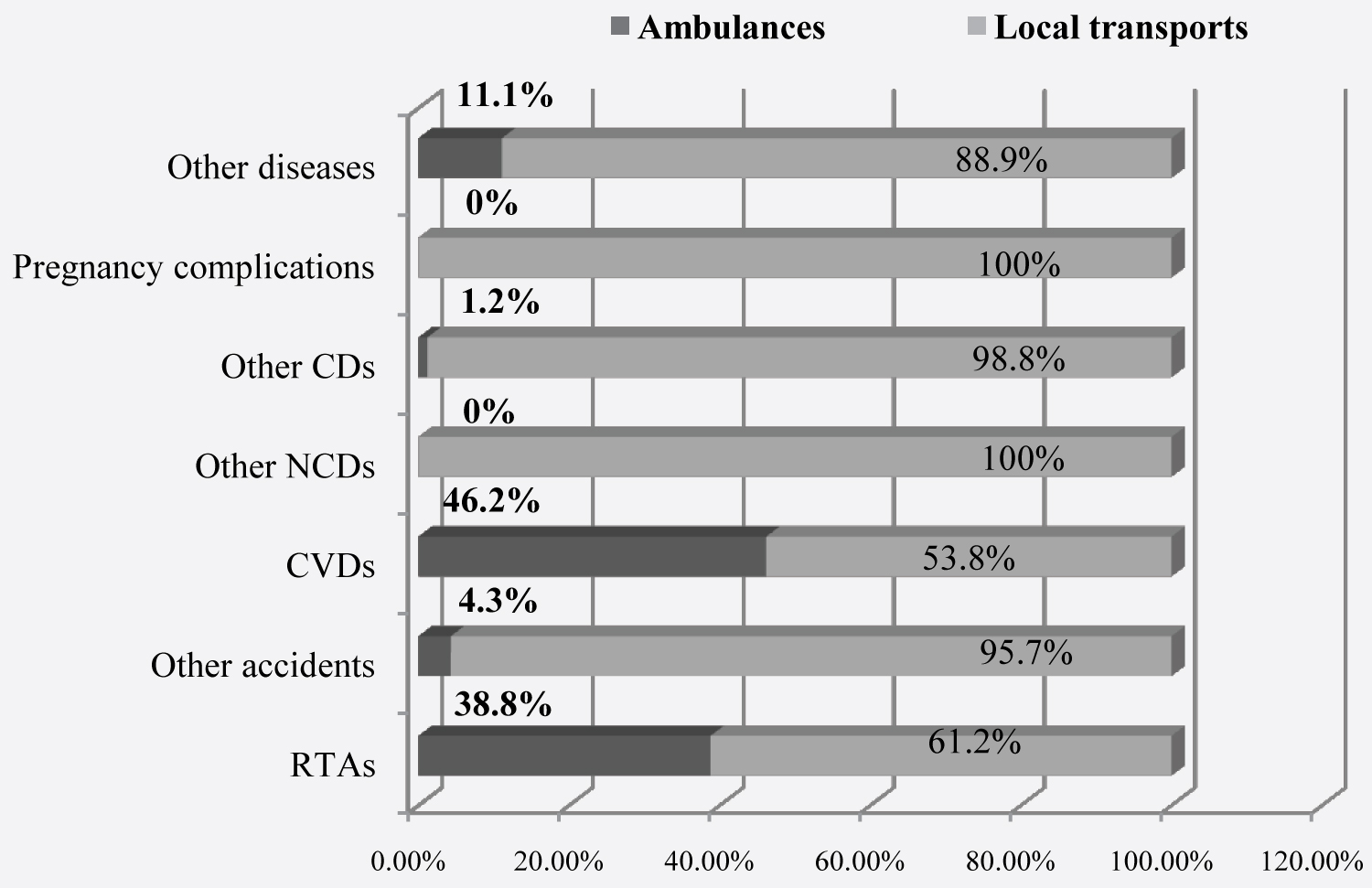 Figure 4: Transport used according to different medical emergencies in 4 study hospitals (N = 734).
View Figure 4
Figure 4: Transport used according to different medical emergencies in 4 study hospitals (N = 734).
View Figure 4
Major reasons for not using ambulances by 651 emergency patients were: Unavailability (534, 82.0%), unawareness of the services (152, 23.4%), high fare (94, 14.4%), hospital staff was not cooperative or demanded extra money (17, 2.6%), use of own vehicle (78, 12.0%; multiple responses). When asking the relatives of 52 emergency patients in 4 hospitals why they did not use ambulances, 78.9% of them reported that they did not wait for ambulances and 67.3% that they were unavailable or 51.9% that they did not know where to call for ambulances (Table 4; multiple responses).
Table 4: Reasons for non-use of ambulances by emergency patients' relatives. View Table 4
Transportation costs to hospitals: According to the interviews with relatives of 52 (out of 56) emergency patients who had used local transport, only 4 (7.7%) did not spend any money because one used a private car and three patients were brought by the people who had witnessed the emergency. For the others, the median cost for using local transport (rickshaws, motor-rickshaws, bus, taxi) was 2.1 Euro (range of 0.2 to 83.7 Euro, 1 Euro = 96.8 BDT). 19 patients out of 52 had used-according the relatives interviews- an ambulance but most of them (84.2%) for referral from one hospital to another. The median payment for ambulance services was reported to be approximately 31 Euro (range of 3.4 to 134.3 Euro).
Delay times as observed/measured in 4 hospitals for its ambulance services: We observed and measured in the 4 hospitals during 4 weeks the delay times of 17 rescue operations of the hospital ambulances. On average the transport by ambulance (from incoming call to arriving back at hospital) took 85 minutes (median) with a range of 22 to 150 minutes (Figure 5). During day time the median delay was 102 minutes, while at night the median delay was only 45 minutes. In terms of travel conditions, to cross 1 kilometer (k.m.) it took on average 5.3 minutes (during the day-time 6 minutes and during the night-time 3.6 minutes). On average it took 157 minutes (median) from starting the emergency call to hospitalization with a range of 75 to 990 minutes. The median delay was 171 minutes during day-time and 110 minutes during night-time. The observed reasons for substantially long ambulance transport times were mainly related to situational and structural limitations, such as congested traffic situations (Photo 2), weak traffic laws and management including public awareness regarding giving right to way to an ambulance (Photo 2), weak organizational structure, management and monitoring system.
 Photo 2: Ambulance with emergency patient was in traffic jam and was struggling in having right to way (source: was taken during field work).
View Photo 2
Photo 2: Ambulance with emergency patient was in traffic jam and was struggling in having right to way (source: was taken during field work).
View Photo 2
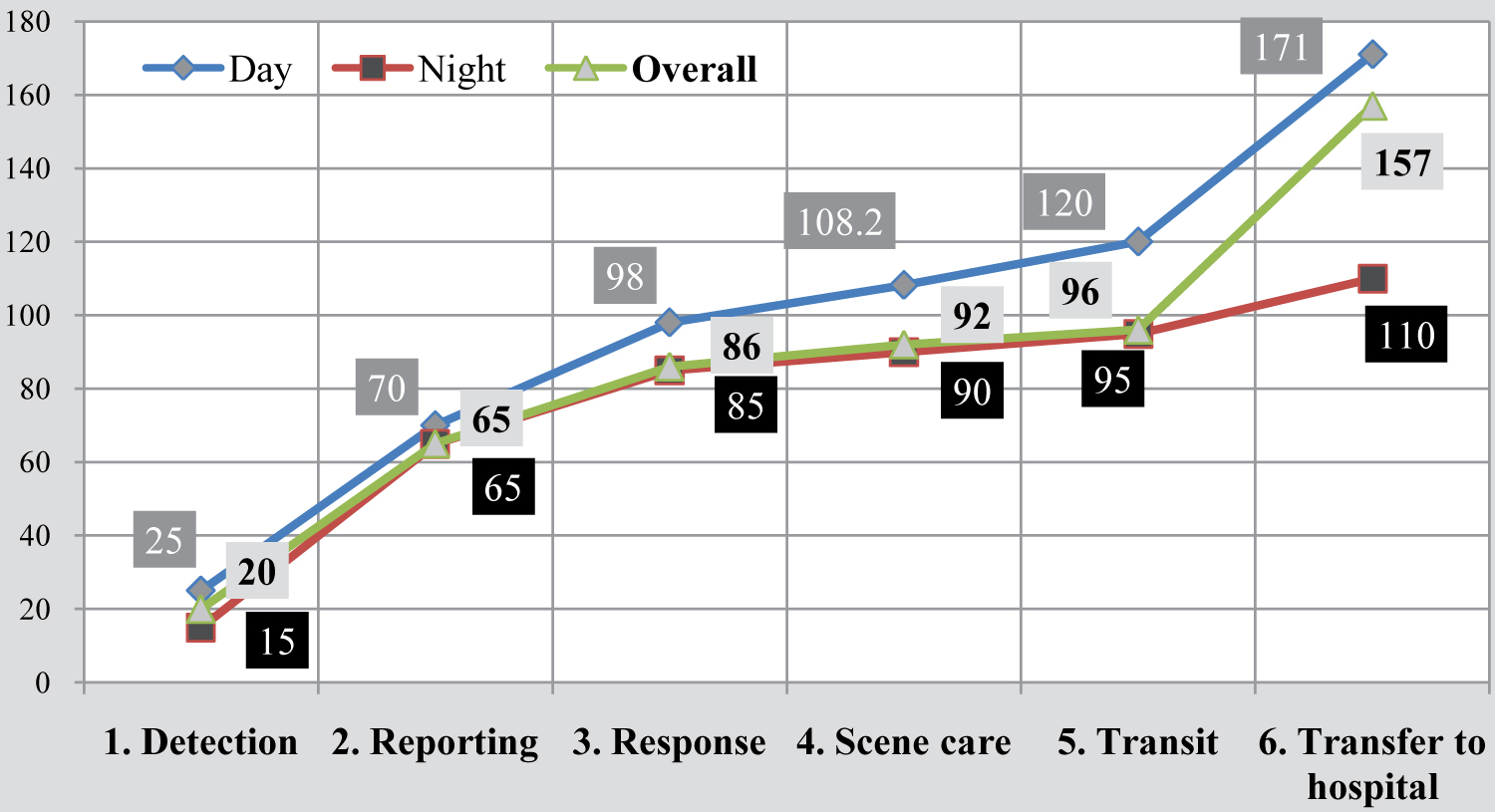 Figure 5: Median delay of rescue operations with ambulances in minutes (different steps from the recognition of emergency to hospitalization; N = 17 rescue cases).
View Figure 5
Figure 5: Median delay of rescue operations with ambulances in minutes (different steps from the recognition of emergency to hospitalization; N = 17 rescue cases).
View Figure 5
Delay of emergency patients using private transport: According to the interviews of emergency patients' relatives, 44.4% (326) of the 734 emergency patients arrived at the four hospitals between 30 to 60 minutes after start of the medical emergencies and the others (408, 55.6%) needed more than 60 minutes or even more than 1440 minutes (Figure 6). The total median delay to arrive at hospitals after the start of the emergency for ambulance users was 360 minutes (45 minutes to 2880 minutes) and for local transports users was 120 minutes (40 minutes to > 2880 minutes). For both ambulance and local transports users the total median delay was 120 minutes (40 minutes to 2880 minutes). The long delays were belonging mostly to situations when victims wait or relatives could not decide to go or not to go to hospital. The median transport duration (from finding transports to arrive at hospitals) for ambulance users was 60 minutes (20 to 480 minutes) and for local transport users was 40 minutes (10 to 800 minutes), and for both users was 40 minutes (10 to 800 minutes). Interestingly, out of the 325 critically ill patients, 67.1% (218) came to the hospitals with a delay of over 60 minutes.
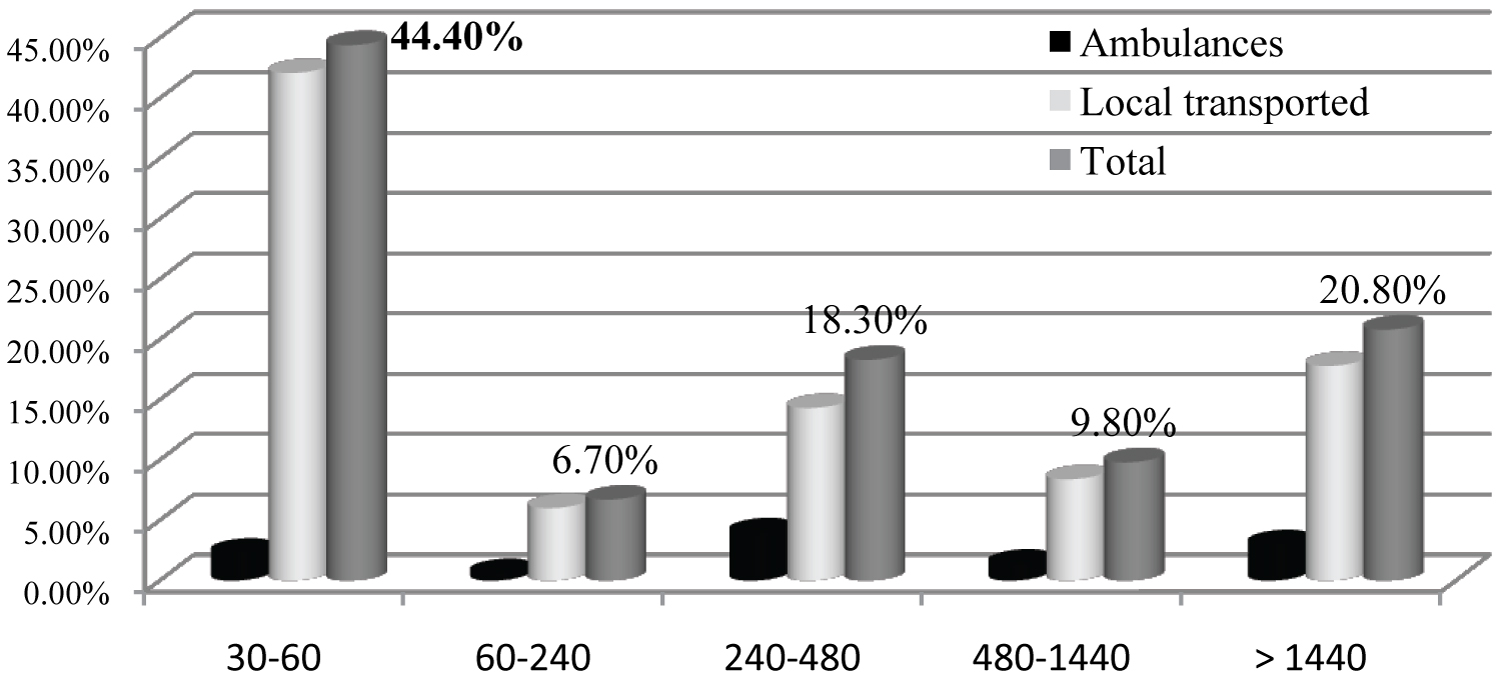 Figure 6: Delay times in minutes from start of the problem to arriving at the hospital by emergency patients (N = 734).
View Figure 6
Figure 6: Delay times in minutes from start of the problem to arriving at the hospital by emergency patients (N = 734).
View Figure 6
Major reasons for delayed arrivals at hospitals' emergency department were: 56.9% of the total emergency patients had to discuss first with relatives or friends what to do (Table 5); 45.8% experienced traffic jams (see Photo 2); 36.6% had difficulties in arranging a transport and 33.4% went first to a nearby dispensary before coming to the hospital (multiple responses).
Table 5: Main reasons for transport delay by different types of emergency patients in 4 study hospitals. View Table 5
Relatives of emergency patients (N = 56) rated their satisfaction with the existing EMRS with only 1.8 on a scale from 0 (= poor) to 4 (= very good). Reasons for their lack of satisfaction were: 82.1% (46) of the relatives of emergency patients stated lack of ambulances with equipment for emergency care, 75.0% (42) mentioned traffic-jams and that the public or police did not guide ambulances through the crowd, 28.6% (16) mentioned corruption, 23.2% (13) mentioned lack of awareness of EMRS, and 57.1% (32) reported about other situational and structural issues (N = 56; multiple responses).
Patients' relatives recommended to ensure availability and to improve the quality of ambulance services (87.5%, 49 out of 56 interviews), to go for governmental initiatives and investment in EMRS (45, 80.4%) and to monitor progress (32, 57.1%). Other suggestions were: To establish a coordination centre with a standardized phone number (16, 28.6%), upgrade the current ambulances (12, 21.4%), formulate policies (11, 19.6%) and promote awareness raising programs (4, 7.1%; N = 56; multiple responses).
Most of the 23 EMRS service providers and managers lamented the non-existence of pre-clinical emergency care in Dhaka city. There was no early response system, no care at scene or during transport and that emergency patients come usually to the hospital by themselves.
Only one service provider (1 out of 23) reported that the EMRS in Dhaka city was partially managed and operated effectively. The others 22 service providers and mangers held the view that none of the investigated aspects of local EMRS (quality, need, saving lives and disabilities, economic aspects, awareness) was working well although they argued that there was a high need of this service to save lives and avoid disabilities.
The service providers and managers (N = 23; multiple responses) major complained about EMRS in Dhaka to be ineffective were: Traffic-jams (22, 95.7%); corruption and syndicate business (18, 78.3%); unfixed fare (17, 73.9%); no universal coordination centre with a standardized phone number (17, 73.9%); lack of ambulances with equipment for emergency care and skilled staff (16, 69.6%); deficit of policy including weak traffic laws and management system (15, 65.2%); peoples lack of awareness of EMRS (10, 43.5%); lack of financial and political initiatives (9; 39.1%); and other reasons (4, 17.4%).
The service providers and managers recommendations to improve the local EMRS were: Organize capacity development (22, 95.7%); re-equip the ambulances (19, 82.6%); assure quality (ambulances with paramedics and equipment for basic emergency care), affordability (reasonable fixed fare) and availability of ambulances (17, 73.9%); formulate policies and guidelines for dealing with ambulances on the street and in traffic jams (police to give preference to ambulances; general public to make space for ambulances in traffic jams; 16, 69.6%); offer awareness raising programs for the police and the public (15, 65.2%); monitor progress (12, 52.2%); establish universal coordination centre with a standardized phone number (11, 47.8%); push for governmental initiatives and investment in EMRS (10, 43.5%); strengthen multi-sectoral coordination and management system (9, 39.1%); and promote health insurance which covers the costs of pre-hospital emergency care (7, 30.4%).
The study aimed at contributing to improve the existing EMRS in Dhaka city, Bangladesh through a situational analysis and needs assessment of EMRS.
Our document analysis of 2 major hospitals in Dhaka city showed that 45.9% of the deaths in 2014 were due to CVDs, RTIs, other accidents or injuries, and suicidal attempts. This is similar to the findings in other parts of Bangladesh [15,18,28,29]. These analyses showed also that the number of deaths from medical emergencies increased over the last decades in the country. Particularly the increase of CVDs in urban Bangladesh has reached alarming levels [15,18,28,30]. Also deaths due to disasters such as building collapse, fire, gas explosion, occupational accidents are increasingly important [12,14,17,31]. Likewise CDs (particularly acute diarrhoea, pneumonia, dengue fever in children), the leading causes of morbidity in Dhaka city [13,14], would often be fatal if emergency services cannot be ensured.
The scarcity of ambulances was found to be highly associated with an increased number of deaths due to medical emergencies in other South-Asian countries such as India and Pakistan [7,8]. Therefore WHO identified emergency medical care at scene as one of the core initiatives for preventing mortality and disability but also for reducing the treatment costs [2,4,6,11,32,33].
We quantified in our study the deficient transport of emergency patients in Dhaka city. We found that particularly rickshaws or motor-rickshaws were used for patient transport which is slow and uncomfortable for the patients. Studies in India and Pakistan also showed that over 70% of patients arrived at hospital by local transport and that many of these emergency patients die before reaching clinical care [7,8].
The concerns of relatives of emergency patients and of service providers and managers were related to three groups of limitations of the current EMRS in Dhaka city:
1) Deficit of policy and inter-sectoral collaboration:
• Deficit of policy and guidelines for the operation of ambulances [7,9,34-36]
• Weak traffic laws and management regarding giving right to way to an ambulance
• Absence of a common fare policy including health insurance practice
• Lack of inter-sectoral collaboration and initiatives
2) Poor Structure of the Current EMRS System:
• The absence of a universal coordination centre with standardized phone numbers in Bangladesh (which was also documented in other studies) [7,36-39].
• The low availability of ambulances due to the limited number (2.8 ambulances per 100,000 population), the misuse of ambulances and the low proportion of functional ambulances out of the existing ones (which was also reported form other cities in Bangladesh) [13,36,37,39-41]
• Poor ambulance equipment and lack of skilled staff for emergency care (ambulances were used like taxis as there was only the un-trained driver and no skilled staff) [38,39]
• Absence of emergency physicians and trained rescue teams for pre-clinical care (studies in other countries - Germany, Switzerland, Japan, South Korea, and Trinidad and Tobago - showed that an ambulance equipped with skilled paramedics, essential medical devices and drugs as well as the short response time of 15 minutes was found to be crucial for the patient`s survival and positive clinical outcome [4,19,20,42,43].
3) Lack of Awareness in the Population on EMRS
• Absence of basic EMRS education in academic curricula and in professional training particularly for police and public transport drivers
• Lack of training of lay people including school children and students to detect medical emergencies and to offer first aid
• Lack of awareness in the general public about ambulance services including where to call and transport costs (The median payment for ambulance use in our study was -according to the relatives of emergency patients- 31 Euros, which was much higher than the actual fare (3.4-10.3 Euros) [41].
The median delay times of ambulances from the call to getting the patient to hospital was 85 minutes (during the day 102 minutes and at night 45 minutes). The transportation delays were longer for ambulance users (60 minutes) than for local transport users (40 minutes). The total delay (time from the count to arriving at hospital) was unacceptably long: Median delays 360 minutes for ambulance users and 120 minutes for public transport users. This is similar to findings in other studies in Bangladesh [44-46] and in India 80% of the emergency patients arrived at hospitals with a delay of over one hour [47]. This is well above the rule that emergency patients should be treated at scene within 15 minutes [4,19,20,42,48].
A step-by-step approach is recommended based on the above described identified three groups of limitations of the current EMRS in Dhaka (Figure 7). Possible steps could be:
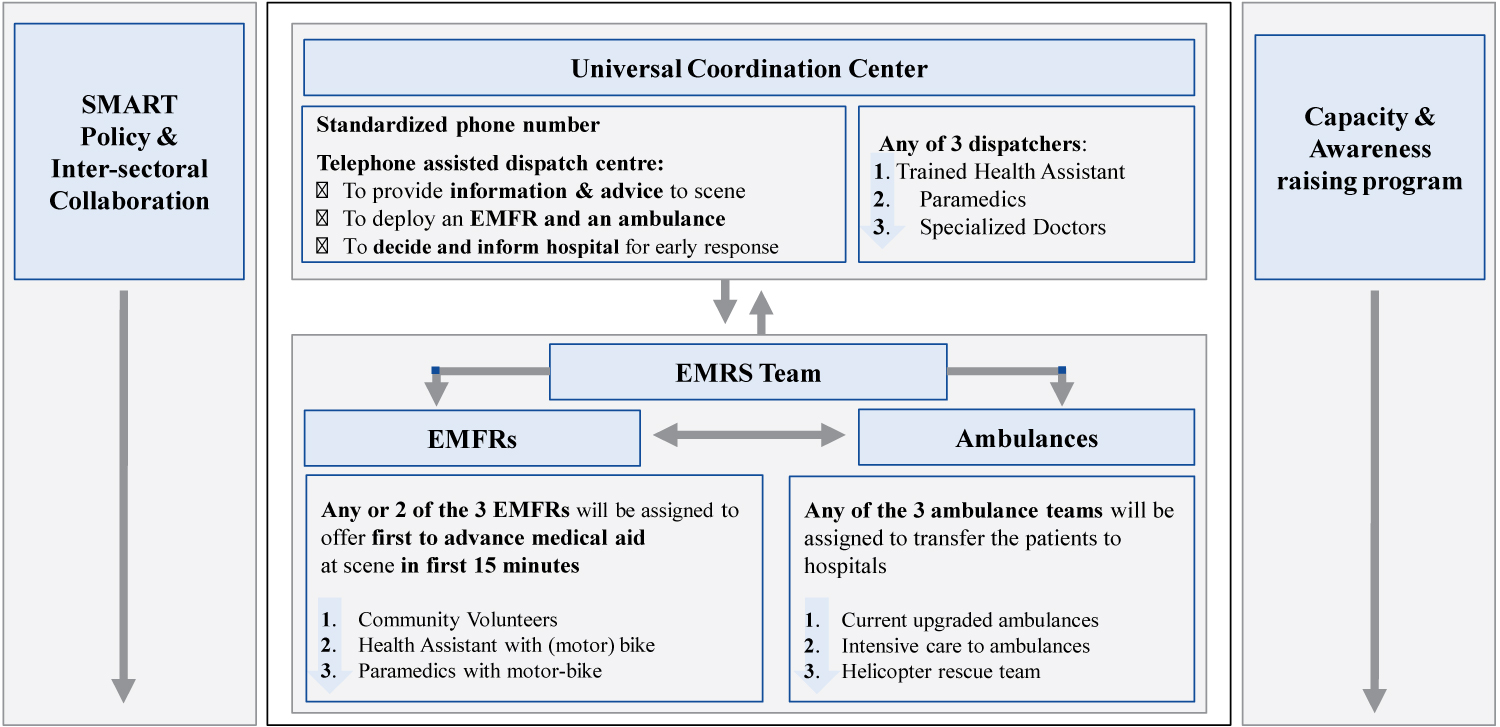 Figure 7: Proposed model to improve the emergency medical rescue services in Dhaka city, Bangladesh.
View Figure 7
Figure 7: Proposed model to improve the emergency medical rescue services in Dhaka city, Bangladesh.
View Figure 7
First step: Strengthen inter-sectoral collaboration and formulate policy: Inter-sectoral collaboration is needed to formulate a Specific, Measurable, Achievable, Result-orient, Time-bound (SMART) policy for EMRS operations and management. In the SMART policy, a sector wide long-term (e.g., 10 years or more) target should be set and emphasis should be given to transparency and accountability. A common fare policy for ambulances also should be included in the policy.
Second step: Upgrade and improve the system: A standardized telephone assisted call centre should be installed to provide information and advice to scene and to deploy an emergency medical first responders (EMFRs) and an ambulance [2,19,21,49]. EMFRs (ranging from community volunteers to paramedics) should be formed to offer first aid at scene before arriving of the ambulance [2,49-53]. The ambulances should be equipped with basic medical facilities [2,7,9,19,21,54]. By adding Intensive Care Units (ICU) to ambulances with skilled paramedics following standard operational procedures would make an important difference.
The response times of ambulances could be improved through (a) The increase number of ambulances [55,56], (b) The decentralization and reallocation of ambulances throughout the city (for this purpose the use of police and fire service stations might be helpful [56-62], and (c) The developing of an emergency lane for emergency vehicles.
Third step: Increase capacity and awareness of the public: Capacity building of EMRS staff is required on a regular basis [7-9,11,19-21,49,52]. To increase the general awareness of EMRS, information on recognition of medical emergencies, and first aid should be disseminated by mass media [8,11,49,62]. It should be compulsory for all levels of schools and university education as well as for professional training (e.g., fire fighters, police, public transports drivers, local pharmacists and other first responders at scene) [2,7-10,20,29,49,52,54,62-66]. Additional awareness raising programs in the population would focus at recognizing medical emergencies, ability to provide by standing first aid, to call the emergency call centre, and to prioritize and give right way to ambulances [8,20,49,62].
The present study had limitations. Other hospitals and rescue service providers and managers could not be included. Due to shortage of sufficient medical records (studied hospitals did not want to open), the results related to sudden deaths and disabilities are not representative for the whole city.
Long delay times and low use and utilization of the limited, unsystematic and unorganized ambulance services in Dhaka city were contributing to a number of deaths and disabilities of emergency patients. Dhaka city needs to upgrade and improve its EMRS system through a step-by-step process of telephone assisted emergency first responders led pre-clinical care.
We are very grateful to all the hospitals and organizations in Bangladesh who accepted and supported this project and to all the relatives of emergency patients for taking the time to answer our questions. Special thanks go to Dr. Shah Alom Siddique (NIPSOM, Bangladesh) and Dr. Md. Mosharof Hossain (Ad-din Medical College Hospital) for their kind field supports. The study would not have been feasible without a grant and support provided by the Björn Steiger Stiftung in Germany. Our final gratitude goes to Dr. Sonia Diaz Monsalve (Centre for Medicine and Society, Freiburg University, Germany) for her constant motivation and valuable advice when carrying out the study.
The authors declare that they do not have any conflict of interest.
This study was supported by the Bjorn Steiger Stiftung, Germany.
All authors were involved in designing, writing and editing of the manuscript, with MMH leading this effort. MMH and KP performed the data collection, processing and analysis of the data and the literature review. MMH and AK did the data evaluation and drafted the first version of the manuscript. All authors reviewed and approved the final manuscript.