Juvenile Nasopharyngeal carcinoma (NPC) is a rare head and neck cancer in Western Countries. Neck radiotherapy (RT) is a routine procedure for treating or preventing the nodal metastasis in NPC patients. Ionizing radiation from RT has been associated with enhanced atherosclerotic process of large vessel arteries of the neck and brain which results in higher incidence of cerebrovascular events.
Herein we describe a 43-year-old man who presented with acute hemiparesis due to partial infarct in the anterior circulation of the brain due to severe steno-occlusive atherosclerosis of the neck arteries decades after RT for NPC. Additional risk factors were high levels of Low-Density Lipoprotein (LDL) and low Arterial Pressure (AP) possibly associated to post-RT secondary hypothyroidism and reduced corticotropin.
Iatrogenic or acquired endocrinopathies may represent additional triggers of the atherogenic process and should be kept into account when dealing with rare forms of juvenile strokes in patients who had undergone to RT for either brain or neck cancers decades before.
Nasopharyngeal carcinoma, Radiotherapy, Carotid atherosclerosis, Stroke, Hypothyroidism, Adrenal insufficiency, Hipopituitarism
Juvenile Nasopharyngeal carcinoma (NPC) is a rare head and neck cancer in Western Countries. Since NPC is highly sensitive to radiation, and cervical lymph node metastasis are common in NPC patients (60-90%), neck radiotherapy (RT) is a routine procedure for treating or preventing the nodal metastasis in NPC patients. Ionizing radiation from RT has been associated with enhanced atherosclerotic process of large vessel arteries of the neck and brain which result in higher incidence of cerebrovascular events [1-3].
Although a latency of decades may separate RT from symptomatic events such as strokes, a number of additional risk factors associated either to acquired pathologies or to the personal genetic profile may further accelerate and extent the atherosclerotic cascade [4]. Interestingly, age of 44.5 years, RT post-duration of 13.5 years and the presence of ≥ 2 additional risk factors were found to be positively associated with an increased risk to found severe atherosclerosis at screening (more than 50% of screened patients) [4].
A 43-year-old man was admitted at the ED department as more than 24 hours earlier had complained blurred vision in the right eye and reduced strength in the limbs of his left hemisome (hemiparesis). NIH-Stroke scale (NIHSS) on admission was 4. He was immediately subjected to head CT which showed the presence of a focal hypodense area at the level of the right putamen, compatible with a subacute infarct lesion (Figure 1). The Angio-CT study documented lack of opacification of the right common carotid artery (CCA) approximately 10 mm from his origin and of ispilateral external (ECA) and internal carotid artery (ICA) throughout their all course. A lack of opacification of the M1 and M2 sections of the right Medial Cerebral Artery (MCA) was also evident. The caliber and opacification of the remaining arterial vessels of the Willis' polygon were regular. An atheromatous plaque, partly calcified, determined hemodynamically significant (stenosis > 70-80%) near the origin of the left Internal Carotid Artery (ICA) (Figure 2).
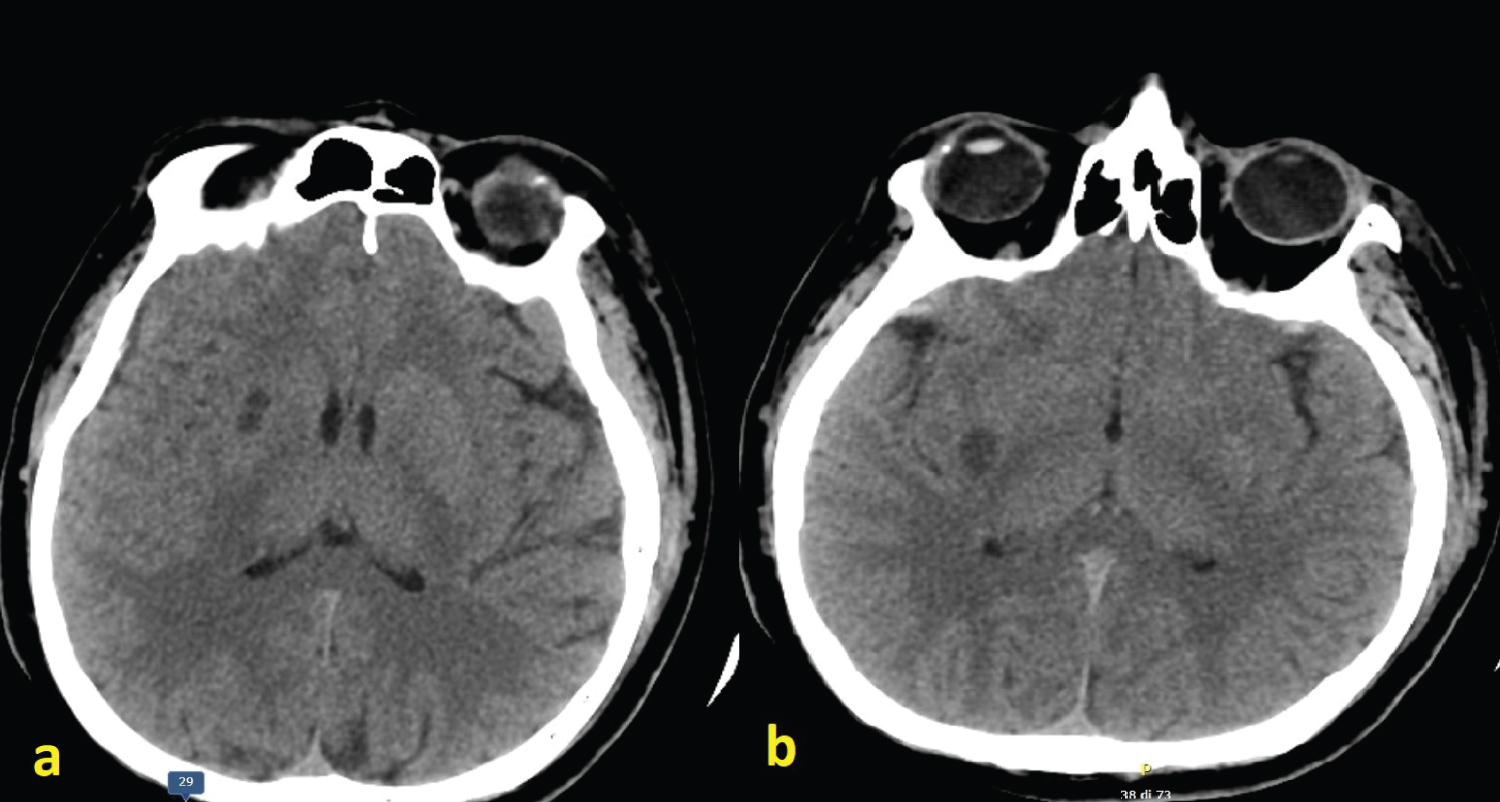 Figure 1: CT brain scan showing hypodense lesions within the right putamen and peri-insular regions due to ischemic infarcts in the territory of lenticulo-striate arteries emerging from the Middle Cerebral Artery (MCA) (a,b).
View Figure 1
Figure 1: CT brain scan showing hypodense lesions within the right putamen and peri-insular regions due to ischemic infarcts in the territory of lenticulo-striate arteries emerging from the Middle Cerebral Artery (MCA) (a,b).
View Figure 1
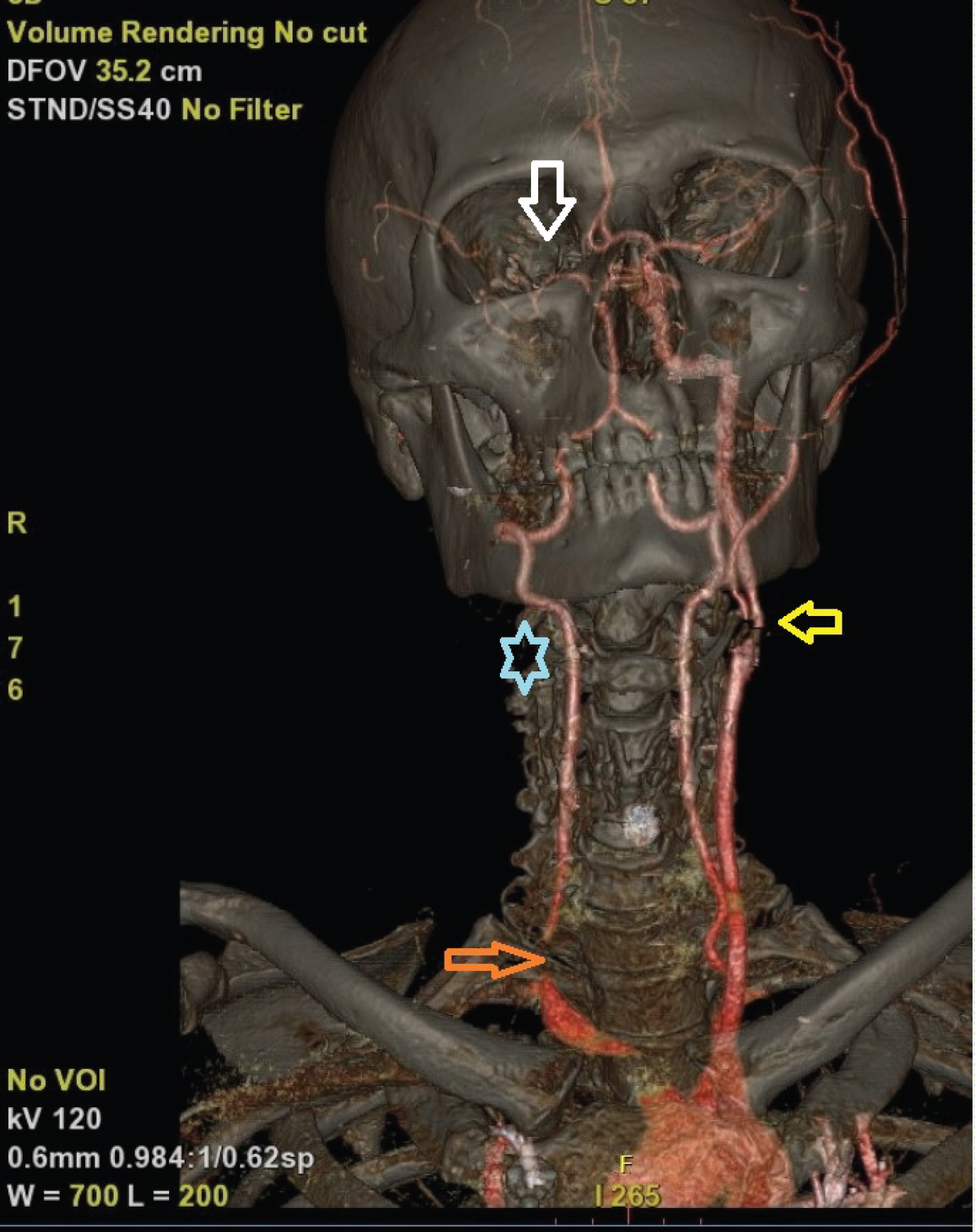 Figure 2: Esocranic and intracranic angio-CT: Light blue star showing the lack of the signal of the right Common Carotid Artery (CCA) with either ispilateral Internal Carotid Artery (ICA) and External Carotid Artery (ECA). Orange arrow: Proximal occlusion of the right CCA. Yellow arrow: Severe stenosis at the origin of the left ICA. White arrow: Absence of the signal associated with lack of flow within M1 and M2 tract of right MCA.
View Figure 2
Figure 2: Esocranic and intracranic angio-CT: Light blue star showing the lack of the signal of the right Common Carotid Artery (CCA) with either ispilateral Internal Carotid Artery (ICA) and External Carotid Artery (ECA). Orange arrow: Proximal occlusion of the right CCA. Yellow arrow: Severe stenosis at the origin of the left ICA. White arrow: Absence of the signal associated with lack of flow within M1 and M2 tract of right MCA.
View Figure 2
Due to the long time spent from the onset of acute symptomatology (more than 24 hours), the patient was declared ineligible to any recanalizing procedures (either pharmacologic or intravascular clot aspiration) and double anti-aggregating therapy was prescribed including 100 mg acetylsalicic acid and 75 mg clopidogrel in an attempt to start a secondary prevention. High dosage statin therapy was similarly added according to international stroke guidelines. Routine blood exams revealed high Low Density Colesterol (LDL) = 154 mg/dl while all other parameters were within normal ranges. Additional risk factors for juvenile stroke were investigated and found within normal ranges. They included either rheumatologic panel, risk factors for thrombophilia and genetics for both factor II and factor V. Interestingly, clinical monitoring revealed very low Arterial Pressure (AP max = 90-100 mmHg) which was unresponsive to noradrenaline triggering. Emphasizing the ginoid obesity of the patient and the scarce development of his body hair as well as of melanin on his skin, we wondered whether he could hide endocrinopathy. Blood ACTH was found reduced with respect to normal levels (4,6 pg/ml; n.v.: 9-52), as well as f-T3 (0.86 pg/ml; v.n. 2.20-4.2), and f-T4 (0.45; v.n. 0.8-1.7). Blood and urinary cortisol, as well as TSH were within normal range.
The patient's AP promptly responded to Idrocortisone 500 mg/die in continuous intravenous administration returning within acceptable ranges (AP max ~ 150 mmHg), thus moving away the risk to induce an hypoperfusive stroke or to disable collateral luxury circulation. The patients' conditions continued to ameliorate during hospitalization and, on day 6 after admission, the patient himself decided to voluntary dismiss.
RT of either the neck and the brain for nasopharyngeal carcinoma or brain tumor may induce delayed radiation-induced cerebral atherosclerosis in middle aged patients, early with respect to their expected survivor curves [4-7]. Predictors and accelerators of such process include classic cardiovascular risk factors as well as age of radiation, radiation dose and post-RT duration [4]. Hypothyroidism and pituitary disfunction are frequent consequences after radiation for anterior skull base malignancies with involvement of up the 71% irradiated patients [8,9]. These endocrinopathies play a relevant role in inducing or aggravating dysmetabolism associated to blood cholesterol homeostasis, glucose intolerance or diabetes, or regulation of AP, relevant risk factors for atherosclerosis and stroke. Indeed, our patient had increased levels of blood LDL, possibly due or aggravated by his post-RT hypotiroidism, which may have completed the pathogenic cascade leading to bilateral steno-occlusive pathology of large artery vessels of the neck.
Although the pathogenic mechanism leading to stroke in our patient was acute occlusion of the right ICA and artery-to-artery embolism up to the M1 - M2 tract of the ipsilateral MCA, we believe that cerebral hypoperfusion due to low AP associated either to iatrogenic hypothyroidism or reduced corticotropin and adrenal insufficiency may be an additional risk factor in enlarging at least the local penumbra through interrupting the surrounding luxury circulation in such patients. Indeed, our patient ameliorated from NIHSS = 4 up to NIHSS = 1 upon PA stabilization and without having performed any reperfusive treatment.
Hemodynamic mechanism may also play a role in triggering stroke in the border territories between different arteries belonging to the Willis' polygon (stroke by misery perfusion).
Due to the high risk to develop an early and severe atherosclerosis in patient who underwent to RT for cancer of the neck or brain, we believe that deep and frequent screening for secondary endocrinopathies should be performed in all these patients as various dysmetabolisms may represent either an additional risk factor for steno-occlusive pathology of arteries and a triggering mechanism for the occurrence of stroke.
None.
The patient is not recognizable.
None.
There is no conflict of interest to disclose.
Giorelli M conceived the work, wrote the article, directed the group. Leone M, Altomare S, Aniello MS, Liuzzi D, Plasmati I, Sardaro M, and Superbo M helped to perform the clinical assessment of the patient and managed execution of the therapy. Tatò D performed laboratory assessments and discussed involvement of endocrinopathies. Carpentiere R performed CT and angio TC neck and brain scans and discussed radiologic findings with Guglielmi G and Giorelli M.