Occlusion or rupture of cerebral blood vessel can cause a stroke. It can occur either on a child and adult even it unusual in children. Stroke in pediatric population is rare but it carries often long-term disability and mortality. We present two cases of pediatric stroke with metabolic disease as underlying disease. One of them admitted with weakness and clumsiness persisted of right hand and leg. The other one admitted with weakness in the left hand and leg. Both showed motor improvement and progression cerebral blood flow after IAH procedure. The rarity of the case and successful management prompted us for reporting along with review of literatures.
Chronic stroke, Pediatric, Digital subtraction angiography, Intra-arterial heparin flushing, Interventional Radiology
The definition of Stroke based on WHO (World Health Organization) is clinical syndrome of rapidly developing focal or global disturbance of brain function lasting > 24 hours or leading to death with no obvious nonvascular cause [1] but stroke in children is varied and different from those seen in adults [2]. It can increase the consequences of the brain injury [3]. Pediatric stroke defined as stroke occurring in children aged 29 days after birth to 18 years [4-6] and it can be classified by stroke type and the number of vessels involved, and territory involved [4].
Incidence of pediatric stroke increased every year even it still becoming serious problem in the health sector. It can cause mortality and disability in children, although not as prevalent as in adults. The annual incidence of childhood stroke ranges from 2.3 to 13 per 100.000 children per year in developed countries [4] and up to 36% of them involved vertebrobasilar territory [7].
The aim of clinical and imaging triage is to differentiate ischemic, hemorrhagic and non-vascular etiologies, triggering different management cascades. Etiology of pediatric stroke is multifactorial and many risk factor such as cardiac disease, prothrombotic disorder, viral infection, arteriovenous malformation (AVM) or another vascular disease, syndrome metabolic disorder, vasculitis, cancer, and head and neck trauma [8] but there are no clearly guidelines for pediatric stroke [9]. Pathogenesis of both ischemic and hemorrhagic stroke was considerably in children compared to adults [10].
Diagnosis of stoke in children can be difficult because there are many other diseases that may mimic a stroke in children and resolve within 24 hours [8,11]. Neuroimaging is essential for the diagnosis of pediatric stroke and to differentiate stroke form stroke mimics. Magnetic resonance imaging (MRI) can identify the site of vascular stenosis or occlusion, presence of vascular malformations and also arterial dissection, offering a greater chance of determining etiology, selection of the most appropriate treatment interventions [12]. Magnetic resonance angiography (MRA) and magnetic resonance venography (MRV) also performed, especially when venous thrombosis is suspected [13].
Ischemic stroke is most caused by a thrombotic or embolic event. Anticoagulant is recommended for patient with arterial dissection or venous sinus thrombosis [11]. In this case, the anticoagulant treatment was unfractionated heparin which was delivered directly to the thrombus site using a catheter as a guidance of digital subtraction angiography, it was already modified as IAHF. After IAHF procedure was performed, no expected complication happens such as hematoma, bleeding at puncture site, and neurological defect.
The following of case series describes an 11-years-old boy and 4-years-old girl with arterial stroke. Both show improvement after IAHF procedure.
An 11-years-old male child was admitted to the pediatric department with chief complain of weakness and clumsiness persisted of the right hand and leg, mild headache, and dysarthria for 6 weeks ago. Physical examination revealed that patient was conscious, all vital sign was normal, but body mass index (BMI) was 29.3 (weight 68 kg, height 154 cm). CDC curve showed that his BMI is over than 95th percentiles by his age - 11 years, and classified in obesity (Figure 1).
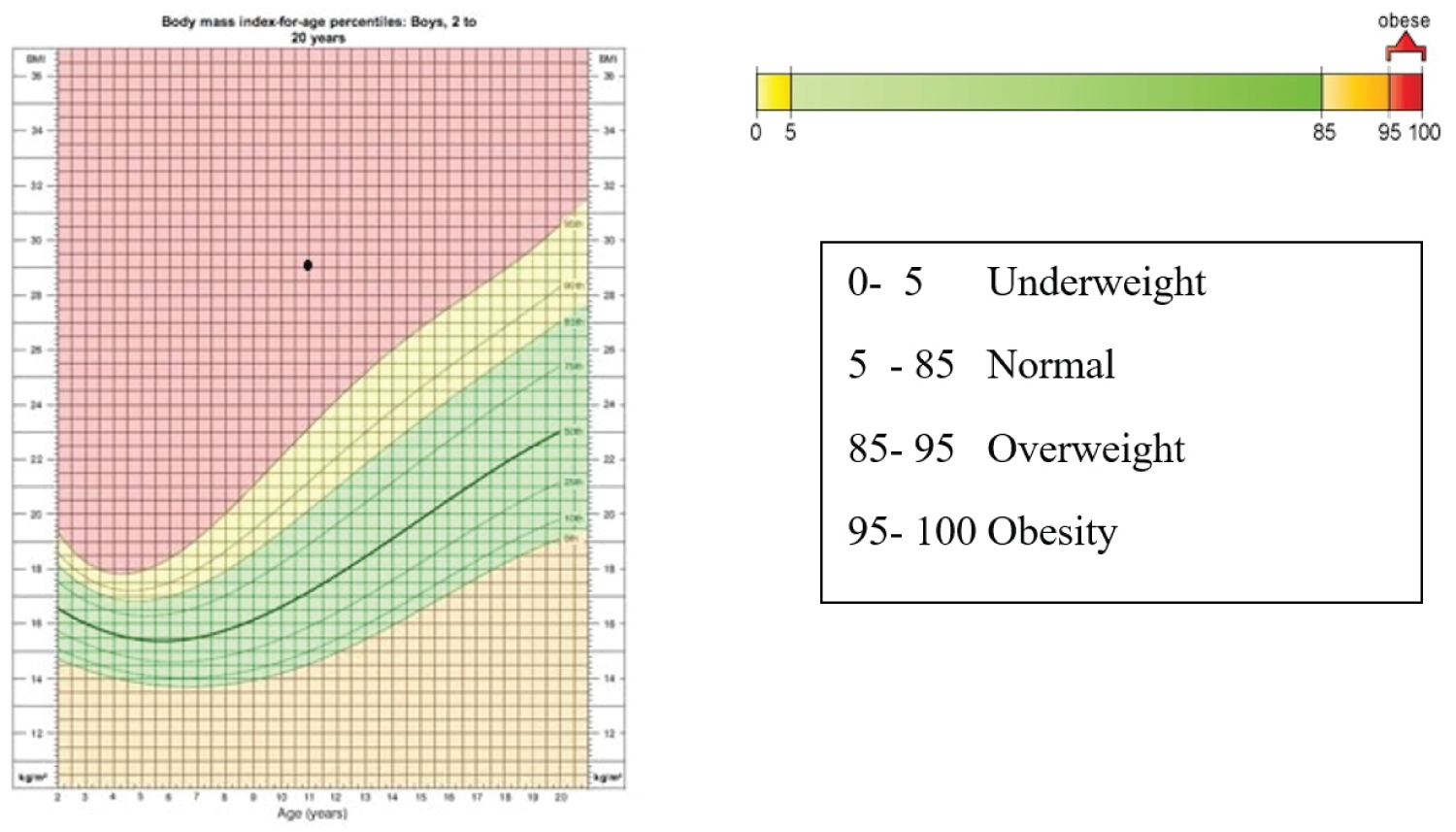 Figure 1: BMI curve by age for boys (CDC).
View Figure 1
Figure 1: BMI curve by age for boys (CDC).
View Figure 1
The neurologic examination revealed decreased grip strength of the right hand and slowing of rapid alternating movements with scale 4 of motor strength both right hand and leg. Brachialis reflex was positive. There was no report of trauma, fever, vomit, nausea or the other symptoms in the previous days and no pertinent past medical history. Growth and development history were convenient with milestone. In laboratory test revealed triglycerides was 414 mg/dL, high density lipoprotein was 41 mg/dL and low-density lipoprotein was 103 mg/dL, sugar level was normal, urea-creatinine serum was normal.
Whole brain MRI were found stenosis at left middle cerebral artery, left transverse sinus and left sigmoid sinus smaller than right transverse sinus and sigmoid sinus, and chronic infarct area are left parietal region.
These results were consulted to the interventional radiology department and IAHF procedure was performed. After IAHF, we found direct improvement in right side motor function, he can do rapid alternating movements even he still leaks of strength to grip. Result from IAHF procedure suggested an occlusion of left middle cerebral artery, collapse of left transverse and sigmoid sinus were release post flushing. No AVM, AV fistula, tumor even extravasation of contrast (Figure 2 and Figure 3).
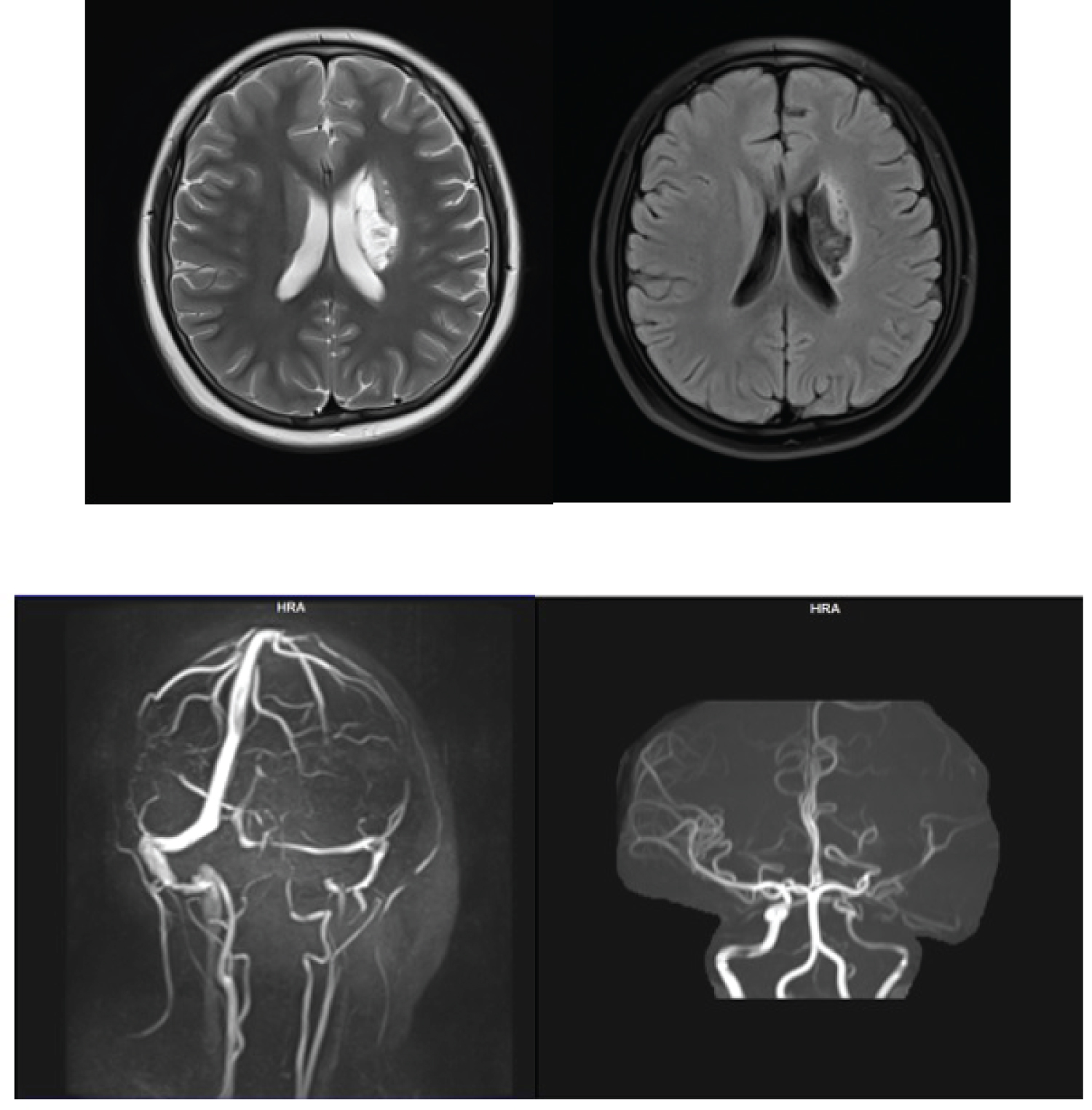 Figure 2: Brain MR Imaging pre IAHF.
View Figure 2
Figure 2: Brain MR Imaging pre IAHF.
View Figure 2
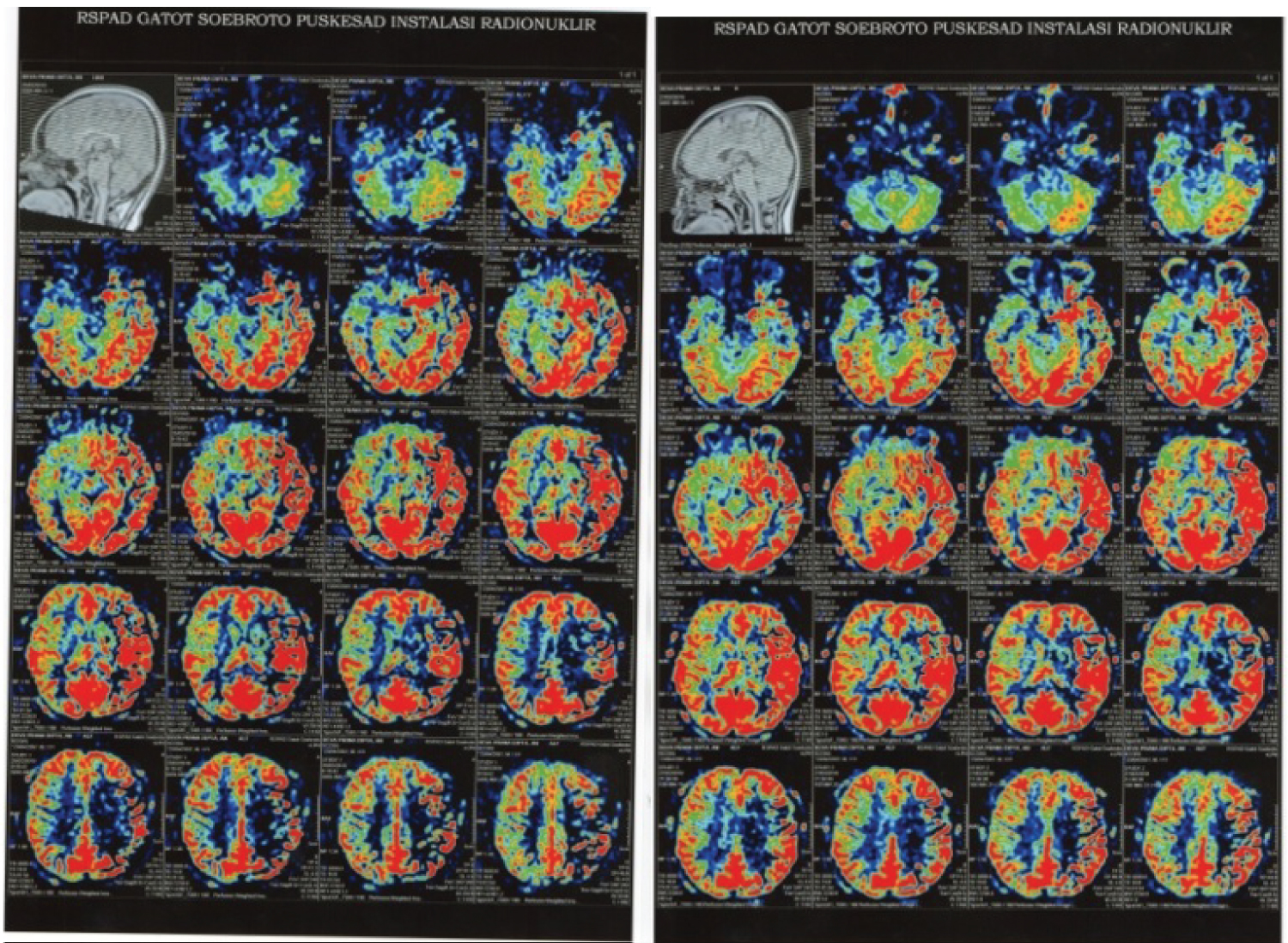 Figure 3: The perfusion image compared brain perfusion before (left) and after (right) IAHF. There is progression CBF after IAHF procedure.
View Figure 3
Figure 3: The perfusion image compared brain perfusion before (left) and after (right) IAHF. There is progression CBF after IAHF procedure.
View Figure 3
Patient was transferred to recovery room for monitoring after IAHF procedure for 2 hours and sent back to ward after fully conscious. He was then discharge from the ward the day after IAHF procedure.
Outcome: 4 hours after IAHF procedure, the child had no clinical or imaging sign of stroke recurrence, although the arterial occlusion persisted. Nearly 2 months after IAHF procedure, the weakness of the right hand and leg, headache and dysarthria improved.
A 5-year-old boy admitted to the Presidential Hospital Gatot Soebroto Army Central Hospital with left side weakness since a month ago. Weakness was noticed by the parents after the child fell off when cycling. After the accident, the child could not fully raise his left hand, nor could hands clasp his fingers hard enough to grasp objects with his left hand. He also had trouble writing because his left hand could not support his right hand when grasping the pen. He walked by use his tiptoe left leg and clawed fingers foot. First, the parents thought that his weakness was caused by an injury to his left hand and leg, but suspicion of another etiology came up when the weakness persisted even after a month from the minor accident.
On physical examination, we found the patient was conscious and verbal communication was within normal. Blood pressure was elevated for his age at 120/70 mmHg. The patient's systolic blood pressure was in the 99th percentile and diastolic blood pressure was higher than the 95th percentiles in comparison to patients that were 5-years-old in the general population. His body weight was 33 kg and height 120 cm with a BMI 22.9. CDC curve showed that his BMI was over than 99 percentiles by his age 5 years and 11 months, therefore he is classified as obese (Figure 4).
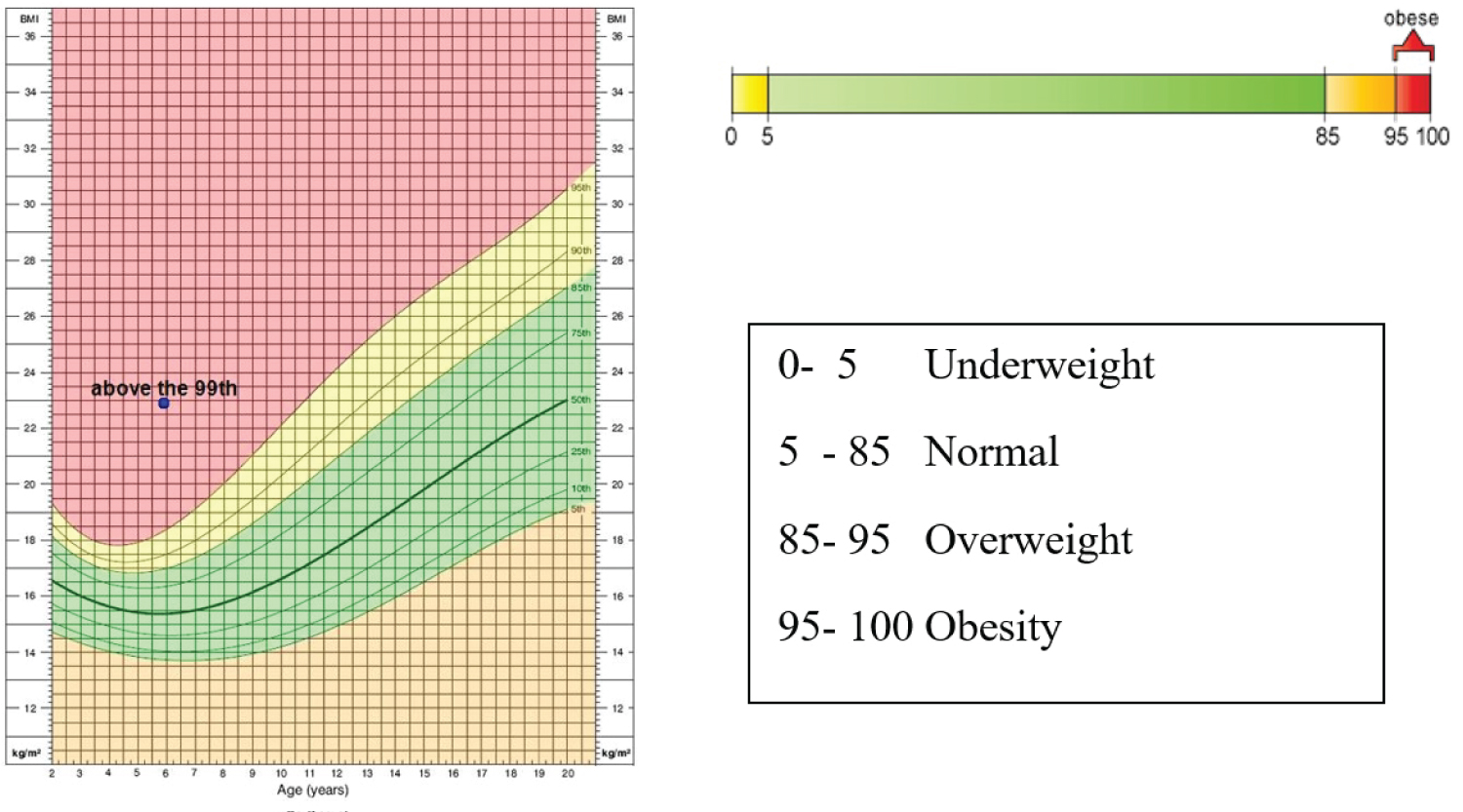 Figure 4: BMI curve by age for boys (CDC).
View Figure 4
Figure 4: BMI curve by age for boys (CDC).
View Figure 4
Eating habit in this child was bad. He liked to consume instant noodles, snacks, fast food rather than eating healthy vegetables and fruits. He preferred drinking milk, as much as 1 liters of milk per day. Neurological examination showed neurologic deficit with scale 4 of motor strength both in left arms and leg. The right side was within normal limits. In standing position, the left arm was in flexion and adduction, the left foot was positioned in plantar flexion with flexion of the phalanges. We found hemiplegic gait when he walks.
Brain MR was performed, and we found chronic infarct area in the right base of ganglia and right lateral periventricular, hemorrhagic lesion was not found. MRA and MRV showed brain vessels within normal (Figure 5).
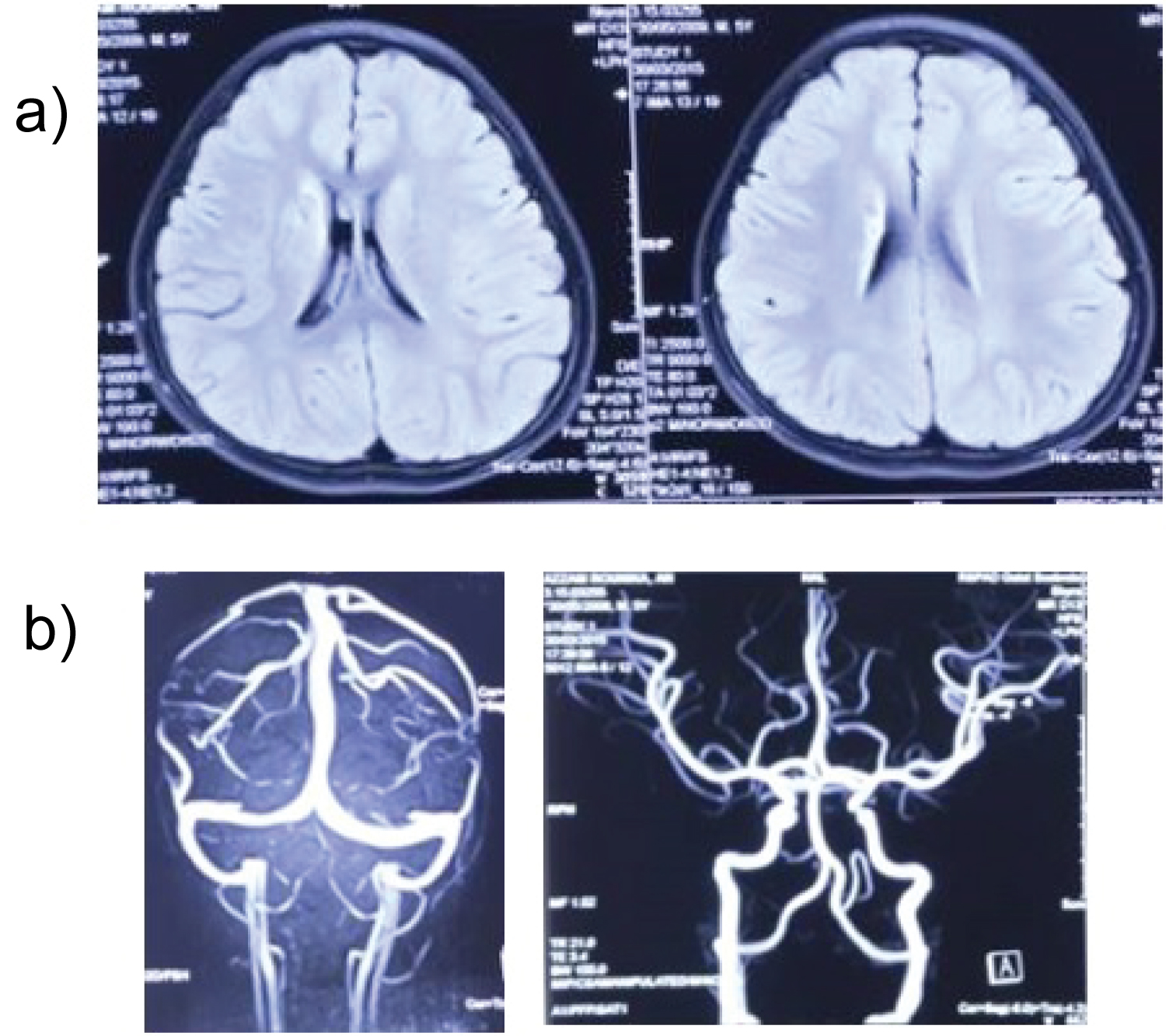 Figure 5: Brain MR imaging (a) FLAIR sequence with infarct lesion in right base of ganglia and lateral periventricular; (b) MRV and MRA imaging within normal.
View Figure 5
Figure 5: Brain MR imaging (a) FLAIR sequence with infarct lesion in right base of ganglia and lateral periventricular; (b) MRV and MRA imaging within normal.
View Figure 5
Blood examination showed increased lipid profile (increase of triglyceride and LDL).
Elective Cerebral Digital Subtraction Angiography followed by Intra Arterial Heparin Flushing (IAHF) was performed. After this treatment, we found direct improvement in left sided motor function. He was able to raise his left hand over his ear, his hand grips strength improved, and finger foot flexion a left foot plantar flexion was reduced. After 4 hours of observation, we performed perfusion MRI to compare brain perfusion before and after IAHF. Compared to pre-IAHF, we found increasing perfusion in cortical and subcortical area (Figure 6).
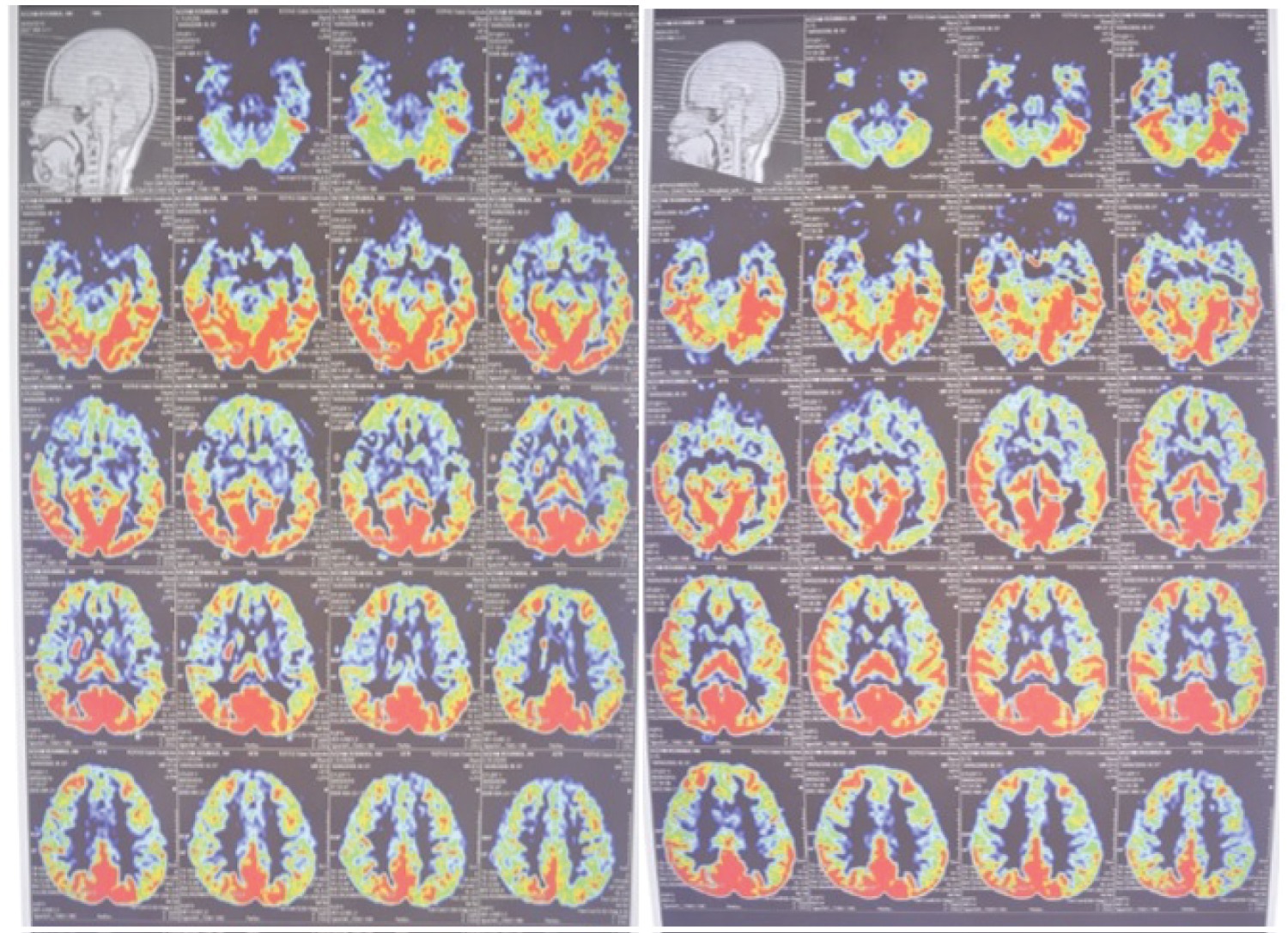 Figure 6: The perfusion image compared brain perfusion before (left) and after (right) IAHF.
View Figure 6
Figure 6: The perfusion image compared brain perfusion before (left) and after (right) IAHF.
View Figure 6
IAHF Procedure: All the IAHF procedure was performed by interventional radiologist. Fluoroscopy was performed to see the anatomical imaging. Diluted heparin was flushed intra-arterial in both right and left carotid arteries and vertebral arteries [14]. After completing the flushing process, femoral artery bleeding was stopped with vascular closure device.
After IAHF procedure, patients were monitored in recovery room for 4 hours. Vital sign measure as soon as the patients presented at the recovery room. Patients back to wardroom as soon as after vital sign stable and they regain consciousness. Patients who were discharged from hospital, underwent physical examination performed by our pediatrician, neurologic examination performed by our neurologist and puncture site examination performed by our interventional radiologist.
Based on the 2013 AHA consensus, ischemic cerebral stroke is defined as an episode of neurological dysfunction caused by cerebral infarction. To clarify, cerebral infarction is defined as cell death due to ischemia based on pathological evidence, imaging, or other effective evidence related to cerebral focal ischemic damage in certain vascular distribution or clinical evidence of cerebral focal ischemic damage based on symptoms lasting more than 24 hours or until death and other etiologies were excluded [15].
Pediatric stroke can be classified as ischemic and hemorrhagic stroke. Ischemic stroke includes arterial ischemic stroke (AIS), venous infarction caused by cerebral Sino-venous thrombosis (CSVT) or cortical vein thrombosis [13].
Cause of stroke in children is varied. High rates of childhood obesity and associated traditional stroke risk factors, such as hypertension, diabetes mellitus, and hyperlipidemia, can be increased pediatric stroke rates. Other factors such as congenital heart disease, prothrombotic states, nonatherosclerotic arteriopathies, head and neck trauma, infection [2], sickle cell diseases (SCD) and hypercoagulable states are important contributors [13]. High cholesterol and triglycerides are found in both of cases.
In both adults and children, metabolic syndrome can be affected to cardiovascular disease (CVD). There are no consensus guidelines or diagnosis criteria for metabolic syndrome in the pediatric, but syndrome metabolic in children (10-16 years-old) can be identified if central obesity plus 2 of the following 4 criteria [16]:
1. Weight Curve > 90th percentile
2. Systolic > 130 mmHg or diastolic > 85 mmHg or use anti-hypertensive medication
3. Triglyceride > 150 mg/dL
4. HDL < 40 mg/DL
5. Fasting glucose > 100 mg/dL
Central obesity, weight curve > 90th percentile, and hyper triglycerides can be found in both of this case. In previous study of population for metabolic syndrome in pediatric was 11.9% from whole population in overweight and 29.2% from whole population in obese population [16]. Based on data from Seoul national university children's hospital, metabolic disease is one of the most common risk factors for children 6-11 years-old [9].
Most children with arterial stroke present with neurologist deficit, altered sensorium, lower cranial nerve palsies and headache even symptoms of arterial stroke can be varied depends on anatomical vascular obstruction [7]. In this case, both them present with neurologist deficits, beside that child in case 1 present with dysarthria.
Diagnosis of pediatric stroke can be difficult, because a lot of condition mimicking ischemic stroke such as electrolyte imbalances, epilepsy, brain tumors must be excluded [11]. MRI of the brain is frequently used to confirm stroke because of ability to sequentially visualize soft tissue, vasculature, and quantitative hem-metabolic markers of ischemia without ionizing radiation, which is it safer than CT-Scan for children [17].
After diagnosing of pediatric stoke can be established, management strategies and recommendation are inspired still basically from adult studies. There are some existing modifications concerning anticoagulant and thrombolytics therapy [18]. Thrombolytic therapy with rTPA has been shown to significantly benefit in adults when implemented within discrete time windows but apply these therapies in children remain controversial caused by the complication from the intra-arterial thrombolysis [13]. Children are rarely been implemented this therapy because rarely once obtain cases pediatric stroke that come less than 3 hours after onset [11]. The use of antiplatelet such as aspirin, commonly used in children for preventing second stroke [13]. In recent literature has suggested that endovascular interventions may be safe and effective with modern devices especially for children with proximal large vessel occlusions [7]. Based on international guidelines, recommend the use of anticoagulation in children and selected neonates, in this case use of heparin being increase in pediatric. It associated with reduction in thrombus propagation and safe for children [19].
In another study, IAHF empirically able to provide improvement in clinical patients after chronic ischemic stroke in adult. It is modification of digital subtraction angiography (DSA) followed by direct catheter and heparin flushing. The uses of heparin as bolus and dilution in catheter for procedure intervention have been known in procedure intervention radiology [20]. Based on previous study in adult, IAHF procedure can significantly improve CBF for chronic stroke in adult. It can recanalization vessel that led to reperfusion of brain tissue and benefit for motor function recovery after stroke. This clinical improvement supported with MRA and MRV comparation before and after IAHF that shown improvement in occlusion and stenosis and it can increase perfusion after IAHF. This increasing perfusion associated with increase of cerebral blood flow that bring nutrition and oxygen to support brain cells metabolism. IAHF can giving new hope for gaining motor recovery for patient with pediatric stroke.
Pediatric stroke often missed diagnose caused by a lot of mimic stroke condition in children. It can cause delays in management and prompt treatment. This case series showed improvement after IAHF treatment in patient with late detected pediatric stroke. IAHF can be promising alternative treatment for pediatric stroke.
We would like to thank Gatot Soebroto Army Central Hospital for their invaluable supports to this study.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.