Percutaneous ablation of renal masses is an alternative to partial nephrectomy. The three main techniques for ablation of these masses are Radiofrequency ablation, cryoablation and microwave ablation.
We report a case of an 83-year-old man who underwent microwave ablation of a renal mass complicated by delayed development of an urinothorax eventually necessitating nephrectomy. Urinothorax following percutaneous renal ablation has not previously been described in the published literature.
Compared to cryoablation, MWA, has a greater potential for injury to the collecting system is higher. The diagnosis of urothorax should be considered in any patient with pleural effusion and recent ipsilateral genitourinary intervention. Ablation of previously demonstrated benign lesions is not recommended; repeat biopsy should be considered. Finally, ablation needles should never enter the renal collecting system.
Cryoablation, Microwave ablation, Renal mass, Partial nephrectomy, Urinothorax, Case report
Percutaneous ablation of T1a renal masses is an alternative to partial nephrectomy. Compared to partial nephrectomy, ablation is associated with similar local tumor control but with shorter recovery time, lower morbidity and greater preservation of renal function but with an overall reported rate of complication of 11.0% [1,2]. Radiofrequency ablation (RFA), cryoablation (CA) and microwave ablation (MWA) are the three ablation technologies used. Microwave ablation is associated with lower risk of bleeding, need for fewer probes and faster ablation times but with higher risk of damage to the collecting system [3,4]. In this case report we describe the unique complication of urinothorax after MWA of a renal tumor ultimately resulting in nephrectomy.
An 83-year-old male who presented with a growing right-sided mass, previously biopsied and shown to be an oncocytoma (Figure 1). Given the growth from 2.8 cm to 3.6 cm over 8 months, there was concern for sampling error and after multidisciplinary discussion percutaneous ablation was pursued. The patient underwent MWA of the 2.9 × 3.6 cm utilizing 3 probes at 90W for 10 minutes (Long Perseon Microthermx®) with an expected ablation zone of 4 × 5.3 cm (Figure 2). Three months after the ablation, the patient developed shortness of breath secondary to a pleural effusion and presented to OSH where he underwent multiple thoracenteses. Given the refractory nature of his effusions, he underwent placement of a tunneled pleural catheter for management of this high volume, refractory effusion. At the time of placement of this tube, urinothorax was considered as an etiology of this effusion and a sample was sent for fluid creatinine, which was 52 mg/dl (concurrent serum creatinine was 0.8 mg/dl). An excretory phase CT demonstrated accumulation of contrast in the chest, confirming the diagnosis of with urinothorax (Figure 3). A percutaneous nephroureteral (PCNU) tube was then placed for urinary diversion and output from the chest tube abated. One month later, the PCNU was removed at outside hospital with subsequent recurrence of the urinothorax. Owing to significant morbidity and frustration the patient opted to undergo right nephrectomy rather than additional stenting.
 Figure 1: 2.9 × 3.6 cm right renal mass, previously biopsied and shown to be an oncocytoma. Given interval growth, concern was for sampling error and simultaneous biopsy and ablation was planned.
View Figure 1
Figure 1: 2.9 × 3.6 cm right renal mass, previously biopsied and shown to be an oncocytoma. Given interval growth, concern was for sampling error and simultaneous biopsy and ablation was planned.
View Figure 1
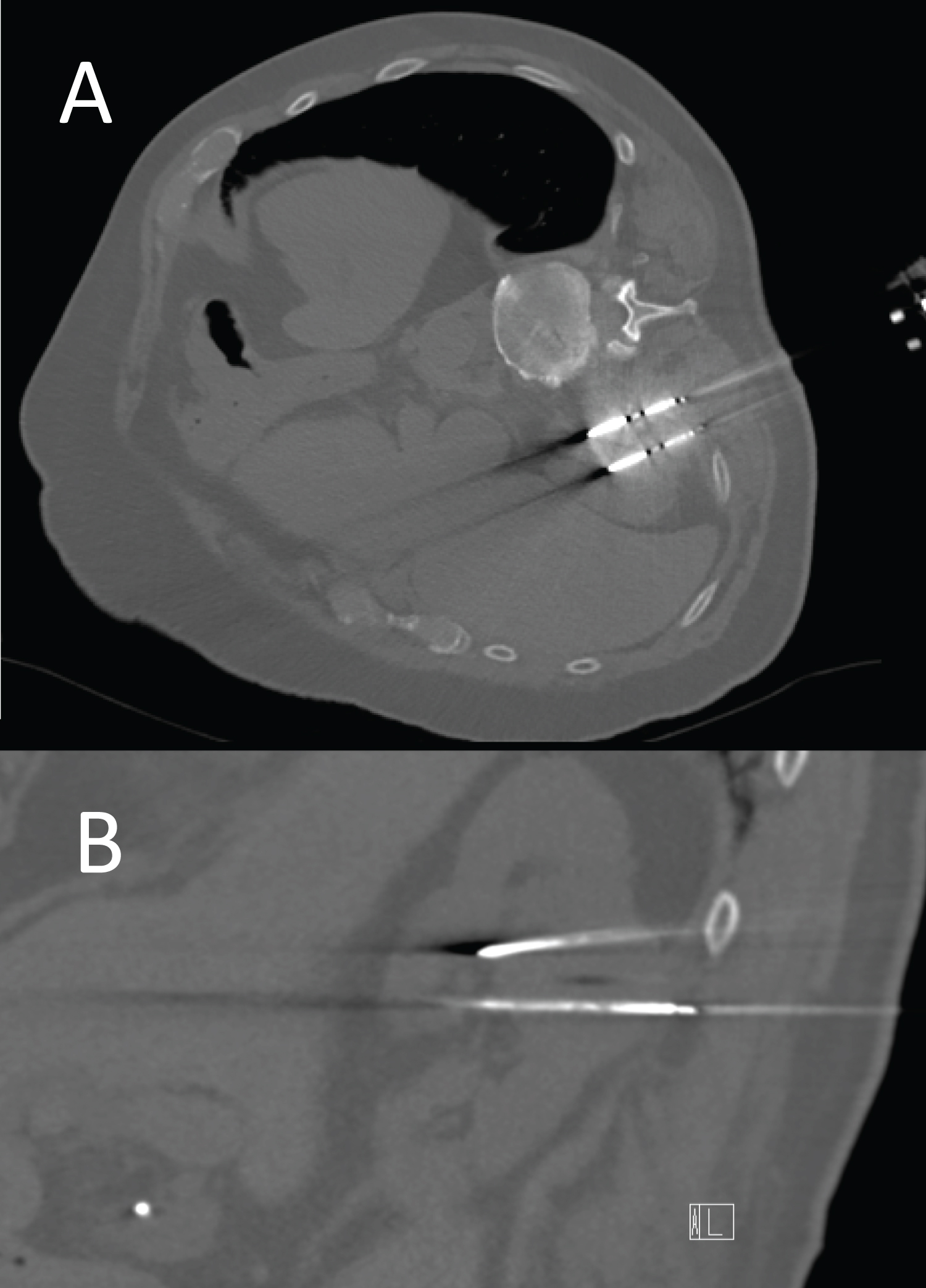 Figure 2: Axial (A) and sagittal (B) images from the ablation show 3 probes within the mass. Anterior aspects of the tips enter into the renal collecting system. The upper probe is seen to take a transpleural course. The expected ablation zone was 4 cm wide by 5.3 cm long. Repeat biopsy at the time of ablation confirmed prior diagnosis of oncocytoma.
View Figure 2
Figure 2: Axial (A) and sagittal (B) images from the ablation show 3 probes within the mass. Anterior aspects of the tips enter into the renal collecting system. The upper probe is seen to take a transpleural course. The expected ablation zone was 4 cm wide by 5.3 cm long. Repeat biopsy at the time of ablation confirmed prior diagnosis of oncocytoma.
View Figure 2
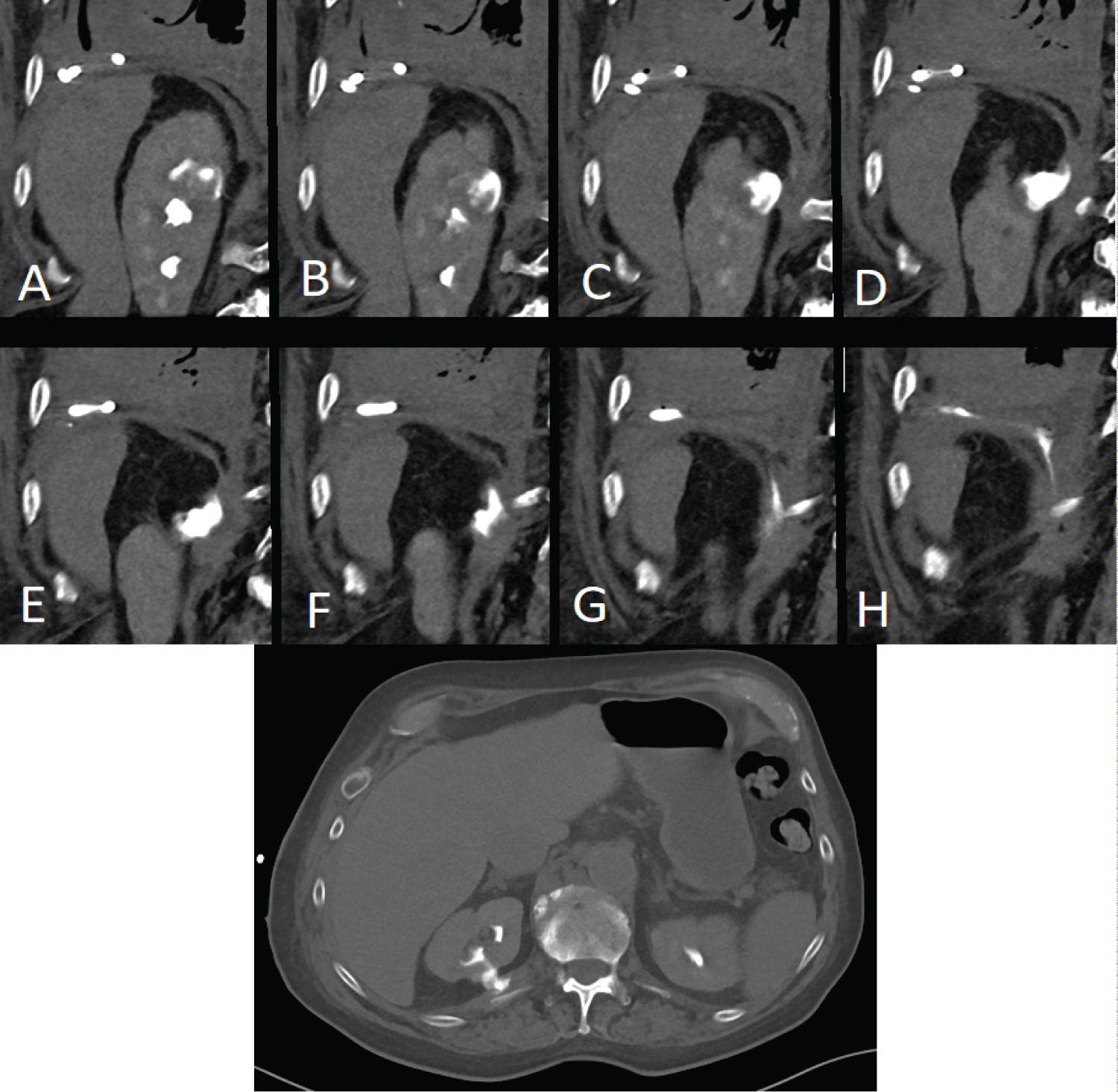 Figure 3: Serial coronal images (A-H) and axial CT (I) from a CT in excretory phase shows accumulation of contrast in the pleural space.
View Figure 3
Figure 3: Serial coronal images (A-H) and axial CT (I) from a CT in excretory phase shows accumulation of contrast in the pleural space.
View Figure 3
Urinothorax, a rare diagnosis most often seen after urologic surgery is defined as urine leakage into the chest cavity. It can be diagnosed when pleural/serum creatinine is greater than 1 [5]. If imaging confirmation is needed, a technetium 99 m renal scan or CT in excretory phase can be performed [6].
Percutaneous ablation of renal masses is a potential alternative to partial nephrectomy with an overall good safety profile [7]. Other case reports have highlighted nephrocutaneous fistulas [8], but this is the first highlighting a urinothorax following MWA. This case report demonstrates a previously unreported complication of MWA and highlights a few teaching points. First, compared to cryoablation, MWA, has a greater potential for injury to the collecting system is higher [6]. Second, while transpleural approach is often needed, one must ensure the ablation zone does not extend through the pleura, possibly by performing hydrodissection. Third, the diagnosis of urothorax, while rare, should be considered in any patient with pleural effusion and recent ipsilateral genitourinary intervention [5]. Fourth, ablation of previously demonstrated benign lesions is not recommended; repeat biopsy should be considered. Finally, ablation needles should never enter the renal collecting system (Figure 2).
Ethics approval and consent to participate: Ethical approval not required.
Patient consent obtained.
Data sharing not applicable to this article as no datasets were generated or analyzed during the current study.
The authors declare that they have no conflict of interest.
This study was not supported by funding.
MM: Reviewed data on urinothorax, wrote case report KQ: Managed patient care, helped with graphics and significant editing of the paper, BS: Managed patient care helped with writing the report.
None.