Objective: To describe the morbidity and mortality of patients with Fournier's syndrome who undergo 3-stage reconstructive surgery and their prognosis according to the anatomic affectation.
Methods: In this retrospective study, we analyzed 58 patients with Fournier's syndrome who underwent a three-stage reconstructive technique at the General Hospital Zone No. 1 of Mérida, Yucatán, by the same surgeon between 2021 and 2024. The primary endpoint was mortality of patients with Fournier's syndrome who underwent three-stage reconstructive surgery and their prognosis according to the anatomical involvement.
Results: The study closed after 3 years with 58 patients (all men; mean age 64-years). The most frequent comorbidity was diabetes mellitus in 93% (n = 54). An anatomic scale was proposed according to the affected area, which was correlated with prognostic scales and its relationship with days of hospital stay. Grade I and grade II injuries were correlated to a hospital stay of less than 7 days. The average hospital stay was 13.5 days (4-22 days). The most frequent site of affection was scrotal at 70% (N = 44), and mortality was 6.8% (N = 4).
Conclusions: Fournier's gangrene is a frequent entity in our hospital with characteristics similar to those reported in the world literature; this study is one of the largest series of cases reported so far in our country. In patients who complete the 3-stage reconstructive technique, the prognosis is promising: low urological complications and lower hospital stay and mortality than reported in other studies.
Mortality, Reconstructive surgery, Perineum, Soft tissue infections, Fournier's gangrene
Fournier's gangrene is a frequent entity in our hospital with characteristics similar to those reported in the world literature; this study is one of the largest series of cases reported so far in our country.
Fournier's gangrene takes its name from the fact that it was described in detail by the French dermatologist Alfred Jean Fournier in 1883. It is a progressive infection of the skin and subcutaneous tissues of the genital and perineal area, potentially fatal [1]. It is polymicrobial in nature, with a synergistic association between aerobic and anaerobic microorganisms. Comorbidities predispose its appearance (diabetes mellitus 40-66%, alcoholism 25-50%, or cancer), leading to a rapid advance of the infectious process and its extension to the abdominal wall and/or the pelvic limbs [2]. Comprehensive treatment should be immediate and include aggressive and extensive debridement of the infected skin and subcutaneous tissues, as well as hemodynamic, metabolic, and antibiotic support. Despite the advance in therapeutic measures, there is currently a mortality rate of up to 40% [3]. Several techniques have been used to reconstruct the tissue loss: skin grafts, transposition of the testicles and cord to a subcutaneous pouch in the thigh, pedicled musculocutaneous flap, fascio cutaneous flap, or several other types of pedicled myocutaneous flaps [4].
Given the high mortality rate of nearly 50%, the 3-stage reconstructive surgical technique, as a treatment option for Fournier's gangrene, offers a reduction in morbidity and mortality in patients treated in our hospital [5]. In the state of Yucatan, the incidence is 10.2 per 100,000 inhabitants, demonstrating that this is a disease of irrefutable importance for the urological field and for the population.
Inclusion criteria: patients diagnosed with perineal necrotizing fasciitis (Fournier syndrome) at the General Hospital Zone No. 1, aged between 40-85 years, who have undergone surgery.
Exclusion criteria: Those who could not be followed up due to incomplete records. Those who did not complete the three procedures due to mortality associated with primary pathologies independent of necrotizing fasciitis.
In this retrospective study, the records of 58 patients with Fournier Syndrome were identified, who underwent a 3-stage reconstructive technique because they did not present results with minor surgery during the period from 2021 to 2024.
Prior to the three-stage reconstructive technique, all patients were impregnated with a broad-spectrum antimicrobial.
All patients underwent the APACHE III score collected 72 hours after admission, was used to measure the severity of the patient's illness.
The first surgical stage consists of damage limitation and extension analysis. In the second surgical stage, it was necessary to wash and prepare the area to be remodeled with the joint creation of the testicular resting space delimited by the fascia of the adductor muscles of the proximal lower limb. Finally, in the third surgical stage, the wound is remodeled and addressed. The surgery was performed on patients with extensive involvement that could not be resolved with minor surgery.
The 3-stage reconstructive technique can be summarized as follows (Figure 1, Figure 2, and Figure 3).
 Figure 1: Stage I: Bilateral testicular and spermatic cord dissection.
View Figure 1
Figure 1: Stage I: Bilateral testicular and spermatic cord dissection.
View Figure 1
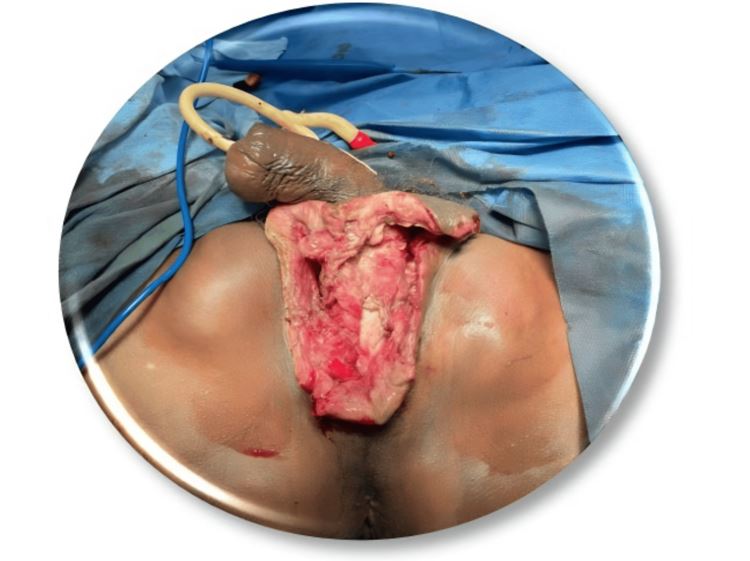 Figure 2: Stage II: Formation of cutaneous flaps and bilateral inguinal neocavity.
View Figure 2
Figure 2: Stage II: Formation of cutaneous flaps and bilateral inguinal neocavity.
View Figure 2
 Figure 3: Stage III: Perineal-scrotal reconstruction with fascial facing and cutaneous flaps.
View Figure 3
Figure 3: Stage III: Perineal-scrotal reconstruction with fascial facing and cutaneous flaps.
View Figure 3
The first step is the analysis and limitation of the tissue injury with bilateral testicular and spermatic cord dissection. The second step is the formation of cutaneous flaps and bilateral inguinal neocavity for the testicles. And finally, the perineal-scrotal reconstruction with fascial facing and cutaneous flaps.
Between March 25, 2021, and March 25, 2024, a total of 58 patients diagnosed with Fournier's gangrene underwent a three-stage surgical procedure by the same surgeon. This study did not include a control group for conservative treatment of Fournier's gangrene, as the mortality rate for this condition exceeds 50% with conservative treatment and is considered a surgical emergency.
Of the 58 patients, 45 belonged to a low socioeconomic level and 13 belonged to a middle socioeconomic level. Socioeconomic level was measured based on each patient's average monthly income, with a low income being less than 14,000 Mexican pesos and a middle income being >14,000 Mexican pesos. None of them had a high socioeconomic level of >40,000 pesos. The main comorbidity was diabetes mellitus in 93% of patients (N = 54) and arterial hypertension in 7% (N = 4). All patients arrived at the hospital via the emergency department. The main clinical manifestation of all patients was pain in the affected area in 90% of subjects, fever in 67.5%, and purulent discharge in 55%. The average time to onset of symptoms before seeking medical attention was 7.8 days, with a range of 2-18 days. Upon arrival, all of them underwent wound cultures, in which the most frequently isolated microorganisms were, firstly, Proteus mirabilis (70%) and secondly, Escherichia coli (30%). All patients received empirical antibiotic therapy based on a third- generation cephalosporin upon arrival and then antibiotics according to the isolated organism and its susceptibility. The antibiotics were continued for 14 days after the first surgical procedure. Four degrees of involvement were categorized by initial anatomical involvement, the most frequent being the scrotum at 70% (N = 44), the second being the perineal (N = 10), and the penis and foreskin involvement (N = 4). All patients underwent a three-stage surgical procedure. Intraoperative bleeding was assessed and documented at 100 to 200 ml. The average surgical time was 30 to 40 minutes for the first intervention, 60 to 70 minutes for the second intervention, and 20 to 30 minutes for the third intervention.
All patients underwent the APACHE III score, which considers the following variables: age, previous health status, temperature, mean arterial pressure, mean heart rate, respiratory rate, partial pressure of arterial oxygen, acid-base imbalance, renal function, hematocrit, leukocyte status, albumin, bilirubin, glucose, and assessment of neurological status. The APACHE III score, collected 72 hours after admission, was used to measure the severity of the patient's illness; the total score on this scale is a number between 0 and 299, with a higher score indicating greater severity.
In our opinion, the APACHE III score is strongly associated with mortality from Fournier's gangrene; patients with an elevated APACHE III score often present with an altered state of consciousness, advanced age, elevated body temperature, low mean arterial pressure, poor oxygenation, altered leukocyte status, high albumin and creatinine levels, and the presence of concomitant diseases such as diabetes or acute renal failure. All of these factors are independently related to mortality in Fournier's gangrene.
We observed a significant change in mortality in our patients with a score equal to or greater than 50 on the APACHE III scale.
The level of affection was correlated with the average Apache III score for each patient, with a Pearson correlation of 0.94 obtained by statistical analysis. In turn, the Fisher test was applied in two large total groups to assess its dependence on the length of hospital stay (less than 7 days and greater than 7 days), with a two-tailed P of 0.01.
The primary endpoint was mortality of patients with Fournier's syndrome who undergo 3-stage reconstructive surgery and their prognosis according to the anatomical involvement (Table 1).
Table 1: Proposal for an anatomical scale. View Table 1
Grade I and grade II injuries were correlated to a hospital stay of less than 7 days.
The overall mortality rate was 4 patients, all due to sepsis leading to multiorgan failure. All deaths occurred in patients who had been hospitalized for more than 7 days.
Finally, the mortality rate in our series was 6.8%, much lower than in published series (Table 2, Table 3, Table 4, Table 5 and Table 6).
Table 2: Associated Pathologies. View Table 2
Table 3: Site of involvement. View Table 3
Table 4: Analysis of different variables. View Table 4
Table 5: Isolated germs. View Table 5
Table 6: mortality rate in other series. View Table 6
Currently our anatomic scale was validated and demonstrated at the 40th Annual European Association of Urology Congress in Madrid 2025, under abstract number AM25-0573
This study represents one of the largest series of Fournier's gangrene reported in the world literature and the largest described to date in our country.
The average age at presentation in our patients was 64 years, higher than the average reported in other existing series. In another study conducted in Mexico, López Samano, et al. reported 40 patients treated at the CMN Siglo XXI from 1996 to 2006, finding a mean age of 59 years at presentation [6]. Azolas reported a mean of 58 years in his series of 31 Chilean patients treated between 2000 and 2007 [7]. In an older study, Nisbet and Thompson reported 26 patients treated in Texas, USA, between 1994 and 2000, finding a mean age at diagnosis of 48 years, it seems that there has been a gradual increase over time in the mean age of 58 years. Presentation of Fournier's gangrene, which could be explained by a better general control of chronic degenerative diseases, particularly diabetes [8].
Regarding comorbidities, we also found diabetes as the main entity associated with Fournier gangrene, present in nearly 90% of cases, much higher than the 55% found by López-Samano, et al. in the study conducted at the CMN Siglo XX [6]. Azolas reported diabetes in 35% (11 of 31) in his series of Chilean patients [7]. Nisbet and Thompson reported a prevalence of diabetes of 77% (20 of 26) in their series of North American patients [8].
Castillo H, et al., reported the results observed in a series of patients diagnosed with Fournier's gangrene who underwent surgical cleaning with debridement plus broad-spectrum antibiotic therapy. It was performed on 56 patients diagnosed with Fournier's gangrene. Mortality attributed to the disease was 48.2%. The most frequently associated pathology was diabetes (66.6%) [9].
There are reconstructive options such as the superomedial fascio cutaneous pedicle flap of the thigh, preserving the arterial pedicle, capable of reconstructing extensive scrotal defects. It offers some advantages: It is a single procedure, achieves a reasonable aesthetic result, and preserves sexual identity, without circulatory compromise and preserving sensitivity [10]. A limitation is its transverse dimension and that, in many cases, bilateral pedicle flaps are required to reconstruct the entire scrotum. Likewise, the patient is subjected to an additional surgical event, and there is a risk of flap necrosis. Not to mention that this procedure is not routinely performed by a urologist [11].
Thus, Larsson, et al. described in a series of cases the usefulness of a combined surgical approach to Fournier's Gangrene in three stages: A first stage of wound control through aggressive debridement and negative pressure therapy, followed by a stage of temporization that combines the use of dermal matrix and negative pressure therapy, and finally a stage of reconstruction to provide final coverage of the defect [12].
This study has several limitations. Accrual was affected by several factors, including that not all patients underwent step 2 reconstructive surgery, since those without extensive testicular involvement did not undergo a new inguinal cavity. Another limitation of the study is that some patients received antibiotics for longer than 14 days, some up to 21 days with carbapenems, which may skew the mortality rate considering the 3-step surgery. Despite these limitations, our study is significant and can be replicated.
Fournier's gangrene is a common entity in our hospital with characteristics similar to those reported in the world literature, predominantly in men, and with diabetes as its primary comorbidity; this study is one of the largest case series reported to date in our country. In patients who complete the three-stage reconstructive procedure, the prognosis is promising: low urological complications and lower hospital stays and mortality rates than those reported in other studies. This study is significant because our 3-stage technique can be replicated by other urological surgeons in different parts of the world, and the new anatomical scale can be used to stratify patients who will require a hospital stay of more than 7 days and who have a higher tendency to mortality.
Human subjects: Consent for treatment and open access publication was obtained or waived by all participants in this study. Mexican Institute of Social Security issued approval 339001250100/CCEIS/0165/2025. Consent for treatment and open access publication was obtained or waived by all participants in this study. Mexican Institute of Social Security issued approval 339001250100/CCEIS/0165/2025. Written informed consent was obtained from the patient for the publication of this case report and accompanying images. The study was registered in ClinicalTrials.gov (identifier: NCT06809738).
Animal subjects: All authors have confirmed that this study did not involve animal subjects or tissue.
Conflicts of interest: In compliance with the ICMJE uniform disclosure form, all authors declare the following:
Payment/services info: All authors have declared that no financial support was received from any organization for the submitted work.
Financial relationships: All authors have declared that they have no financial relationships at present or within the previous three years with any organizations that might have an interest in the submitted work.
Other relationships: All authors have declared that there are no other relationships or activities that could appear to have influenced the submitted work.
Martín G. Mijangos Carpenti contributed equally to the work and should be considered co-first authors.