Introduction: Myxoid liposarcoma is a sarcoma of the supporting tissues. However, its superficial location is rare. It sometimes takes on an appearance that leads to confusion. In these rare clinical forms, its diagnosis is not often considered.
Case presentation: We report a case of myxoid liposarcoma of the bladder with rare exophytic development. It developed around a cystostomy tube. The diagnosis was made after histological examination of a biopsy of the mass. Excision of the mass combined with radiotherapy was proposed. The mutilating nature of the treatment prevented it from being carried out. The course was negative.
Conclusion: This atypical mode of revelation may be a source of diagnostic delay.
Cystostomy, Myxoid liposarcoma, Bladder
Non-epithelial tumours of the bladder are rare. They account for approximately 5% of all bladder tumours. Myxoid liposarcomas are non-epithelial tumours arising from connective tissue [1]. Its mode of appearance can sometimes be unusual. We report a case from our department. In this case, the mode of onset led us to think of a benign tumour of the abdominal wall. Biopsy enabled us to correct the diagnosis. We will focus on the clinical aspects.
The patient was a 61-year-old man. He presented with pelvic pain associated with a mass around the cystostomy. His history was marked by trauma to the perineum with a uro-perineal fistula 30-years ago. Examination of this dysuria in 2019 revealed narrowing of the membranous urethra. A 2-stage urethroplasty using the Bengt Johanson technique was performed. This was unsuccessful. A definitive cystostomy was performed in 2020. During the follow-up, he was consulted about an ulcerating mass associated with pelvic pain. This pain had been resistant to the usual analgesics for 6 months. Clinical examination showed an average general condition (WHO status performans 2/4).
There was an ulcerating mass around the cystostomy orifice. The mass measured approximately 5cm in diameter. The base of the mass was hard (Figure 1). The cystostomy tube drained cloudy urine. There was no palpable superficial adenopathy. The probable diagnosis was hypertrophic peristomal scarring. Cytobacteriological examination of the urine isolated an Escherichia coli infection. We administered a 10-day course of antibiotics based on imipenem and amikacin, combined with replacement of the cystostomy tube. MRI showed a heterogeneous mass with high T2 intensity and an “amorphous, lacy appearance” (Figure 2). The evolution was pejorative with an increase in the mass associated with a worsening of his general condition. A biopsy with histological examination of the mass was subsequently performed. The patient died on day 17 of hospitalisation in septic shock, despite resuscitation measures. Histological examination revealed sarcomatous proliferation (Figure 3) with lip oblasts, suggesting myxoid liposarcoma of the bladder.
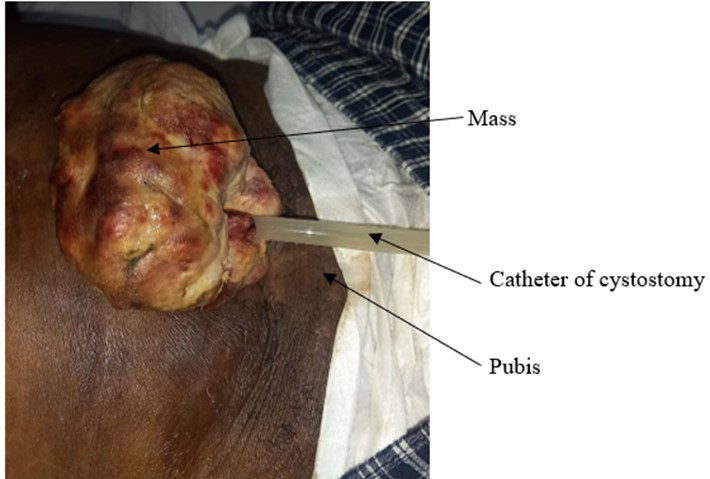 Figure 1: Peristomal ulcerating mass.
View Figure 1
Figure 1: Peristomal ulcerating mass.
View Figure 1
 Figure 2: Abdominopelvic MRI (cross-section through the iliac crests).
View Figure 2
Figure 2: Abdominopelvic MRI (cross-section through the iliac crests).
View Figure 2
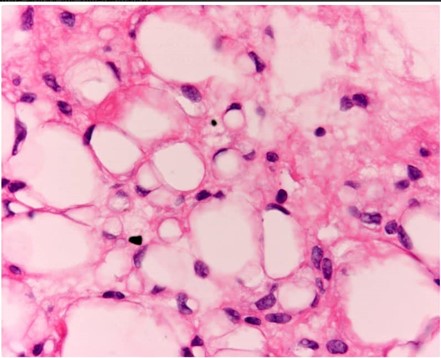 Figure 3: Histological appearance of the biopsy specimen.
View Figure 3
Figure 3: Histological appearance of the biopsy specimen.
View Figure 3
Liposarcomas are rare neoplasms. Some authors describe their origin as allantoic remnants [2,3]. Localization in the bladder is exceptional. The preferred sites for myxoid liposarcomas are the buttocks, retroperitoneum, trunk, head and neck, and wrist [4,5]. In typical forms, they are intra abdomino pelvic. It may present as a palpable, painless mass. Diagnosis then combines imaging techniques and anatomical pathology [6].
Painless haematuria (79%) and irritative bladder symptoms (16%) are the main modes of revelation of bladder tumours [7]. The atypical presentation of the tumour and the absence of specific urinary signs have been the main factors delaying diagnosis. The expansive nature of the mass led us to perform a biopsy. The ecosystem formed by the bladder mass led to repeated urinary tract infections. Ultimately, these infections led to the patient's death from septic shock.
Myxoid liposarcoma of the bladder is a rare tumour. It has no specific clinical signs. It is therefore difficult to diagnose. Imaging and biopsy are the main diagnostic tools. Any mass growing around a cystostomy catheter should be biopsied.
Not applicable.
The authors declare no conflict of interest.
Evrard Kouame Yao: Conceptualization, writing-original draft; project administration; resources.
Abroulaye Fofana: Review and editing
Donafologo Yeo: Writing-review and editing; supervision.
N’Zibla Yebouet: Supervision; writing – review and editing.
Sylvanus Koui: Pathology data Curation
Tawakaltu Adebayo: Writing-review and editing; resources.
Michel Tuo: Review and editing
Noel Coulibaly: Writing-review and editing; supervision.