Background: Cardiovascular diseases (CVDs) are the major causes of death and disability in Australia. The number of migrants from South and South-East Asian countries to Australia is increasing rapidly and are at increased risk of developing CVDs. This study assessed the absolute CVD risk among South and South-East Asian migrants living in Greater Sydney, Australia.
Methods: This is a descriptive cross-sectional study conducted among 129 adult participants aged 40 years and above. We used the World Health Organization (WHO) 2019 non-laboratory ten-year CVD risk calculation chart to calculate CVD risk. Additionally, the CVD risk factors such as smoking, alcohol use, unhealthy diet, and physical inactivity were also assessed and were analysed using SPSS version 26.0.
Results: The mean age of the study participants was 48.43 (7.41) and 56.6% were females. Most of the participants (86%) had low CVD risk with CVD risk scores < 10% and 14% showed elevated CVD risk with CVD risk scores > 10%. Multivariate analysis showed that those migrants with alcohol consumption behaviour, had a personal history of diabetes and those who were overweight/obese had an increased risk of developing CVD at 10 years.
Conclusion: This suggests the need for developing and implementing culturally appropriate intervention approaches to improve unhealthy lifestyle behaviours and minimize the CVD risk factors among these migrants living in Australia.
Cardiovascular diseases, Migrants, Risk assessment, South and South-East Asians
Noncommunicable diseases (NCDs) are responsible for 71% of global deaths every year [1]. The major NCDs include cardiovascular disease (CVDs), cancers, respiratory diseases, and diabetes. Cardiovascular diseases are the leading cause of death worldwide, accounting for 17.9 million deaths, or 44% of all NCDs related deaths annually [1-3]. Over seven million Australians suffer from chronic NCDs, including CVDs [4]. Annually, 43,447 people die due to CVD in Australia, 27% of total deaths [5]. Currently, it is estimated that 1.2 million Australians are suffering from CVD, which accounts for 6.9% of the total NCD burden in 2015 (8.6% for males and 5.0% for females) [4]. Evidence suggests that the migrant population is disproportionately affected by the increasing burden of NCDs in Australia, including CVDs, compared to another ethnic group in Australia [6,7]. South Asian have increased morbidity and mortality due to CVD when compared with people from other origins. The CVD risk is higher among South Asian immigrants in Australia compared to the Anglo-Australians [8].
Studies suggest that there had been not much significant difference in the disease burden even after migration [9]. Cardiovascular Disease is an umbrella term for many circulatory system-related disorders such as Ischemic Heart Diseases, Hypertension, Heart Failure and many more [3,10]. There are two different risk factors for developing the CVDs; direct risk factors that include genetics, high blood pressure, increased total cholesterol or LDL cholesterol (hypercholesterolemia), obesity, increased body mass index and history of diabetes, while indirect risk factors include sedentary lifestyle, physical inactivity, food & nutrition patterns, socio-economic and environmental factors. Most of these risk factors are preventable to a greater extent [3,11].
Australia, a multicultural country, has witnessed a dramatic increase in migrant population, especially the Asian migrants in recent years [12]. South Asian migrants seeking settlement in Australia have been rapidly increasing since 2006, 28% annually [5]. The Australian Bureau of Statistics estimated that these numbers will proliferate in the upcoming years, especially in the major metropolitan cities such as Sydney, Melbourne, and Brisbane [13,14].
South Asians are prone to developing CVD related disorders compared to people from other ethnic groups due to combined factors such as food patterns, lifestyle, and genetic susceptibility [15]. Dietary acculturation is the other cause of developing CVD and other NCDs among the migrant population [12]. Traditional South Asian food also consists of excessive fat, sugar and refined carbohydrates are the recognised risk for developing CVDs [16]. A study by Guo, et al. [12] revealed that South-East Asians are 10-20% more likely to get treated for hypertension or hypercholesterolemia and are 40-60% more likely to suffer from diabetes. Furthermore, the American Heart Association study elaborates that South Asians immigrants engaged in less physical activity than other ethnic groups and are also less aware of dietary risks of developing CVD [17]. A study conducted among the migrants revealed that the migrant's population in Australia face a higher disease burden than the mainstream population, yet they are less represented in the research and government programmes [7].
Of the total NSW population, nearly 60% living in Sydney and the greater Sydney are of Asian ancestry. According to the recorded birthplace of residents from greater Sydney residents, South Asian and South-East Asian migrants contribute nearly 1/10th of the total population living in Sydney [5]. It is well documented migrants' population from all over the world including South Asian migrants have contributed significantly to the economy and development through labour productivity and contributing to higher GDP levels. However, very little research has been done to explore the chronic disease status among South Asian migrants. The health of the migrant populations holds great importance for Australian society, however, very little is known about the distribution of absolute CVD risk among South and South-East Asian migrants. This study estimated the absolute CVD risk among the adult migrants from countries of South and Southeast Asians using the 2019 WHO CVD risk prediction chart [18].
This is a cross-sectional study conducted among the South and South-East Asian migrants living in greater Sydney, NSW Australia. In this study, we defined South and South-East Asian migrants to those coming from Sri-Lanka, Nepal, India, Pakistan, Bangladesh, and the Philippines. South and South-East Asian migrants aged 40-74 years, of both genders, residing in suburbs of south and southwest Sydney were included in the study. The age categories were selected based on the CVD non-laboratory risk prediction chart. The South and South-East Asian migrants under the age of 40 years and above 74 years or people diagnosed with cardiovascular diseases, or pregnant women were excluded in the study.
In order to estimate sample size for this study, we reviewed a range of published literature conducted both in high income and low- and middle-income countries [19-23]. Studies conducted in Bangladesh [22] and Nepal [23] were considered as basis for estimating sample size for this study. The sample size for the study was 129 which was estimated using Cochran's sample size formula [24] based on the following assumptions: prevalence = 13.6% [23], 90% of confidence interval, and 5% margin of error.
A snowball sampling strategy was used to recruit the participants for this study. Snowball sampling is the technique of referring or suggesting the potential participants by enrolled individuals. In this study, enrolled individuals were asked to contact the potential participants to participate in the study. Those who were interested were then contacted via text messages, e-mail, or mobile phone only after obtaining permission to contact them. This process continued till the desired sample was achieved from the selected study sites.
This study adopted the 2019 WHO CVD risk assessment tool to estimate the risk for cardiovascular diseases [25]. Data collection for this study was performed during the months of February and May 2020. Due to an ongoing COVID-19 pandemic and the restriction imposed, the data were collected using an online survey questionnaire. Qualtrics online survey software was used for data collection and the link of survey questionnaires was provided to study participants through Facebook, messenger, WhatsApp and email. Also, the trained postgraduate level research students with public health background collected the data through a face-to-face survey where possible adhering to the social distancing rules and taking recommended protective measures. The purpose of the study, their voluntary participation and confidentiality were explained and assured to each participant. Both the verbal and written informed consent was obtained from the study participants prior to survey. Ethical approval for this study was obtained from the Human Research Ethics Committee (HREC) of Central Queensland University (HREC#2020094).
The questionnaire consisted of a range of variables composed in three different sections which was adapted from WHO STEPS Questionnaire to fit in to this study. The initial section included socio-demographic variables such as, age, gender, educational and employment status, and yearly income. This was then followed by personal history including smoking and drinking behaviours, dietary habits, physical activity, history of high blood pressure, diabetes, and CVDs. The final section included 2019 WHO cardiovascular non-laboratory risk prediction charts for South Asians and South-East Asians that included information on age (in years), gender (male and female), smoking status (smoker and non-smoker), body mass index (< 18.5, 18.5-24.9, 25-29.9 and ≥ 30) and systolic blood pressure [25]. The 2019 WHO cardiovascular non-laboratory risk prediction charts stratified the levels of risks into five categories: very low risk (< 5%), Low Risk 5-10%, high risk 10-20%, high risk 20-30% and very high risk > 30%. The CVD risk prediction chart provides an approximate estimate of the CVD risk in next 10 years for those who are not suffering or have an established diagnosis of coronary heart disease, stroke or atherosclerotic heart diseases [18,25].
Statistical analysis was performed using the statistical Package for Social Sciences (SPSS) version 20. Dataset from the Qualtrics software was exported to SPSS and data from face-to-face interview was manually entered into SPSS. Mean and the standard deviations were reported for the continuous variables while frequencies and percentages were reported for categorical variables. Chi-square test was performed to identify the factors associated with the CVD risk. Multivariate logistic regression test was used among the covariates that were significantly associated (p-value < 0.05) with the dependent variable.
A total of 193 participants were enrolled in the study. Of whom, 34 participants were excluded due to incomplete data and further 30 were excluded because they had a history of stroke and other CVDs. Therefore, altogether 129 participants were included in the study and were analysed (Figure 1).
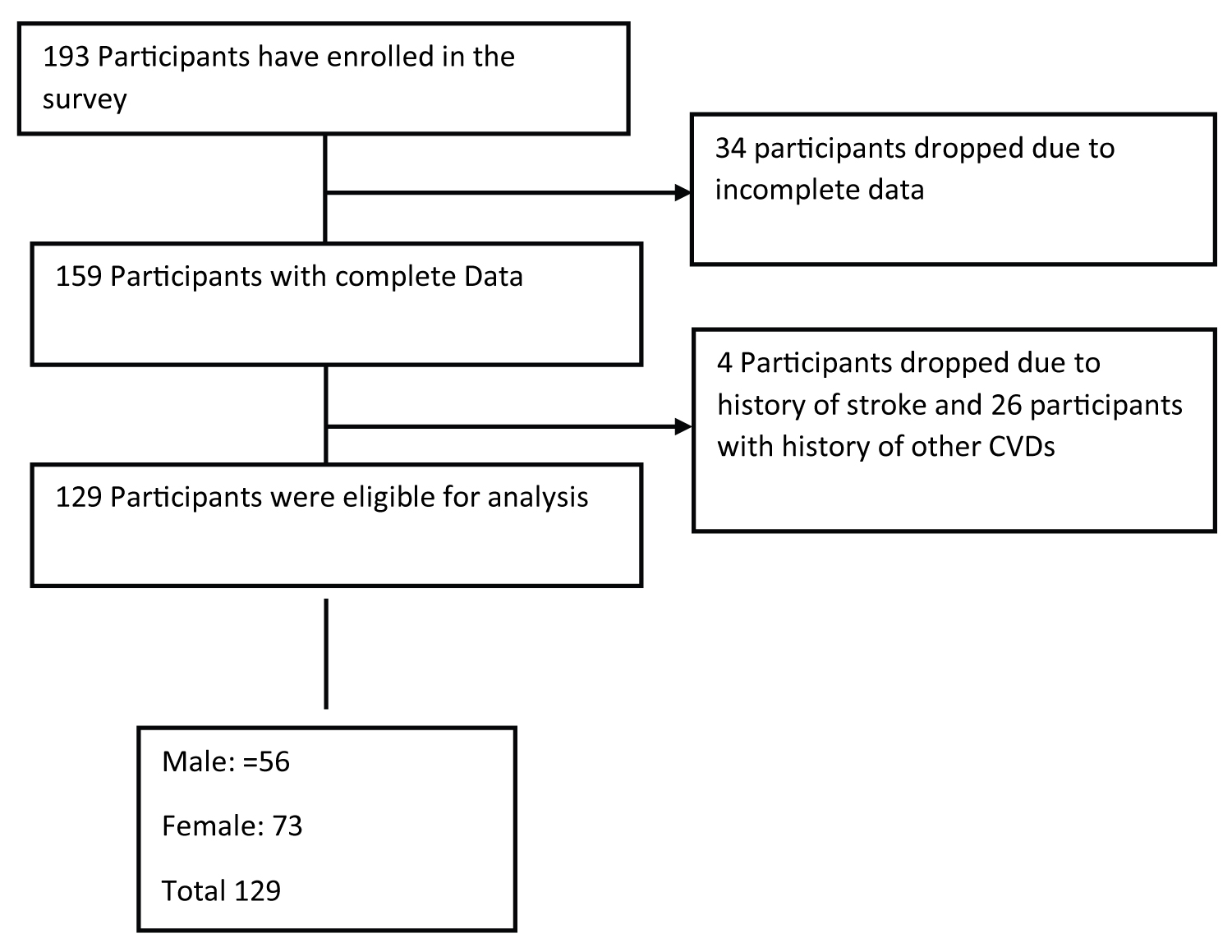 Figure 1: Recruitment of participants in the study.
View Figure 1
Figure 1: Recruitment of participants in the study.
View Figure 1
Of total subjects, majority of study participants were from Philippines (34%), followed by India (22%), Sri-Lanka (20%), Pakistan (11%), Nepal (10%) and Bangladesh (3%). The mean age of the study participants was 48.43 (±7.41) years and majority were females (56.6%). Over half (58.9%) attained the higher level of education (university degree), 79.8% were employed and 59.7% had annual income of AU$45,000 or above (Table 1).
Table 1: Socio-demographic and behavioural characteristics of study participants by gender. View Table 1
The overall behavioural history of the study participants and its gender-wise distribution has been presented in Table 1. The prevalence of tobacco use (smoke or smokeless forms) was 26.4%. Tobacco uses among the male was 44.6% while in females was 12.3%. The prevalence of alcohol consumption was 53.5% among the study participants. The proportion of alcohol consumption among females was 50% while in male was 56.2%.
The intake of five or more servings of fruits and vegetables a day was 21.7% and its proportion was higher among female (23.3%) than male (19.6%). Similarly, 45.7% participants have the usual habit of taking additional salt or a salty sauce in their meal and 75.2% usually consume fried/oily processed food or fast food in their meal. The practice of at least 150 min of moderate to vigorous physical activity a week was present in 44.6% of male and 46.6% of female. Almost two-third (64.3%) participants reported that they have a family history of hypertension, followed by CVDs (41.9%) and diabetes (16.3%).
The self-reported prevalence of diabetes was 19.4% and was most common among females (72%). Almost a quarter of participants (24.8%) reported having hypertension, (Blood pressure ≥140/90). The overall mean BMI was 25.22 (±3.85) Kg/m2, with overweight (41.9%) and obese (11.6%). Overweight and/or obesity were common among the females (63.8%).
Most participants (62%) had a very low risk (< 5%), followed by 24% with low risk (5-10%), 12.4% with moderate risk (10-20%) and 1.6% with high risk (> 20%). The distribution of elevated risk (> 10%) of CVD among females was higher (17.8%) than the male (8.9%). However, gender was not found to be associated with the development of CVD risk. Alcohol use, body mass index, personal history of hypertension and diabetes and family history of diabetes were statistically significant with the CVD risk during the Chi-square analysis. (Table 2). The stepwise multivariate logistic regression analysis showed that being overweight/obese (ORA = 7.71, 95% CI: 1.39-42.66), alcohol use (ORA = 4.77, 95% CI: 1.16-19.68) and personal history of diabetes (ORA = 7.89, 95% CI: 2.05-30.39) were significantly associated with the absolute 10-year CVD risk (Table 3).
Table 2: Socio-demographic and behavioural factors with elevated 10-year CVD risk. View Table 2
Table 3: Associates of elevated ten-year CVD risk among South and South-East Asian migrants. View Table 3
The purpose of this is study documenting the 10-year CVD risk among south and South-East Asian migrants living in Australia. The estimated 10-year CVD risk was calculated using WHO recommended CVD risk calculation tools. This study revealed that 14% of study participants had an elevated (> 10%) risk of developing CVD at ten years. The NCD risk factors such as alcohol consumption, being overweight/obese and those with personal history of diabetes have increased risk of developing CVD in 10 years. The findings of this study showed that most of the adult migrants had relatively low CVD risk. However, those with presence of NCD risk factors such as drinking alcohol, overweight/ obesity, personal history of hypertension, diabetes, and those with family history of diabetes were at greater risk of developing CVD at 10 years. Majority (86%) of participants had low estimated risk (< 10%). However, the rest of the participants are at a significant risk of developing fatal or non-fatal CVD events in 10 years. These findings are concordance with the studies conducted in Bangladesh, Nepal and Sri-Lanka [18,23,26]. In our study, gender was not associated with the estimated overall risk of CVD. This finding is consistent with the study conducted in Nepal [23,27].
The current use of any form of tobacco among the migrants was 26.4%, which is like the findings reported by the studies conducted among South Asian immigrants in the United Kingdom and UAE [28,29]. The higher prevalence of alcohol consumption was found among the participants, 53.5%. This might be due to the acculturation and feeling of socialization [30,31]. The intake of five servings of fruits and vegetables in a day among the participants was 21.7%. A systematic review and meta-analysis of 43 studies assessing fruits and vegetable intake among the south Asians revealed very low intake of fruits and vegetables [32]. The proportion of taking an additional amount of salt during meals was 45.7%. The increased use of salt or additional use of salt may be because the major cuisine of Southeast Asians includes traditional salt rich and the fermented foods that contribute for higher use of salt [33]. Also, 75.2% of participants always or often consume fat rich food or oily food or processed food in their diet. South Asians have a culture of cooking spicy or foods rich in fat during the occasions and social functions or gatherings [34-36].
More than half (54.3%) of participants were physically inactive (< 150 min of physical activity a week). The patterns of relatively low engagement in physical activity among migrants could be due to misconceptions on physical activity, long working hours, and poor family support especially for females [37-39]. Awareness rising and culturally sensitive physical activity programs are to be developed and implemented to motivate and facilitate the South and South-East Asian immigrants to undertake regular physical activity.
Those South and South-East Asian migrants currently consuming alcohol were more than four times likely to develop CVDs than non-alcohol users. This finding is supported by the review, which stated that harmful use of alcohol increases risk of developing CVD, such as stroke, hypertension [40,41]. Alcohol consumption affects multiple aspects of the cardiovascular system leading to high mortality in ischemic strokes and ischemic heart attacks. However, studies also reported that lower levels of alcohol use has protective effects against hypertension, ischemic stroke [40] and also reduces the risk of developing CVD [42].
Our study revealed that those who are overweight and/or obese are more than seven times likely to develop CVDs in long run. This finding is consistent with the findings from Elagizi, et al. [43] that stated overweight, and obesity impacts the cardiac structure and function worsening the physiological parameters which ultimately promotes in developing CVD. Similarly, our study revealed that those with the history of diabetes mellitus are nearly eight times more likely to develop CVDs in the long run. This finding is consistent with several studies conducted among Asian migrants. It is evident that Diabetes mellitus is a risk factor for CVD and has increased risk of morbidity and mortality [44]. Moreover, cardiovascular events were almost 50% higher in South Asians with type 2 diabetes conditions [45-47].
The primary strength of this study is that this is the first study to assess 10-year CVD risk among South and South-East Asian migrants living in greater Sydney, Australia. Second, 10-year absolute CVD risk was calculated using the 2019 WHO cardiovascular non-laboratory risk prediction charts for South Asians and South-East Asians. This study involved a comprehensive analysis to identify the associated risk for developing CVD. As like other studies, this study has some limitations to be considered. This study used cross-sectional study design; the direction of causality cannot be established between the dependent and the independent variables. This study was conducted among the migrants of some Southeast and South Asian countries, and a few were countries representing Southeast Asia and residing in the greater Sydney NSW. The findings should be cautiously used in other settings than the primary health care. Additionally, due to the COVID-19 restrictions, the questionnaire was self-administered where the participants might have under-reported and there may also exist some errors in measuring the blood pressure, body height, and weight. Moreover, the use of snow-ball sampling might have generated some level of sampling bias to this study.
We conclude that a reasonably low proportion of adult migrants demonstrated risk of developing CVD in 10-year time. However, those with presence of NCD risk factors such as drinking alcohol, overweight/obese and personal history of diabetes were at greater risk of developing CVD than others. This suggests the need for developing and implementing culturally appropriate intervention to screen CVD risk factors and addressing lifestyle behaviours that escalates the risk factor for CVD among South and South-East Asian migrants living in Australia. We also highlight the need of a large-scale study focusing on identifying high risk Australian migrants' population for developing CVD.
The ethical approval for this study was obtained from the Human Research Ethnics Committee (HREC) of Central Queensland University (Approval number: 2020 094).
Informed consent was obtained from all the study participants.
Most of the data collected in this study are presented in this paper. However, additional data if required, will be shared up on a reasonable request to the corresponding author.
The authors declare no conflict of interest.
This research received no external funding.
SW, GP and LR conceptualize and conducted the study; GP contributed to data processing and statistical analysis; SW and GP prepared the first draft. UNY, SI, LR provided constructive input finalizing the manuscript. All authors read and approved the final manuscript.