The purpose of this paper is to examine the relationship between measured clinical outcomes and Adverse Childhood Experience (ACE) survey scores in a regional population of children and adolescents admitted to psychiatric services.
ACE survey data collected between 2016 and 2020 was linked with demographic, clinical profile, clinical system variables (eg, repeated admissions), and outcome data for those admitted for treatment. Improved and deteriorated categories of clinical outcome were defined (dependent variable) and their association with demographic and clinical profile data (independent variables) was examined employing bivariate and multivariable logistic regression analysis.
Higher ACE scores were associated with the deteriorated categories of clinical outcome. Demographic, clinical profile and clinical system variables predicted 38% of the variance of the ACE survey total score. A subset of these variables predicted membership in the deteriorated clinical outcome category. There was a strong linear relationship between ACE survey total scores and sequential admissions to services. Poor outcomes were principally related to the following ACE items: Household substance abuse, Physical abuse, Psychotic symptoms, Significant biological family history of mental illness, Social/friendships/community functioning.
The risk for poor clinical outcomes is measurably associated with higher ACE survey scores. Based on the ability to measure this association, a framework is discussed for exploring the nature of effective therapies that take into account adversity child experiences such as Household substance abuse.
Adverse childhood experiences, Child, Adolescent, Clinical outcome, Mental health service, Psychiatric admission
CAAMHPP: Child and Adolescent Addictions and Mental Health and Psychiatry Program; RAIS: Regional Access and Intake System; SMART: Goals - Specific, Measurable, Attainable, Rewarding, and Timely; ACE: Adverse Childhood Experience; WCWL-CMH-PCS: Western Canada Waitlist Children's Mental Health Priority Criteria Score instrument; MTP: Measureable Treatment Plan; CGAS: Children's Global Assessment Scale; PS: Problem Severity Domain of the Strength/Concern Domain Scale
The purpose of this paper is to examine the relationship of measured clinical outcomes and Adverse Childhood Experience (ACE) survey scores in a regional population of children and adolescents treated in the Child and Adolescent Addictions and Mental Health and Psychiatry Program (CAAMHPP). The results form the basis of future work employing ACEs as an indicator of past trauma in order to lay the groundwork to identify what interventions work best to improve clinical outcomes.
Ideally, interventions are directed at stabilization and recovery. Not every individual will respond in time to intervention with improvement. The trajectory of each individual's case is comprised of unique constituents. Some will improve, some will remain unchanged, and some will get worse with or without treatment. These categories of treatment effect related change are not independent of the clinical context. Recovery is a goal, yet for some individuals given their trajectory, a positive clinical outcome might simply be circumventing deterioration. The Mental Health Commission of Canada thematically defines the basis of recovery-focused treatment in their recently published guidelines:
"Recovery approaches stand on two pillars. First, they recognize that each person is a unique individual with the right to determine his or her own path towards mental health and well-being. Second, they also understand that we all live our lives in complex societies, where many intersecting factors (biological, psychological, social, economic, cultural, and spiritual) have an impact on mental health and well-being [1]."
Recovery-oriented mental health services have become a focus of development and reform for several nations including Canada [1]. The recent provincial implementation of Alberta Health Services SMART goals (Specific, Measurable, Attainable, Rewarding, and Timely) aligns with recovery-oriented mental health services in respect to patient participation in goal planning and execution [2]. Recovery-oriented services consist of services wherein consumers actively participate in selecting services and developing treatment plans in the process of recovery [2-5]. Recovery-oriented mental health services are both a philosophy, and evidence-informed approach to practice that requires staff orientation in addition to orientation of patients and their families [3].
Evidence suggests that recovery-oriented mental health services are more effective and efficient than foregoing traditional psychiatric medical models [6]. One key to success is related to the measurement of the processes and effects of program implementation [7,8]. Those who reported receiving higher levels of recovery-oriented services also reported better recovery outcomes. Specifically three domains of recovery-oriented services (i.e., life goal vs. symptom management, individually tailored, and diversity of treatment options) are associated with better overall recovery, and three specific aspects of recovery, namely willingness to ask for help, success orientated goals, and reliance on others [9].
The regional accountability framework developed over the last two decades is presently trauma-informed since 2016, and maps onto the provincial standards of SMART goals and the national standards of recovery-focused treatment, primarily being individually tailored with the long-term embedded ability to build in personal goals and identified strengths (resilience). The present state of the accountability system forms the basis to identify those who do not improve or get worse in treatment in relation to trauma-information – the ACE survey.
Trauma informed, focused and competent clinical practice has been at the forefront of research for over two decades, yet little if any research has tied the progress to clinical outcomes in addiction and mental health treatment (see Table 1 for an overview of a literature search strategy). This is a necessary step in order to more precisely identify what interventions work for what forms of traumatic experience. This is especially the case given the absence of relationship between psychiatric disorders and ACE survey items in a large sample analysis, with the exception of substance use disorder [10]. The present work may be the first wherein ACEs and clinical outcomes are examined in a large clinical sample. In this paper, we examined the relationship between adverse childhood experiences and clinical outcomes. The main hypothesis tested was that those with poor clinical outcomes had higher ACE survey scores.
Table 1: PubMed title search for the terms trauma-informed, focused, competent and competency. View Table 1
The CAAMHPP formed as an integrated regional service division in Calgary, Alberta late in 2001. In early 2002, a centralized intake service was formed to guide a wide range of referral sources and help served families navigate to appropriate services [11]. Facilitating this process, the regional access and intake system (RAIS) was designed and implemented in service of accountability to register and track referred children and adolescents admitted for treatment. Clinical screening and measurement of treatment outcomes was embedded. Screening employed the Western Canada Waitlist Children's Mental Health Priority Criteria Score instrument [12,13] (WCWL-CMH-PCS) and took place primarily at the level of central intake. Clinical outcome measurement occurred at the clinical treatment location on admission and discharge, and took the form of the measureable treatment plan (MTP) which consists of a function domain (Children's Global Assessment Scale: CGAS) and a strength/concern domain labelled as problem severity (PS). In this paper, as the measurement of modulating strengths (strength domain) of as an index of resilience has to date only been marginally employed at baseline measurement in 0.44% of eligible (admitted) registrations [14]. This measurement system has been described [13,14], including its ability to measure the effect of education focusing on the management of child and adolescent mental health cases in primary care [15]. CAAMHPP developed a valid and reliable evidence base permitting a sustainable accountability model employed to evaluate a range of system innovations.
Based on the transformative and evolving program of research emerging from the Adverse Childhood Experience Study [16] (ACE), the local Palix foundation initiated a series of provincial symposia including one focusing on ‘Early Brain Development' (2009-2012) and second titled ‘Accelerating Innovation' (2014-2015). Supported by the Frameworks Institute, these symposia had the mission of accelerating translation of research into practice. Palix's earlier work (Mental Health Showcase) from 2002 to 2007 culminated in a 2007 keynote address on the ACE study by Dr. Vince Felitti that facilitated subsequent local confirmatory research [17-19]. ultimately, the Accelerating Innovation symposium inoculated the senior CAAMHPP leadership with an understanding of the centrality of Adverse Childhood Experiences to life-span health and mental health. Hence in 2016, in conjunction with training, the Adverse Childhood Experience Survey was embedded within the RAIS and formally implemented region-wide. The results have been formidable. While there is a palpable relationship between ACE survey score and clinical severity on admission [20], there is little, if any, relationship between the ACE items and discharge psychiatric diagnosis in complex multivariable analysis [10]. These two findings point to the need to fundamentally change the pedagogical and practice approaches to assessment and treatment, especially given the movement over the last decade toward trauma-informed, -competent, and -focused treatment, foci largely that flow from wide dissemination of the ACE study results. While the ACE survey provides trauma-related information relevant to clinical intervention, the transformation towards proficient trauma-competent and trauma-focused treatment has only just begun. For example, a PubMed search indicates the level of progress in the field (Table 1). While not exhaustive, the results to date with the most work indicate the trend for trauma-information rather than a focus on trauma-competent or trauma-focused research. Trauma-focused and -competent clinical practice will depend on the measured relationship of specific interventions and clinical outcomes within a range of clinical contexts and settings.
The sample consisted of children and adolescents admitted and discharged between November 2016 and May 2020 from regional CAAMHPP services, having at least one completed ACE survey.
These data were linked with Western Canada Waitlist Children's Mental Health Priority Criteria Scores (WCWL-CMH-PCS) and completed measurable treatment plans (MTPs). Demographic variables included age, low risk sex (males) and high risk sex (female, self-defined), low risk family composition (Biological parents and blended families with one step-parent), and high risk family composition (single parent, blood relative, foster parent, adoptive parent or government ward). System variables included repeat admissions, service level (emergent vs. scheduled) and overall length of stay (LOS - final discharge - index admission), described below.
The original ACE survey consists of ten categorical binary items that sum for a total score (value 10) representing the degree of lifetime adversity experienced by the individual across non-ordinal categories [21]. ACEs do not decrease over time. Where children and adolescents had repeated admissions (episodic care model), ACE survey scores were linked to the index admission and last discharge for each client (n = 56667; 58% female, 40% male, 2% self-defined sex/gender).
The use of WCWL-CMH-PCS was implemented in 2002 as a screening instrument that helped place accepted referrals on clinic waiting lists as a function of urgency and severity, rather than the traditional queuing method of first-come-first-served [12]. In addition to clinical utility prioritizing referrals, the WCWL-CMH-PCS is useful in evaluating the clinical quality of referrals to CAAMHPP services, and evaluating clinical outcomes and program effect as a covariate of analysis [11,13,15]. The WCWL-CMH-PCS consists of 17 importance-weighted items, summing to the value of 100 with higher scores indicating greater urgency and severity. The WCWL-CMH-PCS is generally completed by clinically trained intake staff on the index admission to CAAMHPP services, and is not repeated for transfers between services within CAAMHPP.
As employed in this study, the measurable treatment plan (MTP) instrument consists of independent domains. One domain measures global function on admission and discharge employing the Children's Global Assessment Scale (CGAS), which ranges from values of 1-100 based on ten overall categories of function, with lower scores indicting greater functional impairment [22]. The second domain represented on a 20 point scale, with the 0-10 range measuring symptoms, problems, and/or clinical concerns on admission, and respective change on discharge, with lower scores indicating greater problem or symptom. The 11-20 range of the scale permits the measurement of positive adaptations, strengths or resiliencies identified on admission (or over the course of treatment). As noted, the strength domain has not been employed consistently, as clinical treatment has traditionally been concerned with ameliorating symptoms, problems, and clinical concerns, hence is the modulating effect of the strength domain on clinical outcomes is not considered in this analysis. The MTP contains a strength domain, measureable on admission, represents an index of resilience having the potential clinical utility to introduce staff to re-focus models of care on the concepts of recovery- and resilience-oriented treatment.
ACE total scores do not decrease with time and the ten ACE items are binary (0 absent; 1 present). Psychiatric urgency and severity, function, and symptoms do wax and wane over time (WCWL-CMH-PCS total score and 17 weighted scaled items). Based on the CAAMHPP episodic model of care, patients are admitted, transferred between service levels (eg, emergency, inpatient, specialized, and community services), and discharged. Patients may be readmitted subsequently, if required. On average clients are admitted and discharged thrice at different times, often discharged from inpatient or emergency treatment and subsequently transferred to specialized or general community ambulatory care as part of case management. With this naturalistic flow in mind, the length of stay represented in the present analysis is the difference between the index admission and the last discharge of record. The clients' outcome trajectories [13,14] over the course of treatment were derived from the function scale (item #5 within WCWL-CMH-PCS form, generally completed on index referral by intake staff, and the baseline MTP function scale on admission by the primary care provider post-assessment, who usually completes the discharge MTP scales. The measureable treatment plan (MTP) formed the basis of measuring clinical outcome (dependent variable). The clinical function (CGAS) and problem severity (PS) ratings could increase (+), decrease (-), or remain the same (0) over the overall course of treatment.
From the cross-tabulation of the comparison of the three MTP change categories, nine outcome categories arose[(final value at outcome, the final discharge of record) minus the value on admission at baseline (index admission)], with change within each domain being greater than the value zero, equal to zero, or less than zero (Table 2). From these nine outcome categories, two final outcome categories were describe to simplify analysis with the value zero (0) representing MTP improvement (3 gray cells in Table 2) and the value one (1) representing ‘deterioration' (six remaining cells in Table 2) where the change was negative in both or one MTP scale, or there was no change in both scales. This two outcome category construction reduce the chances of rejecting the null hypothesis, given the cells with one positive and one negative MTP change value, and formed basis of the analyzed data structure.
Table 2: MTP change categories. View Table 2
The first the sample demographics were described followed by a description of ACE total score distribution across the nine possible MTP outcomes within the improved and deteriorated outcome categories (Table 2; shaded). This was followed by a binary logistic regression analysis of the outcome and each independent, demographic (age, high/low risk sex), and system (eg, LOS, referral reasons, service level) variables (Table 3). Examination of binary outcomes is important in terms of examining the underpinning data structure when compared to multivariable results for the same variables and those included in final reduced models [15]. Multiple linear regression of the relationship of the Ace total score to all variables simultaneously, including the improved/deteriorated outcome (Table 4). This was followed by a stepwise (forward and backward) multivariable logistic regression analysis that identified the most important variables related to the binary the improved/deteriorated outcome (Table 5). Figure 1 shows a best fit graphic illustrating the relationship of the ACE total score and length of stay (LOS). The analysis was conducted employing Stata 15.
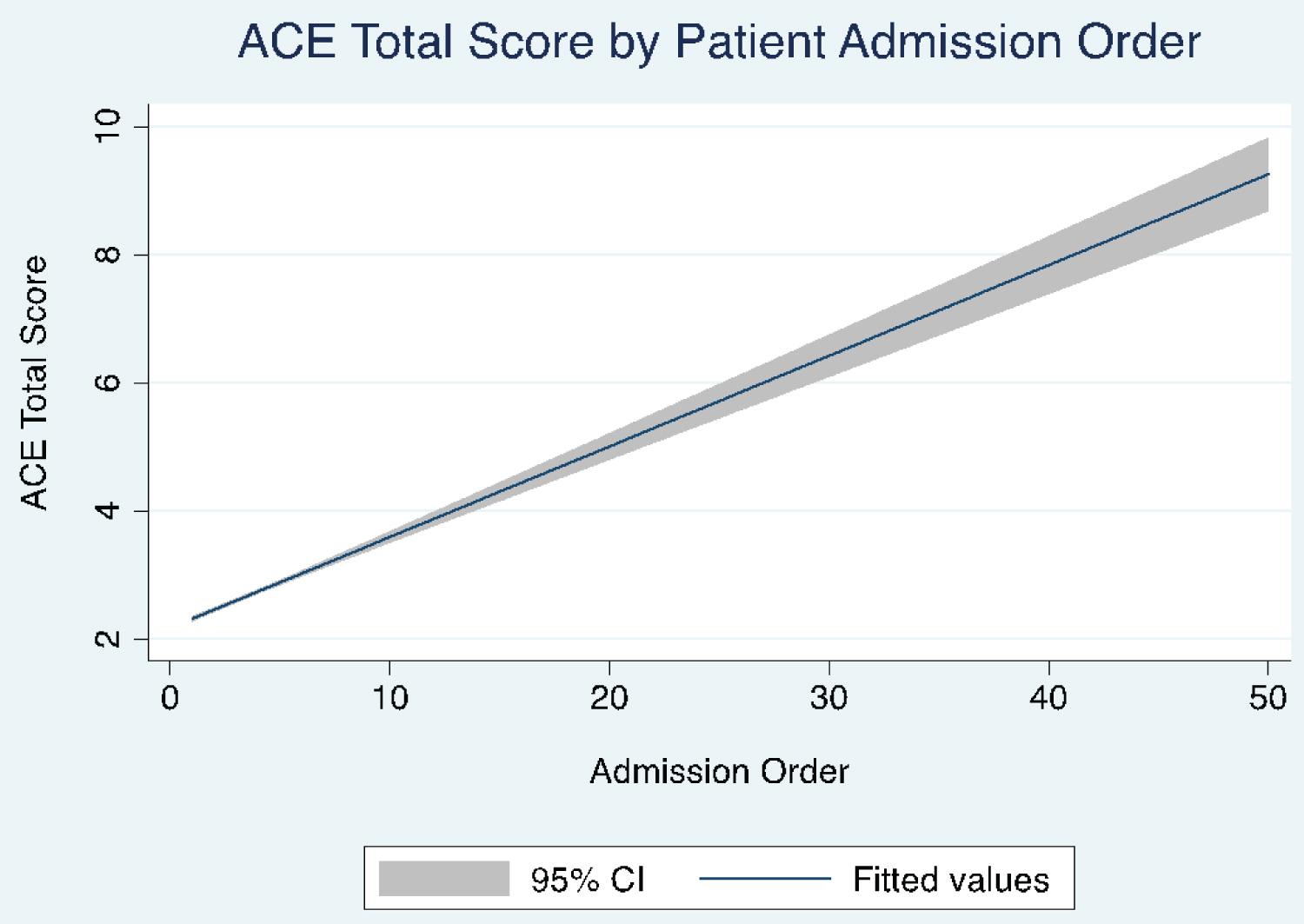 Figure 1: Linear fit of ACE total scores and sequential patient admissions to regional child mental services.
View Figure 1
Figure 1: Linear fit of ACE total scores and sequential patient admissions to regional child mental services.
View Figure 1
Table 3: Bivariate description of independent variables. View Table 3
Table 4: The linear regression analysis summary showing the associations of all other independent variables and the ACE total score. View Table 4
Table 5: Logistic regression result summary of the most important independent variables representing improvement (odds ration < 1.0) or deterioration (odds ratio > 1.0) at outcome (dependent variable). View Table 5
Males (mean age 11.57; Std. Dev. 4.42) had of the lowest median ACE total scores (mean 2.89; median 2; Std. Dev 2.65), whereas higher ACE total scores (mean 3.42; median 3; Std. Dev. 2.7) were observed for females (mean age 13.7; Std. Dev. 3.7) and self-defined sex (mean age 14.63; Std. Dev. 2.63) had the highest ACE total scores (mean 4.2; median 4; Std. Dev 2.64).
Table 2 shows the cell size (n) mean, median, standard deviation (Std. Dev.) of ACE total score for the nine MTP (CGAS/PS) change groups. The shaded cells contain three improvement groups (value 0) and the remainder contains the deterioration group (+1) with the associated changes in both the CGAS and problem severity (PS) score domains on discharge. These three improvement groups formed the base group (value 0) in the following bivariate summary and multivariable logistic regression analyses. The remaining 6 groups represent change in CGAS or problem severity scores on discharge, where there was no change (0) or decrease (-1) in one of the domains, even with an increase in the other group (+1). On this basis, the outcome groups of the sample were reduced, along with providing a bias against finding a positive result. For example, including the marginal groups served two purposes when one category decreased (deteriorated) even though the other MTP domain improved (CGAS or Problem Severity): 1) Reducing the chances of finding significant differences in the analyses, and 2) Increasing the sample sizes in each of the two outcome comparison groups. Both purposes served to improve the reliability of the analyses.
Table 3 shows that the ACE total score distinguished the outcome groups in logistic bivariate comparison. Similarly, 11 of the 17 WCWL-CMH-PCS items and the WCWL-CMH-PCS total score distinguished the outcome groups in logistic bivariate comparison with WCWL items #4 and #17 reducing the likelihood of membership in the deteriorated group. The increases in age, membership in high risk sex (female or self-defined) and family composition (single parent, blood relative, ward ship or custody, or adoption), as well as system variables including length of stay (marginally), number of admissions after referral, and presentation to emergency services, all increased the likelihood of membership in the deteriorated group.
In Table 4, with the exceptions of WCWL items #3, #7, #9, #12, and #14, all other independent variables had a significant association accounting for 38% of the variance in the ACE total score.
Multivariable logistic regression results (Table 5) summarize of the association of the most important independent variables and the binary outcome groups (dependent variable). Positive values of the odds ratios represent a significantly increased probability of membership in the group with an absence of improvement at outcome (defined here as deterioration), whereas values significantly below the value one, represent a significantly decreased probability of membership in the group with an absence of improvement (eg, deterioration) at outcome (defined here as improvement).
Table 5 represented the most parsimonious model containing the significant independent variables accounting for the likelihood of membership in the deteriorated outcome group, as compared to the improved group (base of comparison) given by the odds ratios. Of note, ACE items #5-Emotional neglect and #9-Parental separation or divorce, as well as membership in the high risk sex grouping, WCWL item #17-Degree of likely benefit with further intervention, referral reasons school/learning/attention problems, and lower likelihood of emergency services, reduced the odds of membership in the deteriorated outcome group (eg, odds ratio less than the value one). The remainder increased the odds of membership in the deteriorated outcome group (eg, odds ratio greater than the value one). These ACE items included #1-Physical abuse, #3-Psychotic symptoms, #7-Household substance abuse, #11-Significant biological family history of mental illness, #13-Social/friendships/community functioning.
Figure 1 is provided to illustrate one of the most salient burdens of care related to higher ACE scores, independent of clinical variables and complex analysis. It shows the strong positive linear relationship between ACE total scores and order of admissions for individuals grouped by their sequence of admissions.
Having an established regional access and intake system (RAIS) that gathers case-specific referral, admission, and discharge information [11] pertinent to ACEs, along with information pertaining to the assessment of clinical urgency, symptom profile, and global function data, has permitted the examination of the relationship of ACEs and two categories of clinical outcome on discharge. This body of information about those seeking treatment in the catchment area has confirmed the hypothesis that higher ACE scores are associated with poor outcomes.
Nevertheless, many more patients with high ACE scores improve than deteriorate. Each of the 9 possible outcomes shown in Table 2 has a distribution of ACE scores. The independent variables account for about 38% of the ACE total score, and, while substantial for psychosocial measurement, 62% of the variance remains unaccounted for. Although, some degree of this variance resides in measurement error of the instrumentation, it is likely other unidentified sources of variance remain. For instance, the effects of time alone, individual differences among clinicians (training, personal history, motivation), differences in clinical processes and settings (clinical atmosphere, environment milieu, office, group, mandatory vs. voluntary treatment, virtual vs. face-to-face) are important factors that may contribute to the unaccounted variance. Patients interact with all aspects of the aforementioned and bring to bear on their own outcomes similar if not categorically identical sets of developmental, constitutional, and epigenetic individual differences, familial, and social influences.
Recent local community initiatives focusing on resilience have become popular, along with dissemination of national recovery-focused models of care [1]. Focusing on strengths at the outset of the clinical relationship is cornerstone to such initiatives. One observation from the present study is that the regional system of child mental health care measurement framework incorporates a strengths measure on admission, but this measure has not been implemented to the extent where it can be employed in analysis. This is perhaps indicative of a system of care that is largely problem-focused rather than patient-focused. While there are longstanding models locating disorder in the relational space brought into the clinical setting [23-27], CAAMHPP primarily focuses on a psychiatry-based, biopsychosocial model of treatment that does not take into account the past trauma of the patient when it comes to assessment and prescribing treatment [10]. The treated problem (or diagnosis) within this standard of care presently resides in the patient.
Identifying strengths and existing positive adaptations at the point of clinical intake employing the existing measurement framework is a straightforward approach to integrating a strength assessment. In other words, orienting staff to use the existing strength-based measure may, without undue stress, may help them in the task of identifying resilience. This could be accomplished will minimal training of staff that is already practicing in an already burdened system of care [11]. Formalizing measurement of the resilience or strength domain of the MTP scale would advance the model of care and expand the capacity to account for a greater portion of the unexplained variance within the existing measurement framework and assess the effect of this important measurement domain on treatment outcomes.
Measuring types of therapeutic intervention represent another potentially measureable source of the unexplained variance that is critical to systems of care seeking to become trauma-competent and trauma-focused. Simple, yet comprehensive approaches [28] can easily be integrated into the existing accountability system with minimal difficulty. In fact, the MTP has been generalized to the point that it may be implemented to measure the effect of any treatment or intervention for any disorder at the level of individual or groups of patients employing a randomized controlled trial format to which takes into account, both life events and comorbidities. It may even be employed in focused clinical training [29] similar to how the MTP has been employed [15]. This approach not only expands the field of measurement, but fundamentally changes the clinical educational assessment paradigm by bringing objective skills and clinical examination into the everyday field of practice [29]. Implementation of more detailed and standardized identification of the types of clinical interventions may permit identification of interventions presently associated with clinical outcomes. This creates the clinical space that may be directed at possible improvement of the outcomes for those admitted with high ACE survey scores, who are at risk for poor clinical outcomes, and thereby, identify what works best for these patients. However, this standardized, measurable method based on the Hawaii Blue Menua of assessing the current types of clinical intervention employed by clinicians [28] has not yet been linked to clinical outcomes. When measured independently, the report indicated that a minority of clinicians employed evidence-based interventions when analyzed by disorder and age, whereas most employed eclectic approaches and the minority endorsed age-, diagnosis-appropriate and evidence-based approaches (eg, CBT) [28]. Eclectic approaches tended to those learned during training then employed ubiquitously in practice. Individuals reporting the use of an eclectic approach to treating child and adolescent mental health problems tended to have less knowledge of the current evidence-based treatments of what was embedded in the survey. A minority of staff (~30%) reported varying evidence-based clinical approaches by therapeutic context (e.g., family, group, individual), patient age, and diagnosis [28].
ahttps://www.practicewise.com/Community/BlueMenuIt is the exception that this study has focused on the parameters related to poor clinical outcome. There is a range of factors underlying poor clinical outcomes. Factors may reside not only in the individuals' case histories, as indicated by the ACE survey scores associated with poor outcome, but also in the relation to the WCWL-CMH-PCS scale items. The present results do not include any definition of the therapeutic type, context, milieu, or quality in relation to age or diagnosis [28]. While the accountability system is presently trauma-informed [10,11], and is possessed of the ability to measure the effect of community-level professional training on the frequency and quality of referrals from primary care [5] to date, there has not been a concerted effort to quantity the type, context, milieu, or quality of therapy with linkage to clinical outcomes.
Limitations included the following. There were sign differences comparing the bivariate and multivariate likelihood of membership for some of the variables (Table 4 and Table 5). The reasons for this may be associated with collinearity and low sample sizes within strata, such as in the reasons for referral variable remaining in the model. These two reasons are less possible explanations for the other variables, as there were much larger sample sizes in the outcome cells for each variable. The sign reversal differences for these variables in the multivariable model may be due to latent variables not examined in this study; thus, there is a need to develop more complex models (eg, Structural Equation Models) to explain potential underlying relationships is recommended.
Additional limitations to note are related to patient trajectory in treatment. For example, it is unknown whether or not treatment prevented those who deteriorated or remained the same on discharge (Table 1) from further deterioration. Similarly, while unlikely, treatment may have impaired achievement of higher levels of improvement based on the passage of time alone. The MTP reliability study provided evidence suggesting, treatment had an effect on functional outcomes independent of time when waitlist controls were used to measure baseline trajectory [14].
A minority of children admitted to child and adolescent mental health services with high ACE scores do poorly as indicated by the clinical variables measured on discharge. A multi-method approach is required to elucidate the factors accounting for those who do poorly in treatment compared to those who well compared. Understanding the qualitative differences underpinning membership in either group may improve the delivery of trauma informed, competent and focused services.
Risk for poor clinical outcomes is measurably associated with higher ACE survey scores. The ability to measure this association provides a framework for exploring in more detail the nature of effective therapies in relation to the quality, context, and milieu within the range of interventions provided by clinicians, in addition to the influences of social determinants, social environment, and other family factors.
Finding a standardized method for defining the types and context of clinical interventions, as well as measuring strengths on admission, are a logical next steps toward becoming recovery-focused (resilience) and trauma-competent (what works) on the path to providing an effective trauma-focused standard of care provided by way of treatment. A standardized definition of therapy and its context is required to advance toward evidence-based trauma-competence in service provision [28]. The baseline information from this study helps somewhat to better define details related to the types of clinical profiles associated with the risk of poor clinical outcomes and illustrates the burden of care related to those with high ACE survey scores.
Each category of outcome described in this paper has a distribution of ACE survey scores. The majority of patients with higher ACE scores do better as indicated by the measured clinical variables on discharge (Table 1). Exploring matched cases with both poor and improved outcomes in qualitative detail, including the clinical context of each case by interviewing clinicians, patients and families, may help to identify and isolate factors that differentiate the two outcome groups. Disseminating such the findings by way of undergraduate, continuing, and professional development, education models may help clinicians improve their clinical approach to high-risk cases.
Finally, the strong linear relationship between ACE total score and service utilization (Figure 1) provides strong evidence to support the need to reshape [11] the present service delivery models to incorporate ACE survey and item data at the point of assessment and prescription of treatment consideration of within current psychiatric standards of care [10].
Conceptualization: Sandra Cheung, David Cawthorpe; Formal analysis: David Cawthorpe; Methodology: Sandra Cheung, David Cawthorpe; Validation: David Cawthorpe; Writing-original draft: Sandra Cheung, David Cawthorpe; Writing-review & editing: Sandra Cheung, David Cawthorpe.
Study conducted under Ethics ID: REB15-1057.
No conflicts of interest to declare.
Unfunded.