Kaposi's disease (KD) is a multifocal, vascular lesion of low-grade malignant potential that presents most frequently in mucocutaneous sites. KD also commonly involves lymph nodes and visceral organs.
This case intend to describe multifocal atypical kaposian manifestations in HIV negative patient.
Kaposi, Herpesvirus 8, Human, HIV Infections, Homosexuality
Kaposi's disease (KD) is a multifocal angiogenic process characterized by a double vascular and cellular proliferation, often multicentric, that is associated with human herpesvirus 8 (HHV-8) infection. Four recognised clinical subtypes can be distinguished [1]. Visceral manifestations, particularly lymph nodes, are frequent in AIDS-associated KD [2]. They are rarer in the classical forms.
We report the observation of a classical form of KD, atypical by its multifocal character and its rapid and destructive evolution, without any known immunodepression factor.
A 70-year-old patient presented to our department with a 2-year history of a painful tumor of the left foot. There were no pulmonary or gastrointestinal symptoms. There was no history of any systemic disease or use of immunosuppressive drugs except he has been on insulin for diabete.
Clinical examination showed a multi-nodular ulcerating tumor (Figure 1) associated with homolateral lymphedema of the left foot. The lymph node examination revealed bilateral axillary and inguinal adenopathies with a large adenopathy in the left popliteal fossa. There were no oral mucosal lesions.
 Figure 1: A multi-nodular ulcerating tumor of the left foot.
View Figure 1
Figure 1: A multi-nodular ulcerating tumor of the left foot.
View Figure 1
The histological study showed a tumor proliferation of atypical epithelioid cells with a spindle-shaped aspect in the dermis (Figure 2). The immunohistochemical study noted the expression of CD 34 and HHV8 (Figure 3). HIV serology was negative. The diagnosis of Kaposi's disease in its classical form was retained.
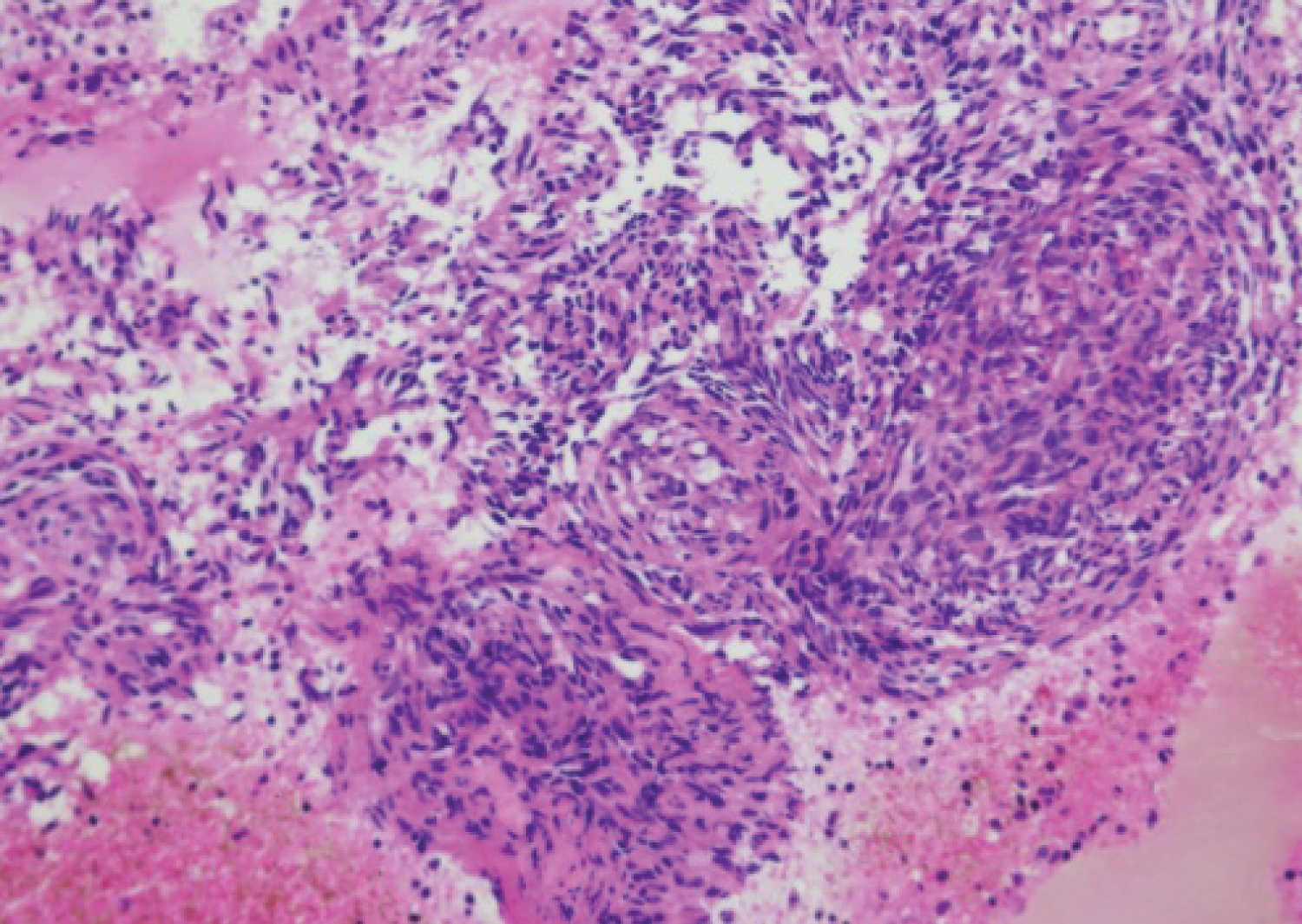 Figure 2: Histo-pathological evaluation revealed proliferation of spindle-shaped cells with cytological atypia (Hematoxylin, original magnification x 200).
View Figure 2
Figure 2: Histo-pathological evaluation revealed proliferation of spindle-shaped cells with cytological atypia (Hematoxylin, original magnification x 200).
View Figure 2
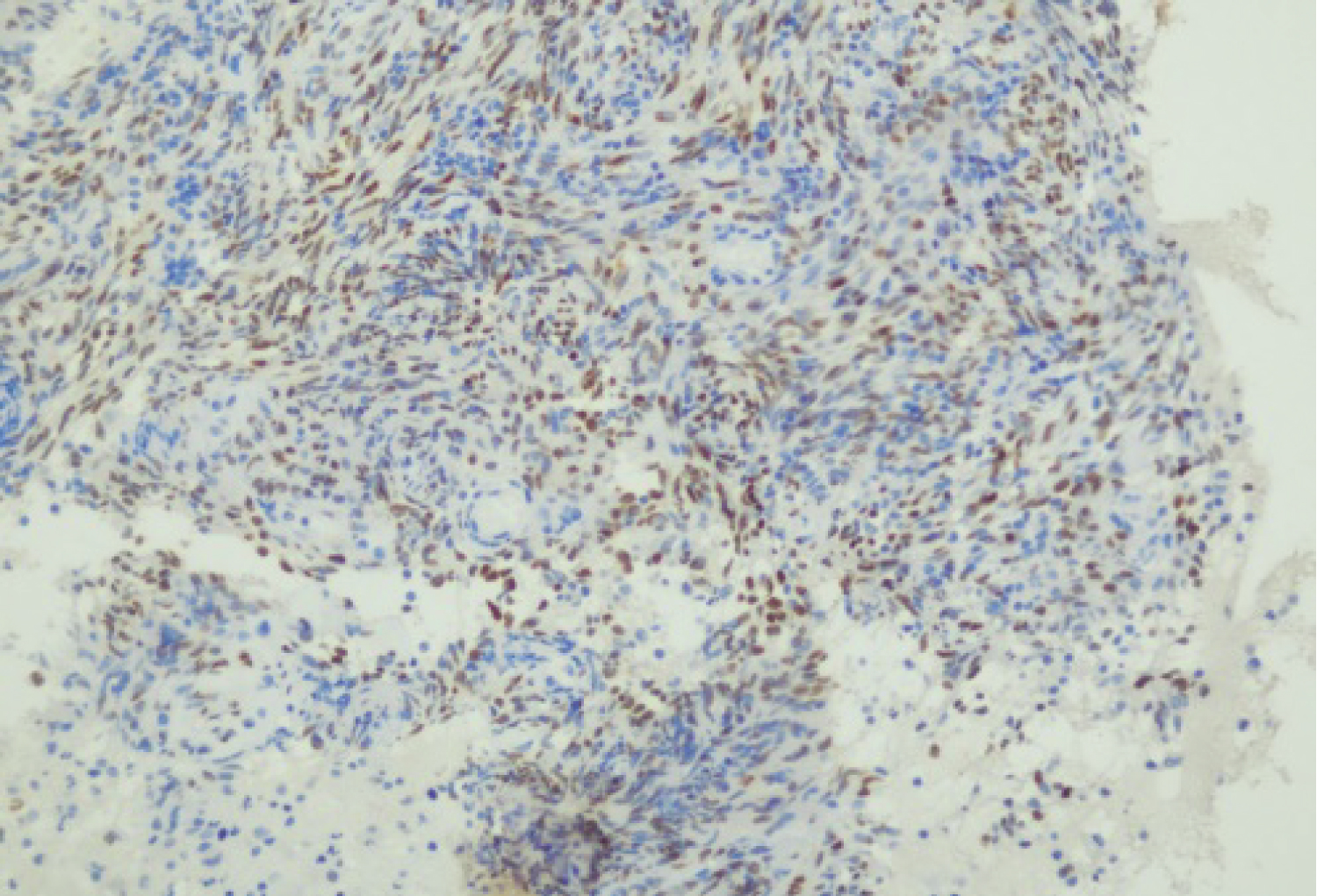 Figure 3: Immunohistochemical staining for human herpesvirus 8 in a biopsy specimen taken from the lesion (haematoxylin and eosin stain, Original magnification x 200).
View Figure 3
Figure 3: Immunohistochemical staining for human herpesvirus 8 in a biopsy specimen taken from the lesion (haematoxylin and eosin stain, Original magnification x 200).
View Figure 3
The X-ray of the foot showed a total lysis of the fifth metatarsal. Abdominal echography and thoracoabdominal CT scan demonstrated lesions highly suggestive of hepatic and pulmonary involvement, and inguinal lymph node whose biopsy concluded to a lymph node localization of his Kaposi's disease. Digestive endoscopic exploration was normal.
The patient was classified Classical disseminated Kaposi's sarcoma with multivisceral involvement, chemotherapy was initiated.
Kaposi's disease is a multifocal low-grade vascular neoplasm witch cutaneous and visceral expression associated with HHV-8 infection. There are 4 subtypes with different epidemiologcal and clinical manifestation and prognosis; wich include a) Classic KD occurs primarily among men, usually over the age of 50 years, who are of Mediterranean and Jewish origin. The site most commonly affected is the skin of the lower extremities. Internal organ involvement is rare, b) African-endemic KD affects patients across a broad range of ages, including children, young adults, and elderly people. Male patients predominate. The severity of the disease also varies. Typically, young children have a more severe course of disease, affecting both the lymphatic system and internal organs rather than the skin, c) Iatrogenic, immunosuppressive, drug-associated KD affects immunocompromised individuals such as transplant recipients, those on steroids and other cytotoxic drugs, it often progresses rapidly and often affects internal organs, lymph nodes, and the face. Patients taking immunosuppressive therapy frequently have full regression of the Kaposi's lesions when the therapy is terminated, d) HIV-associated KD with extensive cutaneous and mucosal forms, lymph node and visceral involvement and can rapidly lead to death [3-5].
Recently a new categorie of KD has been discribed among HIV-negative homosexuel men it has only been reported sporadically, but most cases fulfill the same characteristics: Patients around 50 years of age, with a Classic clinical presentation of Kaposi's disease, limited to the skin and associated with a good prognosis. No immunodeficiencies are presented with normal humoral and cellular immunity [6,7].
Visceral involvement in HIV-negative patients with classical Kaposi's disease (KD) has been described only rarely and is particularly seen during the advanced stages of the disease. The nodular form of the disease is characterised by locally aggressive lesions which may appear as fungating, exophytic, ulcerating growths or as a diffuse infiltrative process involving large areas of skin and subcutaneous tissue, with bone involvement [8].
Biopsy is mandatory for diagnosis. Histopathologically, there is no difference between these subtypes Plaque-stage KS lesions are characterised by the proliferation of spindle-cells throughout the whole dermis and sometimes the subcutis. The most important immunohistochemical labelling is that of the causal virus, HHV-8, which is currently found in all forms of KD [9].
Treatment of KD depends on the setting, the extent, the course and the subtype; forms with Localised, asymptomatic lesions, therapeutic abstention and monitoring can be proposed. Aggressive forms characterised by lymph node and/or visceral involvement, severe oedema, local complications or rapid extension require systemic treatment with a preference for vinblastine or bleomycin. Taxanes may be indicated in the presence of mucosal involvement and in edematous forms; in extensive and/or visceral forms, chemotherapy may be proposed [10].
In this case, our patient had a very "aggressive" clinical presentation, rapidly evolving, with normal immune function and in the absence of HIV infection indicating the interest to carry out further explorations even in the absence of clinical symptoms.
The authors declare no conflicts of interests.