Background: Long-term hemodialysis treatment of chronic kidney disease (CKD) can lead to disorder of calcium and phosphorus regulation and abnormal parathyroid function. Most patients with renal failure often have secondary hyperparathyroidism, at which time the parathyroid glands can release large amounts of parathyroid hormone (PTH), which activate osteoclast activity to increase serum calcium levels, resulting in severe skeletal diseases, including osteoporosis, pathological fractures, bone pain.
Case presentation: We report a case of a 62-year-old woman with bilateral femoral neck pathological fractures who was diagnosed with tertiary hyperparathyroidism and severe osteoporosis due to long-term hemodialysis treatment for renal failure. On the 1st day after bilateral total hip arthroplasty (THA), sudden seizure resulted in periprosthetic fractures and acetabular loosening. After the patient's condition stabilized, bilateral revision total hip arthroplasty was performed respectively. There are no similar reports in the previous literature.
Conclusions: Perioperative anti-osteoporotic therapy and close monitoring of serum calcium levels are beneficial in long-term hemodialysis patients with hip fractures. At the same time, more attention should be paid to refractures caused by severe osteoporosis and hypocalcemic seizure after THA.
Total hip arthroplasty, Kidney failure, Tertiary hyperparathyroidism, Osteoporosis, Periprosthetic fracture, Hypocalcemic seizure
The global prevalence of chronic kidney disease is estimated at 11%-13% [1], and end-stage renal disease (ESRD) accounts for 6.8% of all health expenditures [2]. With the improvement of medical level and treatment methods, the survival rate of patients with CKD continues to improve, but the incidence of disease-related complications is also increasing.
At present, hemodialysis is often used for chronic renal failure in the country and abroad to remove metabolites that cannot be excreted from the body and maintain homeostasis. According to reports in the literature, long-term dialysis treatment can stimulate the parathyroid glands to a certain extent, leading to parathyroid dysfunction and increasing the probability of parathyroid adenoma [3]. Long-term disturbance of PTH levels can lead to an imbalance of calcium and phosphorus regulation in the body, which largely contributes to the occurrence of bone-related diseases and hypocalcemic epilepsy [4].
However, early hyperparathyroidism does not have a significant effect on the human body. As the disease progresses, PTH increases serum calcium levels through direct action on bone and the kidneys, resulting in multiple organ system complications, including osteoporosis, pathological fractures, bone pain, skin itching, urinary stones, gastrointestinal discomfort, asthenia.
Pathological fractures of bilateral femoral necks due to endocrine system diseases are uncommon, and cases of bilateral periprosthetic fractures and acetabular cup loosening due to hypocalcemic seizure after THA are even rarer.
A 62-year-old woman was diagnosed with CKD stage 5 two years ago due to abnormally elevated creatinine levels and was treated with twice-weekly hemodialysis. The increase of PTH was found 3 months ago, which was diagnosed as tertiary hyperparathyroidism with severe osteoporosis. She was admitted to hospital 10 days ago with bilateral hip pain and joint mobility disorder without apparent trauma.
After admission, the patient received hemodialysis and symptomatic treatment, and completed the related preoperative examination. The results of hip X-ray and SPECT/CT indicated: bilateral femoral neck fracture (Figure 1), parathyroid adenoma, severe osteoporosis, and bilateral renal atrophy. In laboratory findings, hemoglobin was 77 g/dL (normal 115-150 g/dL), albumin 32.1 g/L (normal 35-55g/L), creatinine 559.8 umol/L (normal 41-81 umol/), alkaline phosphatase 624.4 U/L (normal 50-135U/), urea 24.34 mmol/L (normal 3.1-8.8 mmol/L), serum phosphorus 1.91 mmol/L (normal 0.85-1.51 mmol/L), PTH 352.0 pg/ml (normal 15-65 pg/ml). Serum levels of sodium, potassium, calcium and chloride were all normal.
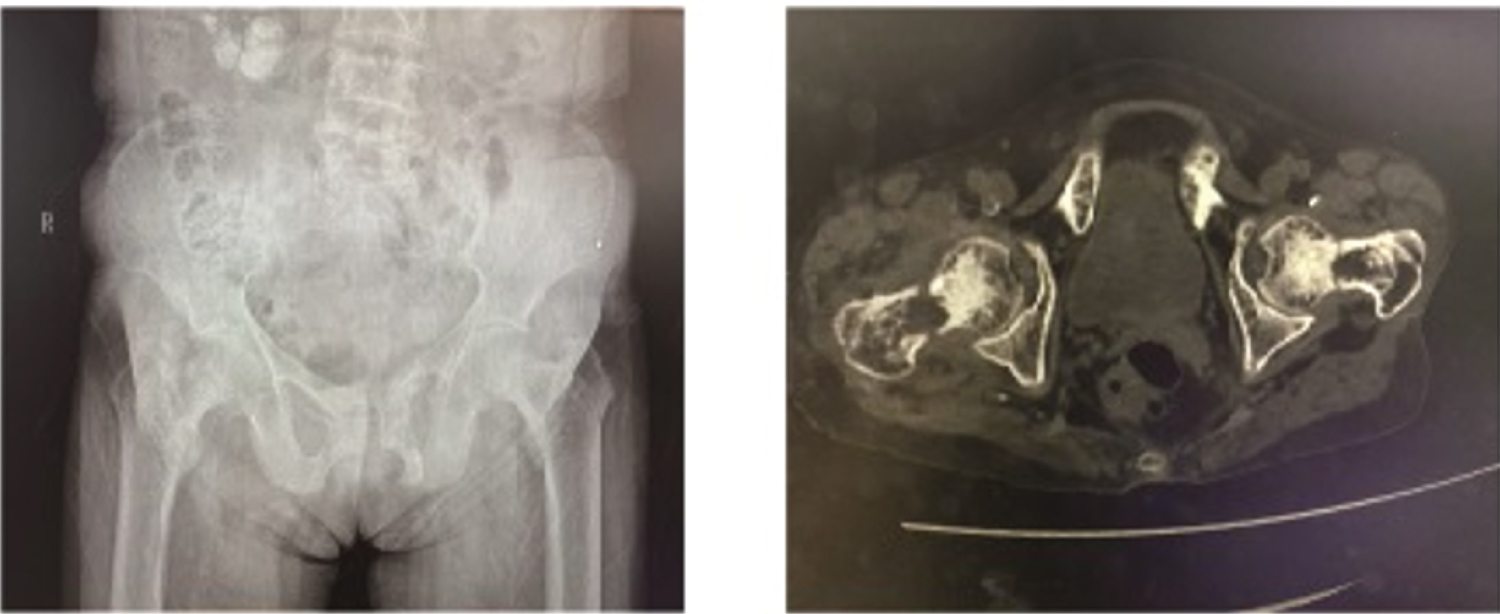 Figure 1: Preoperative pelvic imaging showing bilateral femoral fractures.
View Figure 1
Figure 1: Preoperative pelvic imaging showing bilateral femoral fractures.
View Figure 1
Bilateral THA was performed through posterolateral approach under general anesthesia after the condition was stabilized. The Intraoperative fluoroscopic images are shown in Figure 2. The intraoperative blood loss was about 500 ml, and 2U of leukocyte-removed suspended red blood cells were infused. The vital signs were stable, the patient was brought back to the ward safely. On the first postoperative morning, the patient became unconscious and went into convulsive seizures. Considering that hypocalcemia caused epileptic seizures, the patient was in critical condition and was later transferred to the intensive care unit (ICU) for treatment.
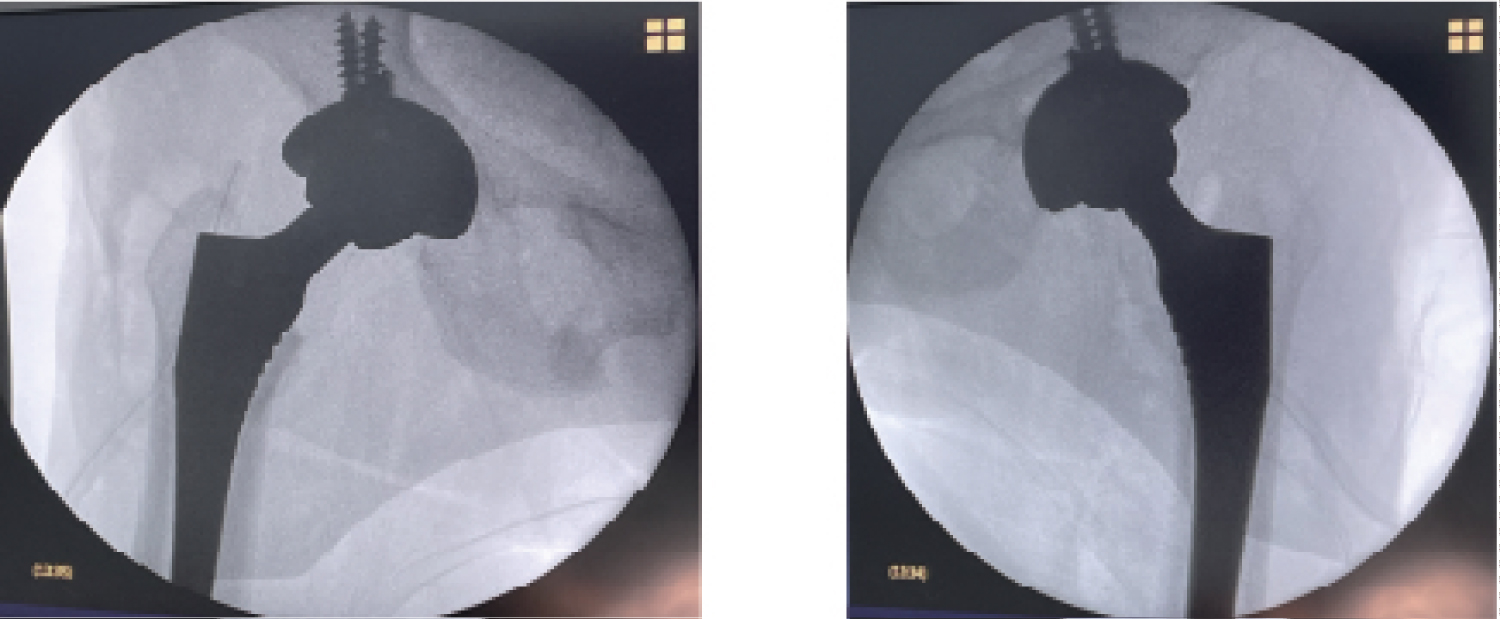 Figure 2: Intraoperative fluoroscopic images of bilateral total hip arthroplasty.
View Figure 2
Figure 2: Intraoperative fluoroscopic images of bilateral total hip arthroplasty.
View Figure 2
After 4 days of ICU treatment, the patient was transferred to the general ward, and the X-ray of the hip showed: bilateral periprosthetic hip fractures, left hip dislocation, and right acetabular cup loosening (Figure 3). Anti-osteoporosis therapy with vitamin D and calcium during the period of hospitalization. On the 14th postoperative day, the left femur fracture was fixed with steel wire and the femoral cement stem was replaced under epidural anesthesia (Figure 4A). One week later, right revision total hip arthroplasty, acetabular reconstruction, and greater trochanter fixation were performed (Figure 4B). The patient was discharged successfully after 46 days of hospitalization in orthopedics department.
 Figure 3: Antero-posterior view of the pelvis: periprosthetic fractures and acetabular loosening after hypocalcemic seizure.
View Figure 3
Figure 3: Antero-posterior view of the pelvis: periprosthetic fractures and acetabular loosening after hypocalcemic seizure.
View Figure 3
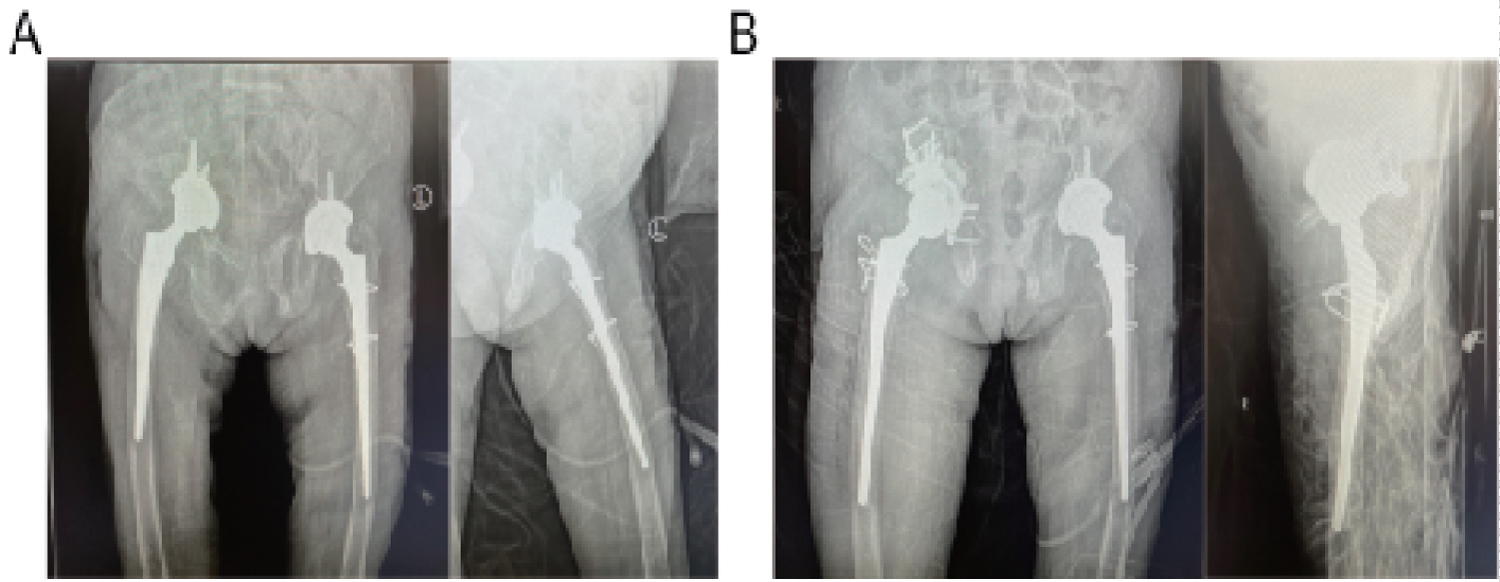 Figure 4: Postoperative radiography of the pelvis after bilateral revision total hip arthroplasty (A) left side; (B) right side.
View Figure 4
Figure 4: Postoperative radiography of the pelvis after bilateral revision total hip arthroplasty (A) left side; (B) right side.
View Figure 4
The kidney is a multifunctional organ which serves primarily to rid the body of metabolic wastes and to form hormones. Renal osteodystrophy (ROD), a bone remodeling disorder, is a rare complication associated with several alterations in mineral metabolism present in patients with CKD. Low circulating calcium (Ca2+) concentration will stimulate the parathyroid gland to secrete PTH, coupled with the reduction of its inactivation by the kidneys, the level of PTH in patients with renal failure is significantly higher than that in normal people.
Studies on early chronic kidney disease show that most patients have hyperparathyroidism when they reach CKD stage 3, and nearly 90% of them have hyperparathyroidism at the beginning of dialysis treatment [5,6]. Hyperparathyroidism mainly upregulates the expression of RANKL, thereby activating osteoclasts to cause severe cortical bone destruction and large decrease in bone mineral density [7]. Steven Fishbane, et al. showed significant associations between PTH, serum calcium levels and hip fracture in dialysis patients [8]. The risk of hip fracture in patients with ESRD was 4.4 times greater than the general population [9].
Medical treatment for hyperparathyroidism consists of supplying vitamin D receptor activator and reducing phosphate intake, but surgical removal may be required in severe cases [10,11]. Previous literature reported that surgical management of secondary hyperparathyroidism showed good efficacy [12], and surgery also significantly reduced the risk of fractures in the elderly [13]. In addition, Amila Silva, et al. reported 3 successful cases demonstrating that it is safe and effective to perform total parathyroidectomy and bipolar hemiarthroplasty at the same setting [14]. But such cases are very rare, there is currently no uniform standard for whether such patients should undergo parathyroidectomy at the same time.
Studies have shown that people with epilepsy are twice as likely to sustain a fracture as people without epilepsy [15], and most of the fractures of the skull, clavicle and nasal bones are caused by direct trauma, but a few humeral fractures are caused by the muscular tension of the seizure itself [16]. There are also case reports of bilateral femoral neck fractures in children due to hypocalcaemia-induced seizure caused by vitamin D deficiency [17]. The mean arterial calcium ion concentration of patients within 3 days after surgery was 0.89 ± 0.46 mmol/L (normal 1.15-1.35 mmol/L), and preoperative hemodialysis treatment and surgical stress may induce hypocalcemic seizure. Because the patient had severe osteoporosis, involuntary muscle twitching resulted in refracture and prosthesis loosening.
Surgical treatment for femoral neck fracture includes closed reduction-internal fixation with cannulated screw and THA. A systematic review showed that renal dialysis patients can expect good functional outcomes after total hip arthroplasty compared with non-dialysis patients [18], but in periprosthetic Joint Infection (7%), dislocation (7.6%), revision and 90-day mortality risk is higher [19]. The one-year pooled mortality for periprosthetic femoral fractures after hip arthroplasty in the last decade was 13.4% [20]. With the aim of avoiding from secondary surgery, Bilgehan Tosun, et al. suggested that initial treatment of hemiarthroplasty might be the most suitable way of intervention for dialysis patients [9].
For long-term hemodialysis patients with hip fractures, perioperative anti-osteoporotic treatment, monitoring of PTH level and serum calcium concentration is necessary. Surgeon needs to fully evaluate the patient's bone mass and select an appropriate surgical plan, and more importantly, be alert to refracture caused by hypocalcemic seizures. But the optimal timing of parathyroidectomy in hip fracture patients with secondary hyperparathyroidism or parathyroid adenoma requires further research.
National Natural Science Foundation of China, Grant/Award Number: 82160173. Natural Science Foundation of Jiangxi Province, Grant/Award Number: 20212BAB216019, 20171BAB205033.
Weihua Li and Zehui Zou are responsible for the compilation and writing of the paper, and are regarded as co-first authors for equal contributions.