In haemodynamically stable patients with blunt splenic injuries, non-operative management (NOM) including the use of selective splenic artery embolization have been shown to be an effective treatment option [1]. Proximal splenic arterial embolization reduces bleeding by decreasing pulse pressure to the spleen, hence lowering intra-splenic arterial blood pressure and promoting thrombosis of injures vessels [2]. Splenic tissue perfusion is still achieved through a collateral arterial network, deriving from the short gastric arteries and left gastroepiploic artery [3]. Splenic abscess is a known complication of splenic injury and has been reported to occur in up to 4.3% of patients after embolization and NOM [4].
In this report, we present a rare case of delayed splenic abscess formation with upper pole necrosis following proximal splenic artery embolization in a patient with impaired splenic collateral blood supply, having previously undergone sleeve gastrectomy surgery for weight loss. Consent was obtained from the patient for the writing of this case report.
A 31-year-old female patient initially presented to the trauma centre after falling off a horse, sustaining a AAST (American Association for the Surgery of Trauma) grade IV splenic injury including lacerations in the middle of upper aspects of the spleen extending to the hilum without evidence of active bleeding. The patient's medical history was remarkable for a laparoscopic sleeve gastrectomy three months prior to the accident with a resultant 35 kg weight loss and a current BMI of 26.3 kg/m2, previously 35 kg/m2. The patient proceeded to a proximal splenic artery embolization using pushable coils within four hours of the time of injury and had an uneventful recovery on the ward. All recommended vaccinations were administered as per the Australian Spleen Registry guidelines, and she was discharged home after five days without clinical concern. Prophylactic antibiotics were not required in accordance with these guidelines. There was an absence of Howell-Jolly bodies on the peripheral blood film performed four weeks after the procedure, indicating normal splenic function [5].
Fourteen weeks later (98 days), the patient re-presented with five days' history of sharp left flank pain radiating to the left shoulder and back. In the emergency department, she was febrile at 38.1 °C and tachycardic at 105 beats per minute. Inflammatory markers were elevated with white cell count (WCC) of 14.7 × 109/L and C-Reactive Protein (CRP) of 190 mg/L. Repeat computerised tomography scan revealed a large area of devascularised splenic tissue with a peripherally enhancing collection measuring 4 cm and surrounding fat stranding, in keeping with a splenic abscess (Figure 1). There were also reactive changes in the liver adjacent to the abscess.
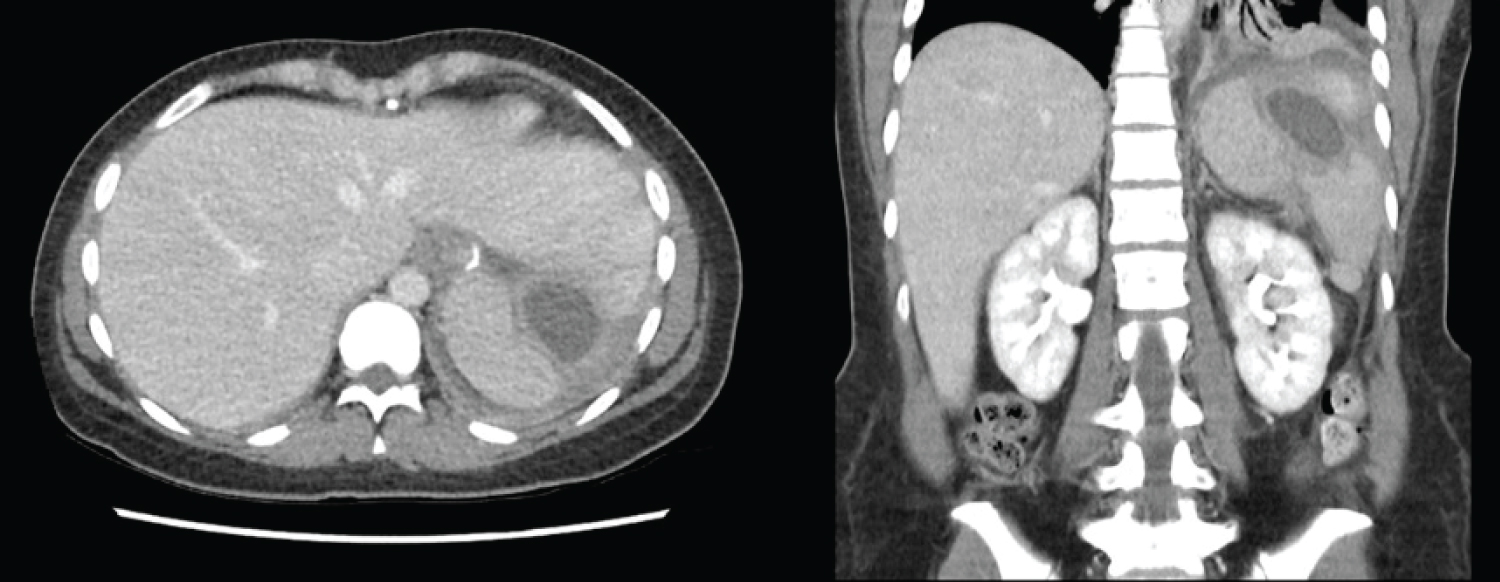 Figure 1: Axial (left) and coronal (right) portal venous phase CT abdomen-pelvis showing the splenic abscess.
View Figure 1
Figure 1: Axial (left) and coronal (right) portal venous phase CT abdomen-pelvis showing the splenic abscess.
View Figure 1
Intravenous antibiotics were administered with azithromycin, ceftriaxone and metronidazole. With compromised splenic blood supply due to embolization and the absence of short gastric vessels, the decision was made to proceed to open splenectomy. Intra-operatively, there was no generalised contamination. The spleen was found in two segments with a central abscess cavity. The upper segment was necrotic, the lower segment appeared healthy, but removal was required to facilitate access to the upper segment. There were dense adhesions of the superior infected segment to segment II of the liver and lateral diaphragm. After splenectomy, thorough washout with normal saline was undertaken, and a drain was left in the left upper quadrant.
The intra-operative fluid and tissue was sent to microbiology for microscopy, culture and sensitivity analysis. The initial gram stain identified gram-positive cocci and gram-positive rods, but the final culture of the intra-operative sample yielded no growth, possibly due to the preoperative administration of antibiotics. All blood cultures were negative. Post-operatively, patient was switched to piperacillin-tazobactam and vancomycin, based on the results of the initial gram stain. Drain-tube amylase was sent on day 3 post op and was found to be low. The drain was subsequently removed on day 5.
The patient also developed bilateral pleural effusions post-operatively with near complete collapse of left lower lobe, resulting in persistent tachypnoea and tachycardia on the ward. Given her symptoms, the left pleural effusion required drainage on day 2 post op. Serous fluid only was drained, and the effusion was likely reactive.
Antibiotic regime was de-escalated to oral amoxicillin-clavulanic acid after 7 days of intravenous antibiotics. Due to a transient increase of inflammatory markers without a clear source of infection, a repeat CT abdomen pelvis was performed on day 13 post op. Imaging revealed a subdiaphragmatic collection, however targeted ultrasound imaging showed that it was more consistent with a post-splenectomy haematoma and was not amenable to radiological drainage.
The patient was discharged home on day 16 post op with two weeks of oral antibiotics and followed up with general surgery as well as the infectious disease outpatient clinics. Patient remained well at two weeks and then at two months follow-up, with an abdominal ultrasound demonstrating a decrease in size of the haematoma.
Splenic injury is the most common intra-abdominal injury following blunt abdominal trauma [6]. In haemodynamically stable patients with blunt splenic injury, (NOM) has become the standard of care as it is cost-effective and has been shown to preserve long-term splenic immune function [7,8]. In intermediate to high-grade splenic injuries (Grade III-V), embolization has been shown to increase the success rates of NOM [9]. On the other hand, surgical management is often indicated in the presence of haemodynamic instability and peritonitis due to concomitant visceral injury [10]. Predictors for failure of NOM include bleeding disorders, grade V injury and blood transfusion requirement [11].
There are two main approaches to splenic arterial embolization. In cases of focal splenic injuries, selective distal arterial embolization may be performed to prevent bleeding from a specific branch of the splenic artery. In more severe and multi-focal injuries, proximal embolization is utilised to decrease the perfusion pressure in the spleen but still allow tissue viability through collateral pathways [3]. Both techniques have an equivalent rate of major complications requiring secondary splenectomy; however distal embolization carries a higher risk of minor complications not requiring splenectomy due to the rate of infarction distal to the site of embolization [12]. In a recent study, it was shown that there is no significant difference in splenic immunological function between the two approaches and that long-term immune function can also be preserved in this cohort [8,13].
Potential complications post-embolization includes bleeding, infarction, abscess formation, pleural effusions and coil migration [14]. Amongst these, splenic abscess has been reported to occur in up to 4.3% of patients who underwent embolization, most required a splenectomy with the exception of one reported case which was treated with one month of intravenous antibiotics [4].
An important collateral blood supply to the spleen after embolization to prevent infarction and the formation of abscess is the collection of short gastric vessels. They are 2-10 terminal arteries arising from the distal or sometimes the upper polar branch of the splenic artery. They supply the fundus of the stomach along the greater curvature and form anastomoses with the left gastric artery, a branch of the coeliac trunk [3]. In sleeve gastrectomy surgery, the short gastric vessels are often ligated during the mobilisation of the gastric fundus. This has been observed to lead to insufficient perfusion of the upper pole of the spleen, which is asymptomatic in the majority of cases but may occasionally lead to splenic infarct and abscess [15]. While the gastroepiploic artery remains viable for collateral blood supply in patients after sleeve gastrectomy, in this case it proved to be insufficient to allow appropriate flow for aseptic healing to occur.
Currently there is a lack of literature to support a treatment algorithm for patients with high-grade splenic injuries after gastric surgery. On many occasions, this history is not available at the time of injury if the patient is unconscious, or the type of surgery is not known, and the diagnosis is made on CT. Given the size of the left gastroepiploic artery, and the positive attributes associated with the use of splenic salvage techniques, it is reasonable that we should continue to offer NOM adjuncts such as embolization in these patients. However, it may be prudent to observe these patients more closely in both the inpatient and outpatient settings, where the dual collateral supply has been reduced to a single supply. This is a direction that future research should take given the current obesity epidemic and use of durable surgical techniques for weight loss [16].
In conclusion, we present a case report of a patient with delayed failure of NOM of splenic trauma in the setting of proximal embolization and previous sleeve gastrectomy. This case highlights the role of the short gastric vessels as one of two collateral blood supplies to the spleen. Although definitive data is not available in the literature on this unique subset of patients, the sleeve gastrectomy in this case may have contributed and patients with previous gastric surgery should be more closely observed after embolization due to a potentially higher risk of failure of NOM.
- Splenic injuries are common in abdominal trauma.
- Non-operative managements including arterial embolization are preferred in haemodynamically stable patients.
- The short gastric vessels are important collateral supply to the upper pole of the spleen.
- In patients with impaired splenic collateral blood supply, risk of splenic abscess formation is increased post-embolization.
- Patients with previous gastric surgery should be more closely observed after embolization for risk of failure of NOM.