Ischemic stroke is a rare neurological complication following SriLankan Russell's viper envenomation. We report a case of a 44-year-old person, who developed multiple cerebral and cerebellar infarctions following SriLankan Russell's viper envenomation. The patient developed both local and systemic envenomation and was treated with Snake Venom Anti-Serum I.P. (VinsBioproducts Ltd). On day six, this patient developed left-sided hemiparesis. CT scan of the brain showed bilateral cerebellar, bilateral occipital, and right-sideparietal lobe infarctions.
Cerebral infarctions, Cerebellar infarctions, Russell's viper, Snake bite
There are about 37,000 admissions to Sri Lankan hospitals following snake bites every year [1]. The Sri Lankan Russell's viper is responsible for 30-40% of these cases. Severe envenomation and case fatalities due to Russell's viper bites are higher compared to other snake bites in Sri Lanka. These viper bites usually occur in paddy (rice) fields and on footpaths at dusk and dawn. It affects agriculture workers and considered to be an occupational hazard in Sri Lanka [1]. Envenomation causes local swelling, coagulopathy, acute kidney injury, neuromuscular paralysis characterized by ophthalmoplegia and ptosis, and rarely respiratory muscle paralysis [1]. Rhabdomyolysis, chronic renal failure, myocardial infarction, and secondary hypopituitarism [1] have also been reported following Russell's viper envenomation.
Anuradhapura is an ancient city in the north-central province of Sri Lanka and is home to around 860,575 people (census 2012). Majorities are farmers and at risk of snakebite. We report a case of a 44-year-old previously healthy farmer from Anuradhapura presenting to the emergency department 90 minutes following a snake bite. Dead snake was identified by the medical officer at the emergency department as Russell's viper (Daboia Russelii -Thith Polanga). There was moderate pain and swelling at the bite site and fang marks were clearly seen on the right foot. Two hours after admission patient developed irritability, vomiting, blurred vision, ptosis, ophthalmoplegia, and, difficulty in breathing with inspiratory stridor & difficulty in swallowing. His GCS was 15/15; pupils were 3 mm in size and reacting equally bilaterally. The pulse rate was 80/min, and the blood pressure was 120/80 mmHg. His oxygen saturation was 100%, and the lungs were clear. He was treated with anti-venom serum (AVS) 20 vials. Six hours after completion of AVS, his whole blood clotting time (WBCT 20) was still prolonged (> 20 minutes) and clotting time was 12 minutes, INR was 2.06; APTT was 56 second (control 44 Sec). Ten vials of AVS were repeated uneventfully. On day two, the patient developed respiratory distress with worsening inspiratory stridor and the patient was intubated and admitted to ICU. During intubation, severe laryngeal edema and bleeding were noted. During the ICU stay, he developed acute kidney injury with a raised serum creatinine of 193 μmol/dl, which recovered gradually during the next few days. Throughout his blood pressure remained stable and no cardiac arrhythmias noted. His 2D-echocardiogram was normal. On day six, it was noted that he had developed left-sided hemiparesis. Non-contrast CT of the brain was done and showed right parietal, bilateral occipital and bilateral cerebellar infarctions (Figure 1a, Figure 1b and Figure 1c) with early obstructive hydrocephalus and cerebral edema. No hemorrhages or midline shift was seen. The neurosurgical team suggested an urgent decompressive craniotomy. Unfortunately, the patient passed away before the procedure.
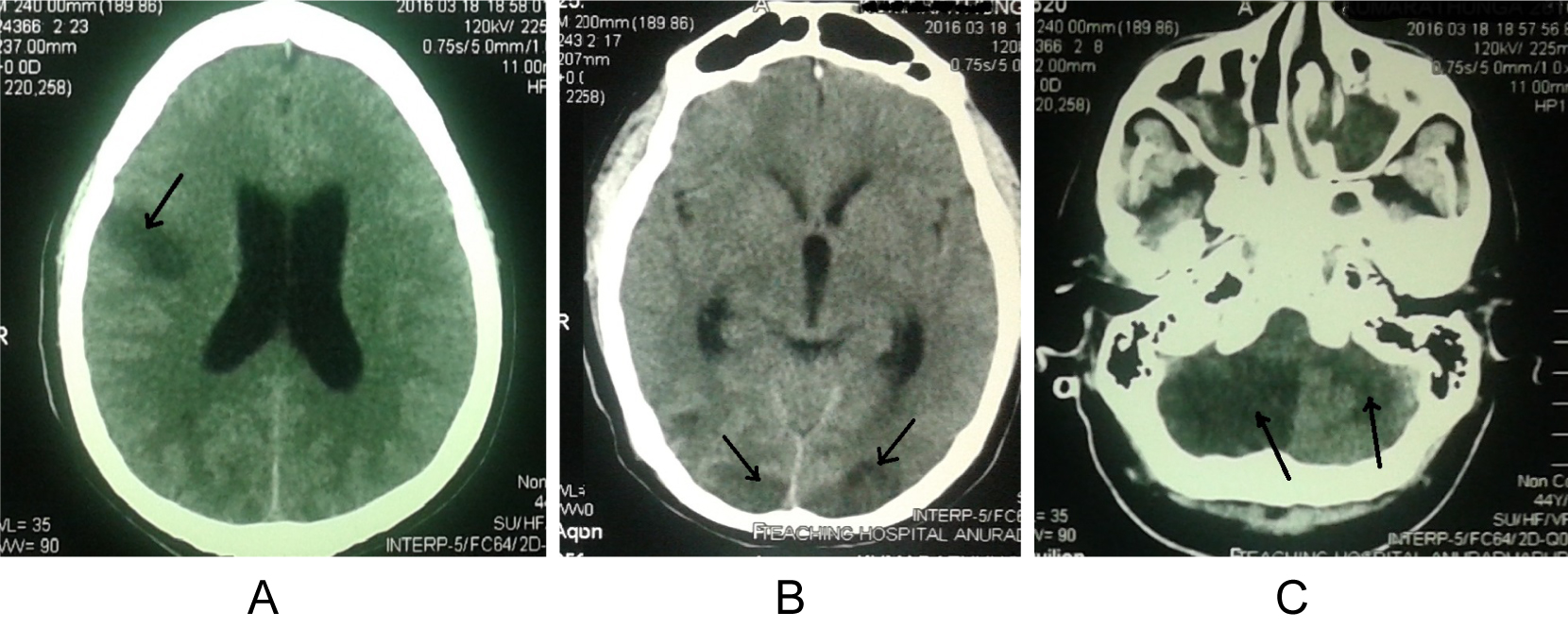 Figure 1: Non-enhanced CT brain scan of the patient with infarctions (arrows), involving both anterior and posterior circulation territories. a) Right parietal lobe; b) Bilateral occipital lobes; c) Bilateral cerebellar hemispheres. View Figure 1
Figure 1: Non-enhanced CT brain scan of the patient with infarctions (arrows), involving both anterior and posterior circulation territories. a) Right parietal lobe; b) Bilateral occipital lobes; c) Bilateral cerebellar hemispheres. View Figure 1
Although cerebral infarctions were reported following Russell's viper envenomation, infarctions involving both anterior and posterior circulation are rarely reported. Most reported cases had anterior circulation strokes. The following are the few reported cases of ischemic strokes following Russell's viper bite, found in the Sir Lankan literature (Table 1). Russell's viper venom-associated thrombosis involving the heart and limbs is a well-recognized phenomenon [3,6].
Table 1: Previously published cases of ischemic strokes following Russell's viper bites in Sri Lanka. View Table 1
The following mechanisms have been proposed as the cause for thrombosis resulting in ischemic cerebral infarction after Russell's viper envenomation. Toxins such as hemorrhagins of snake venom cause vessel wall damage and severe vascular spasm and microthrombi formation [7,8]. The toxins with well-established pro-coagulant and platelet aggregating properties like cerastobin [9], factor IVa [10], cerastocytin [11,12], cerastotin [13] and afaacytin [14], causes thrombus formation. Arginine, esterase, and hydrolases in venom also have procoagulant properties [8]. These various protein products have thrombin-like enzyme activity; each toxin activates different pathways of the coagulation cascade. Their activities are inhibited by monoclonal antibodies against GP1b or GPIIb/IIIa or thrombin receptor. Endothelial damage, toxin-induced vasculitis [6,15] and, increased vascular permeability may contribute to vascular occlusion leading to thrombosis. Micro-thrombi formation as a sequel to the low-grade disseminated intravascular coagulopathy and hypotension are also leading causes for ischemia and infarction.
Venom induced consumption coagulopathy (VICC) happens following Russell's viper envenomation. It includes a broad range of factor deficiencies depending on the procoagulant toxin in the venom, which used to cause bleeding [16].
Better outcomes have been reported with immediate AVS treatment. A large number of studies have demonstrated that antivenom can bind to procoagulant toxins and prevent their effects in vitro if the antivenom and venom are pre-mixed. Antivenom may not be effective in certain situations. The most important being that irreversible toxic effects cannot be reversed by antivenom binding to toxins after the damage has occurred, such as clotting factor deficiencies resulting from VICC. For antivenom to be effective against such irreversible effects, it must be administered early, so it can bind with toxins before they distribute to their target sites and cause irreversible toxicity [15]. But no studies to show the effectiveness of AVS for snakebite-associated thrombotic microangiopathy. The mean time for the onset of stroke symptoms after envenomation seems to be as early as 23.8 ± 10.9 hours in some studies [17]. In our patient onset time was much delayed.
In this patientm ischemic infarctions due to hypotensionis unlikely as he was normotensive and no watershed infarctions seen in CT brain. The possibility of a cardiac source of embolization was excluded. His blood picture did not show any evidence of thrombotic microangiopathy. Therefore, it can be hypothesized that toxin-induced vasculitis, pro-coagulant, and platelet aggregating properties of toxins might have given rise to this complication.
Despite early treatment with AVS, this patient developed cerebral infarctions involving both anterior and posterior circulation territories. This case study illustrates that ischemic cerebral infarctions must be looked in to as a complication related to Russel's viper envenomation. Further research is needed to identify the possible mechanisms of ischemic stroke in the context of snake bites and to develop specific treatment strategies.
No funding was provided for this report.
All authors declare no conflicts of interest.