Conjoined twins are one of the rarest forms of twin pregnancy. The prenatal evaluation of conjoined twins the first trimester is crucial due to the increased risk of perinatal morbidity and mortality.
A Caucasian 31-years-old pregnant woman, referred to our Department at 11 weeks of gestation. At first evaluation, the pelvic ultrasound revealed a monoamniotic-monocorial conjoined twins pregnancy, a single trunk, two heads in close apposition, two necks and two vertebral columns, four upper limbs and four lower limbs were detected. A single apparently normally structured heart was revealed with cardiacactivity. After diagnosis an adequate counselling to the couple was performed, and they opted for termination of pregnancy at 12 weeks of gestation.
A tempestive diagnosis of conjoined twins pregnancy is highly important to lead to the best the rapeutic option. Thoracopagus conjoined twins account for more than 40% of conjoined twins pregnancies, and the prognosis is very poor because in most of cases a single heart and/or liver is present. In our case, the premature diagnosis has given the family a chance to choose for pregnancy termination reducing as far as possible the already heavy emotional impact of that condition.
Conjoined twins are one of the rarest forms of twin pregnancy accounting for 1:50.000 to 1:100.000 live births [1]. Although the pathogenesis of this malformation is not clear, monozygotic twin pregnancies are thought to be caused by the aberrant division of a single zygote (fission theory) after 13-15 days of the embryonic period or, more probably, by the secondary association of two separate mono-ovulator embryonic discs (fusion theory) [2].
Conjoined twins were firstly classified by Spencer [3] and are named according to the most prominent site of fusion. The conjoined site may be in the ventral, dorsal or lateral groups. According to the shared anatomy, the conjoined twins are classified into: Thoracopagus (most frequent), parapagus dicephalus, cephalopagus, omphalopagus, parasitic, craniopagus, parapagus diprosopus, ischiopagus, rachipagus, pygopagus and unspecified (about 21% of cases) [4].
The prenatal evaluation of conjoined twins using ultrasound in the first trimester is very important due to the increased risk of perinatal morbidity and mortality. In the second trimester, ultrasound evaluation and magnetic resonance imaging can improve and clarify the diagnosis by describing detailed anatomy of the two foetuses and the parts shared [5,6].
Prognosis of conjoined twin depends on the body parts shared, it is estimated that up to 60% of cases die in utero, approximately 35% are stillborn or die within the first 24 hours after birth [7]. It is reported to be a sporadic condition with no known associations and approximately 70-75% of cases involves female foetuses [8].
The surgical approach to conjoined twins pregnancy is a complex and multidisciplinary process, thus diagnostic tools are essential to provide the anatomical informations required for performinga surgical division of conjoined twins. Although the most common type is thoracopagus, it is difficult to surgical treat this form because of a shared heart often present [9].
After the diagnosis, an accurate counselling to family is needed to define the possible therapeutic options including termination of pregnancy, selective fetocide and post-partum surgical separation of twins. Here, we present an extremely rare case of thoracopagus conjoined twins with a single heartshared, diagnosed in the first trimester of pregnancy.
A Caucasian 31-years-old pregnant woman, referred to our Department at 11 weeks of gestation for the first trimester screening. This was a spontaneous first pregnancy. The patient was in good general condition, without history of any disease. No history of twin pregnancy in her family has been reported.
At first evaluation, the trans-abdominal pelvic ultrasound revealed a monoamniotic-monocorial conjoined twins pregnancy, with evidence of a single trunk, two heads in close apposition, two necks and two vertebral columns, four upper limbs and four lower limbs. A single apparently normally structured heart was revealed with cardiac activity (Figure 1). The crown-rump length was 47 millimeters. Moreover, both foetuses appeared in costantly fixed position according to each other and a moderate amount of oedema around both twins extending from above the heads to most of the common trunk was detected (Figure 2). A sagittal scan of the thorax and abdomen and a transvaginal ultrasound evaluation confirmed the diagnosis of conjoined thoracopagus twins with spillage of abdominal organs. The Color-Doppler evaluation revealed a reverse flow in the single venousduct. The three-dimensional ultrasound scan added few informations to the previous bi-dimensional exam.
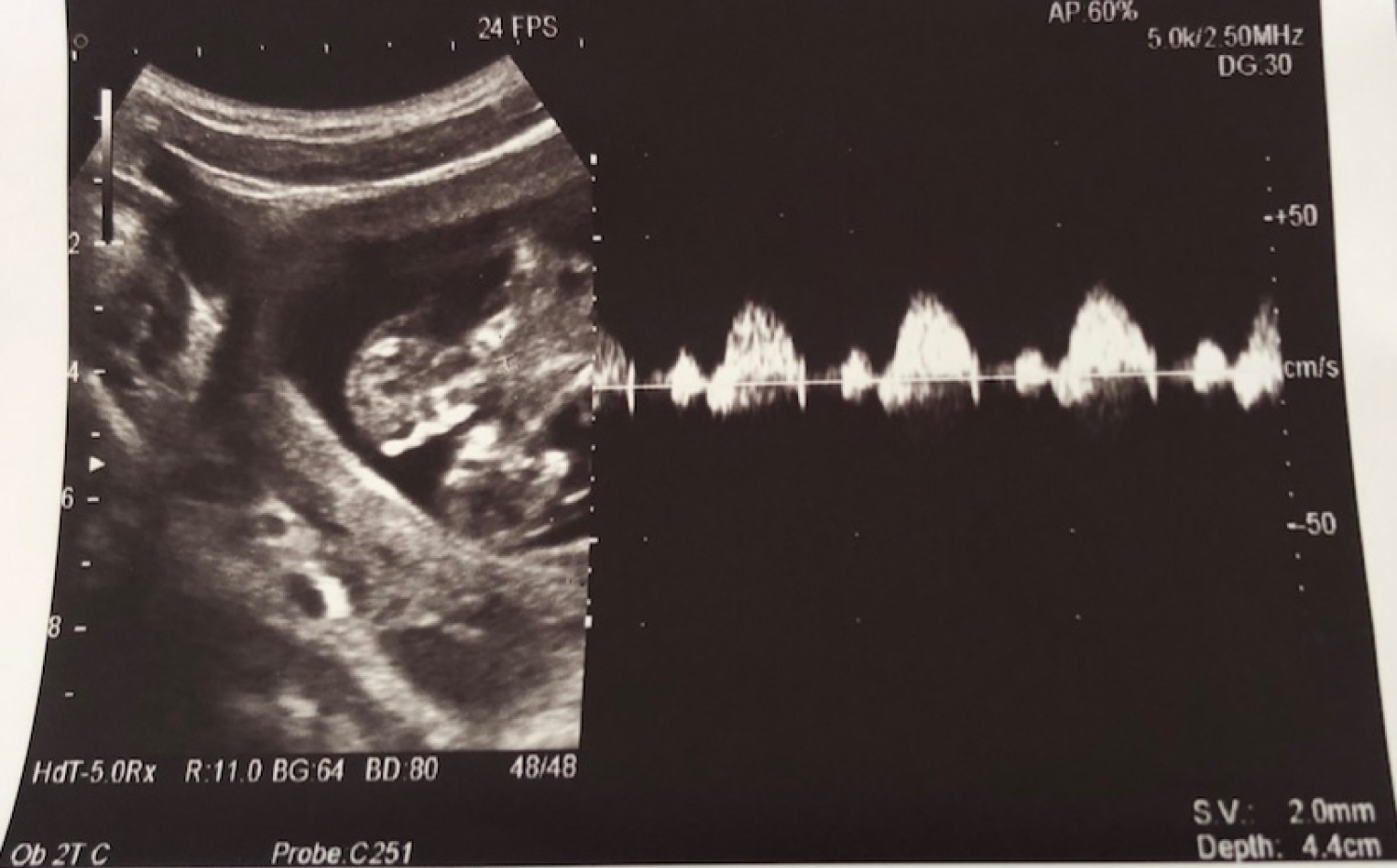 Figure 1: Twins' single hearth activity. View Figure 1
Figure 1: Twins' single hearth activity. View Figure 1
 Figure 2: Sagittal view of the increased nuchal thickness with posterior oedema. View Figure 2
Figure 2: Sagittal view of the increased nuchal thickness with posterior oedema. View Figure 2
After diagnosis, an adequate counselling to the couple was performed by illustrating all the possible options, and they opted for termination of pregnancy at 12 weeks of gestation. The procedure of pregnancy termination was conducted by vaginal prostaglandins administration to the patient after informed signed consent. The expulsion of foetuses occured after the end of one cycle of prostaglandins, with both twins intact (Figure 3). After that, a dilatation and curettage was performed, The procedure was uneventful and the patient was discharged the dayafter. The pathology report confirmed the diagnosis of intact thoracopagus conjoined twins with a single heart, a single gastroenteric system with bowel spilled from the abdomen, an unrecognizable liver, four kidneys and adrenals, four upper limbs, four lower limbs, a single polylobed left lung, a single umbilical cord with three vessels and a single placenta.
 Figure 3: Intact thoracopagus conjoined twins after abortion. View Figure 3
Figure 3: Intact thoracopagus conjoined twins after abortion. View Figure 3
A tempestive diagnosis of conjoined twins pregnacy is crucial for choosing the best therapeutic option in terms of pregnancy termination or gestational continuation with surgical twins separation.
Early pregnancy termination could be defined as a safer option because it implies a less emotional impact for the couple that instead could be exacerbated by the multiple and multidisciplinary follow-up required during prenatal and post-natal period [10].
In our case, we have been able to detect prematurely a monoamniotic-monocorial conjoined twins pregnancy by pelvic and transvaginal ultrasound, thus leading the couple to the widest choice available in this situation. Obviously a premature diagnosis is not always possible, for example in cases of obese mother or if a reduction of amniotic fluidis diagnosed, the ultrasound evaluation could not be enough efficient requiring a pelvic magnetic resonance imaging support. Fortunately, in this case we performed the diagnosis in the first trimester and the couple was able to choose for the termination of pregnancy at 12 weeks. Thoracopagus conjoined twins account for more than 40% of cases [11], and the prognosis of this kind of twins is very poor because in most of cases a single heart and/or liver is present [1]. The ultrasonographic findings in our case were consistent with literature reported diagnostic criteria for thoracopagus conjoined twins with a single heart shared and an unrecognizable liver without the gross anomalies apart from these. A surgical twins separation in our case would have been quite impossible because of the single heart shared, thus the premature diagnosis has given the family a chance to choose for pregnancy termination reducing as far aspossible the already heavy emotional impact of that condition.
No funding was provided for this report.
All authors declare no conflict of interest.
• Doctor Rosica G, Bucari D, Pastore G: Participated to the conception and revision of the work;
• Doctor Musella A, Rosica G: Provided to the acquisition of data and draftof the work;
• Doctor Rosica G, Bucari D, Pastore G: Contributed to the final approval of the version to be published.