Subclinical hyperthyroidism, Atrial fibrillation, Anticoagulation
TSH: Thyroid Stimulating Hormone; EKG: Electrocardiogram; AF: Atrial Fibrillation; EF: Ejection Fraction; RVR: Rapid Ventricular Response; EGD: Esophagogastroduodenoscopy
A 72-year-old Hispanic male with an unconfirmed history of alcohol-related cirrhosis presented to the hospital for rectal bleeding and dark stool for two days. Vitals included a heart rate of 90-120 bpm, blood pressure 90-140 over 50-60 mmHg. A left thyroid nodule was appreciated on physical exam. His pertinent labs included TSH, free T3 and T4 levels that were 0.033 mU/L (low), 3.33 mU/L and 1.33 mU/L (both within normal limits) respectively. A TSH done 3 days later was low (0.024). Thyroid peroxidase antibody and TSH receptor antibody were negative. EKG on admission revealed new-onset atrial fibrillation (AF) with a ventricular response of 99. Neck ultrasound confirmed the physical exam finding of a calcified nodule on left inferior lobe of thyroid corresponding to a cold nodule on radioactive uptake scan (Figure 1). Ultrasound of the abdomen documented coarsened liver echotexture/chronic liver disease with no free fluid. Echocardiogram revealed mild left atrial dilation with normal EF and diastolic dysfunction. Rate control was achieved with a diltiazem bolus during episodes of RVR. Metoprolol was used to treat AF and the adrenergic effects of subclinical hyperthyroidism. Low dose methimazole therapy was considered, though with caution due to his high risk of liver dysfunction. However, the patient ultimately refused. Anticoagulation was delayed due to his increased risk of bleeding (HASBLED - 4). The patient was later discharged with apixaban after an unremarkable EGD and colonoscopy and was advised to follow up for a possible biopsy of a hypoactive thyroid nodule and follow up to evaluate alternative options to treat subclinical hyperthyroidism.
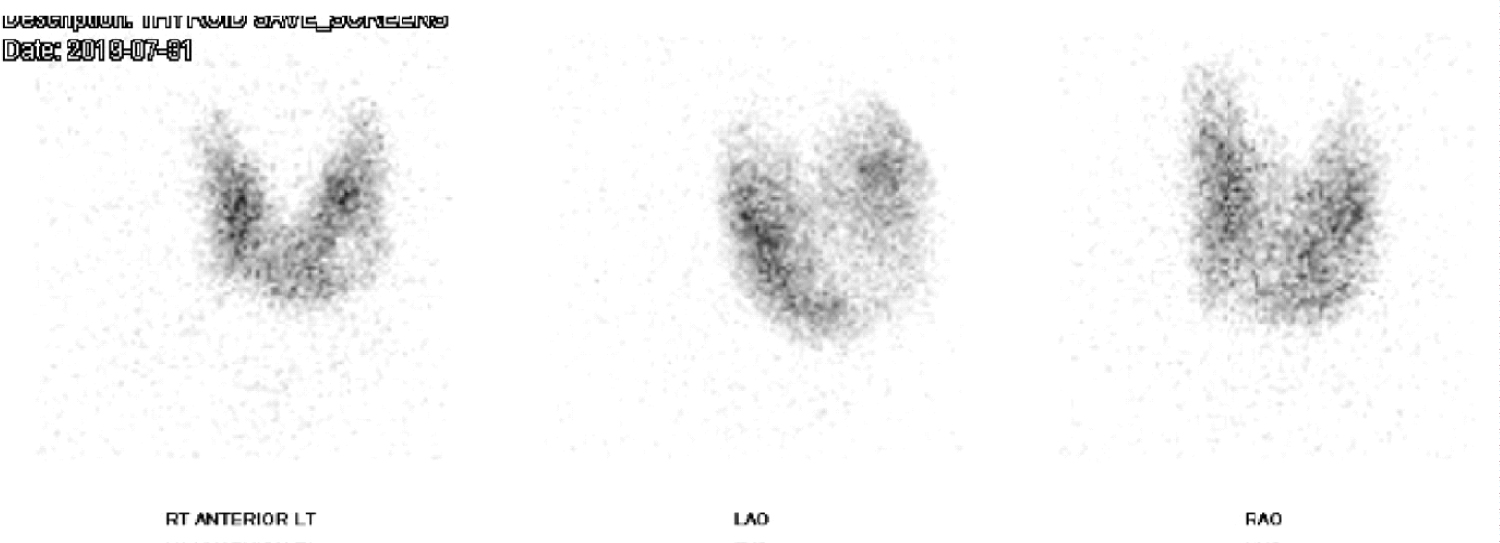 Figure 1: Cold Nodule in the Inferior Lobe demonstrated on thyroid uptake scan. View Figure 1
Figure 1: Cold Nodule in the Inferior Lobe demonstrated on thyroid uptake scan. View Figure 1
Subclinical hyperthyroidism is defined by normal T3 and T4 with subnormal TSH (< 0.5 mU/L). While overt hyperthyroidism is often misconstrued as the presence of clinical symptoms, its definition is biochemical hyperthyroidism (HT) with elevated T3, T4 (or both) and a subnormal TSH concentration. The risk of atrial fibrillation is documented to be higher in patients with TSH levels below 0.1 mU/L. Although the effect of T3 on chronotropy and inotropy is well-known, the cause of atrial fibrillation in an individual with normal free T3 remains unclear [1-4]. Causes of subclinical hyperthyroidism such as herbal supplements with iodine, biotin, Grave's or Hashimoto's Disease, and autonomous adenoma were considered but excluded during our evaluation; male sex and increasing age (> 61 years) were two risk factors for AF present on this patient.
Restoration of thyroid function, in this case, may eventually reverse his abnormal cardiovascular hemodynamics and improve his overall outcome. The benefits can be even larger if anticoagulation can be discontinued in patients with a higher risk of bleeding such as this patient.
Subclinical hyperthyroidism is associated with a higher prevalence of atrial fibrillation as exemplified by the case above. It highlights the importance of thorough work-up for causes of atrial fibrillation. It serves as a reminder to consider reversible causes of atrial fibrillation, which could change the risk-benefit assessment for anticoagulation when the underlying cause of AF can be corrected.
All authors mentioned above have contributed equally to the case.
This case report has been reviewed and accepted to be presented at Society of Hospital Medicine 2020, California.