Endoscopic ultrasound is important to assess gastric tumors in pediatric age. However, at present there is little information about its indications, applications and risks, as well as difficulty in obtaining adequate training.
A 5-year-old male patient with a gastric tumor under study, in the endoscopy, an umbilicated tumor suggestive of ectopic pancreas is observed, the endoscopic ultrasound reveals that it is dependent on the muscular layer, pathology diagnosed Gastric adenomyoma.
This is a rare tumor in the pediatric age, where among its complications is the malignant transformation. The performance of an endoscopic biopsy is not useful. Hence the great importance of performing an Endoscopic Ultrasound.
Gastric carcinomas are extremely rare in children, but common in adults, many could have been detected in pediatric age, or were mistakenly diagnosed as a benign tumor due to the lack of an ultrasound endoscopy.
EUS, Gastric adenomyoma, Gastric tumors
Endoscopic ultrasound (EUS) as a diagnostic method is a very useful tool for assessing gastric tumors in the Pediatric age. However, there is currently little information about its indications, applications and risks, as well as difficulty in obtaining adequate training [1].
Within the applications of the EUS studied in Pediatric procedures, it exists in both the upper and lower tracts: dilations, mucosectomies and polypectomies. In addition, pancreaticobiliary EUS can also be performed [1]. It is also a useful tool to study malignant tumors, performed mainly in adults, for the staging of preoperative gastric cancer, where the result can lead to important decisions for the treatment of patients [2]. In adults, the possibility of performing endoscopic diagnostic and treatment interventions for small submucosal tumors (< 3 cm) has also been studied [3].
In this case, the utility of the endoscopic US for the observation of a gastric tumor is presented, for which the type of tumor was suspected, and at what depth of the gastric tissue it was to be able to perform the appropriate management to reach the diagnosis. A partial gastrectomy excision is performed and through a pathology the diagnosis of a gastric adenomyoma was made.
5-year-old male patient, with a family history of the maternal grandfather with vascular brain disease that causes dysphasia and right hemipacies. Paternal grandfather who died from unspecified stomach cancer. The pathological personal history is pyloric hypertrophy at 3 months of age, performing a Fredet-Ramstedt pyloromyotomy without complications. Hospitalization at 2 years of age due to an uncomplicated community pneumonia, and at 3 years of age for unspecified acute sinusitis. His condition begins a year prior to hospitalization when an apparent lipoma was detected in the 0.5 cm umbilical area which was increasing in size until reaching 1 cm, 5 months prior to hospitalization involved only without treatment. For a subsequent evaluation, his pediatrician decides to perform an abdominal US where a filling defect in the gastric antrum with hypoechogenic polipoid appearance of approximately 1.5 × 0.6 cm, mobile is observed incidentally in the gastric cavity (Figure 1). A gastro-duodenal esophagus series was performed where it is reported as normal. Subsequently, an endoscopy is performed where a tumor with a punch center is observed at the level of the gastric antrum before the pylorus approximately 1.5 cm in diameter that allows the endoscope to pass through the pylorus and then into the duodenum (Figure 2), and the lateral borders of the tumor are marked with Chinese ink, later a US is performed by endoscopy which reports in the prepyloric region, an umbilized submucosal tumor, dependent on the muscular layer with a diameter of 1.6 × 0.8 cm that does not penetrates serous layer (Figure 2) and there are no perigastric adenopathies, the body and tail of the pancreas and the gallbladder are evaluated, reporting as normal. It is subsequently scheduled for a partial laparoscopic gastrectomy, in which there are no complications during the procedure. The tissue sample is sent to the pathology which reports to the macroscopic group that it weighs 3.4 g and measures 2.5 cm × 2.1 cm × 1.8 cm the largest piece and 0.3 cm the smallest, grayish, irregular surface, fibrous appearance and with a hollow consistency, a benign lesion formed by abundant smooth muscle tissue is observed at the microscopic level, in which the gastric mucosa of irregular appearance is found, as well as small pancreatic islets positive for chromogranin (Figure 3). The lesion is consistent with a gastric adenomyoma. There is no evidence of malignancy in the material examined. The patient has good post operative evolution and is discharged.
 Figure 1: Abdominal ultrasound where polypoid tumor is observed in the gastric cavity.
View Figure 1
Figure 1: Abdominal ultrasound where polypoid tumor is observed in the gastric cavity.
View Figure 1
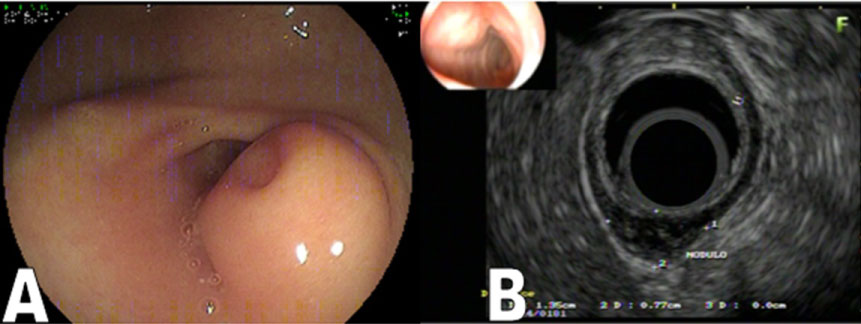 Figure 2: A) Endoscopy showing a tumor in a punch that is compatible with ectopic pancreas; B) EUS shows that the tumor is dependent on the muscle layer.
View Figure 2
Figure 2: A) Endoscopy showing a tumor in a punch that is compatible with ectopic pancreas; B) EUS shows that the tumor is dependent on the muscle layer.
View Figure 2
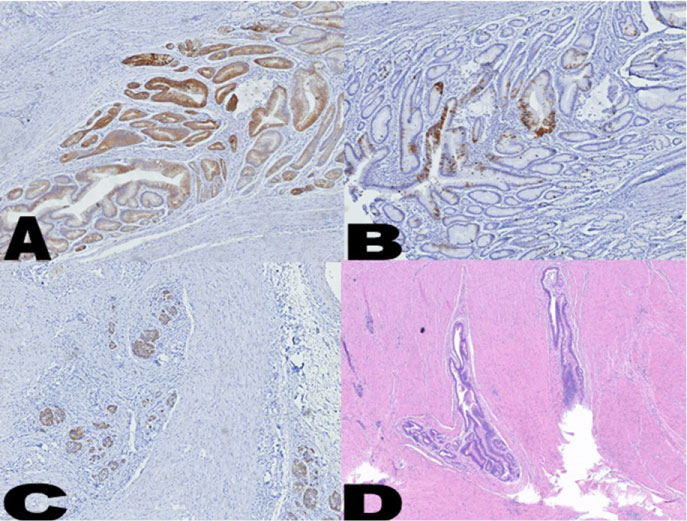 Figure 3: Tissue analyzed by pathology consistent with gastric adenomyoma. A) CK 7 immunohistochemical marker; B) CK 20 immunohistochemical marker; C) Chromogranin biochemical marker; D) Hematoxylin-eosin staining.
View Figure 3
Figure 3: Tissue analyzed by pathology consistent with gastric adenomyoma. A) CK 7 immunohistochemical marker; B) CK 20 immunohistochemical marker; C) Chromogranin biochemical marker; D) Hematoxylin-eosin staining.
View Figure 3
Adenomyomas are rare tumors composed of a combination of glandular structures intervened by bundles of smooth muscle. These are more commonly found in the pyloric area of the stomach. It is usually an incidental finding, but it can cause epigastric pain, nausea, vomiting or obstructive symptoms. Most cases occur in adults, however pediatric patients are not exempt. The most common complication is intussusception [4]. However, there may also be mass formation, inflammation, cystic degeneration and malignant transformation [5].
Unlike pancreatic heterotopia, there is not only poor epithelial accommodation, it is also accompanied by disorderly smooth muscle proliferation [4]. Other differential diagnoses include heterotopia of gastric glands, duplication, submucosal cystic glands and gastric cancer. Hence its great importance to know its pathological diagnosis. Performing an endoscopic biopsy of the lesion is not useful since the lesion is usually located in the submucosa. For this reason the great importance of knowing its location in which layer of gastric tissue is the tumor through the EUS. In addition to the great utility of the EUS to know risk factors for tumors for malignancy, in adults for GIST it has been determined: size > 3 cm, non-oval shape, irregular margins, hyperechoic foci > 3 mm, cystic spaces > 4 mm and presence of intratumoral Doppler signal [3]. Finally, surgical excision is recommended to reach a final diagnosis [5].
Malignant tumors of the gastrointestinal tract in pediatric age are very rare, being 1.2% of the malignancies. Among the most common gastric malignancies are soft tissue lymphomas and sarcomas. Gastric carcinomas are extremely rare in children, falling in 0.05% of gastrointestinal malignancies, but due to the unusual and unspecific symptoms, the diagnosis is made in advanced stages when metastases already exist and the prognosis is poor. However, this tumor is common in adults, being within the 4 most frequent tumors in world statistics [6], it is unknown how many of these could have been detected in pediatric age, or how many were wrongly diagnosed as a benign tumor due to lack of studies such as EUS.
The EUS is a new diagnostic tool with multiple utilities for the diagnosis and management of pediatric gastric tumors. However, due to lack of studies on its indications, applications and difficulty in receiving adequate training, its great benefits have not been exploited.
The EUS demonstrated its great utility for the evaluation of a gastric tumor, where we are guided on the location of the tumor, concluding that an endoscopic biopsy cannot be performed due to the depth of this and that requires a surgical resection for evaluation by pathology who concludes that it is an adenomyoma.
It is important to emphasize that if the EUS had not been performed in the patient, the lesion would have been concluded as an ectopic pancreas by endoscopy, and would have been allowed to evolve, however it could have debuted as gastric cancer in the adult. Hence the importance of performing EUS as an endoscopic diagnostic method.