A female in her 20s presents to the emergency eye clinic with a painful, red right eye (OD) with visual loss down to light perception following non-accidental penetrating trauma of an iron sewing needle two weeks prior to presentation. This is thought to be as a result of auditory hallucinations possibly from undiagnosed schizophrenia for a large proportion of her life. After extensive investigations, it was found that she had exogenous endophthalmitis from the foreign body which was treated with systemic and intravitreal antibiotics. Imaging showed a 44 mm foreign body penetrating from the right globe to the right orbital cavity and the right cavernous sinus, in close association with the right internal carotid artery. Following multi-disciplinary team (MDT) discussion, it was agreed that the following day she would undergo surgery to remove the foreign body. The extraction was successful, and recovery is ongoing with further input from psychiatry to optimally treat psychosis.
An Intraocular Orbital Foreign Body (IOFB) is any object that gets stuck within the orbit potentially causing penetrating or perforating injury of the eye. These foreign bodies can be a result of trauma, accidental or intentional injury. IOFBs occur in up to 40% of penetrating ocular injuries and can be considered a surgical emergency [1]. This depends on factors such as the size of the foreign body, its location within the eye socket, and the structures it has penetrated. Each case of an IOFB is unique and must be handled individually, as each one carries its own risks. These risks are very much dependent on the structures involved, however can include loss of the eye, permanent loss of vision, bleeding and infection, among many others.
We present a young patient with a non-accidental insertion of a metallic IOFB with vision loss and resultant endophthalmitis, an inflammation of the interior of the eye. This is, to our knowledge, the first reported case of endophthalmitis resulting from a self-inserted metallic foreign body. Endophthalmitis is a rare but serious condition that can threaten sight. Therefore, it is crucial to identify and manage it quickly and aggressively to achieve the best possible outcomes.
A patient in their 20s presented to the emergency eye clinic with a painful right eye (OD) with associated visual loss and conjunctival injection. She reports succumbing to auditory hallucinations that urged her to insert a metallic foreign object into the medial right orbit. According to the patient, two weeks from admission, she was having a steam bath at home where she burnt the right side of her face, resulting in pain in her OD. One week from admission, the pain worsened and the only way she felt she could relieve the pain and auditory hallucinations was to insert a sewing needle into the medial side of her OD. Her sight became blurry since insertion, and attended a local private clinic where the diagnosis and management were unclear. The pain and blurriness continued, and she travelled 2 hours to the eye hospital for more optimal management. She has no past ocular history of note, however her past medical history indicated a 2-year history of anxiety disorder. It is thought now that she has been suffering from psychosis for an extended period.
At the eye hospital, on examination, visual acuity was 6/10 in the left eye (OS) and limited to light perception in her OD. Her intraocular pressure was measured using an iCare tonometer and was found to be 13 mmHg in the OD and 10 mmHg in the OS. Extra-ocular motility was unaffected in both eyes. Her OD showed widespread conjunctival injection and corneal oedema with temporal subconjunctival haemorrhage. This was accompanied by swelling of the upper eyelid and contusions surrounding the eye. The anterior chamber in the OD exhibited the Tyndall effect, with cells 4+ and fibrin with a hypopyon measuring < 1 mm. The pupil was 6 mm post-dilation, RAPD was not assessed prior to dilation. On examination posteriorly, there was marked vitreous opacity, with the retina difficult to observe. The OS was normal on examination.
The patient was diagnosed with endophthalmitis of the OD suspected to be caused by the self-inflicted injury. Orbit anterior-posterior and lateral X-rays were taken, revealing the foreign body. The patient then received intravitreal antibiotic injections and aspiration of the vitreous humour for microbiological testing before being transferred to a second hospital that had the capacity to manage the complexity of her condition. Here, the patient was admitted for further investigations and management.
On examination at the second hospital, the OS was normal, OD visual acuity was light perception with an injected conjunctiva and temporal subconjunctival haemorrhage. The patient had a 4mm pupil with a negative light reflex and positive reverse relative-afference pupillary defect (RAPD). Again, the fundus was difficult to observe due to an opaque vitreous humour that obscured the view.
Initial laboratory investigations done at the second hospital revealed abnormalities in the full blood count and liver function tests. In the full blood count, there was a raised white blood cell count (WBC, 12.8 × 10 9 /L; normal range 4-11 g/L) with neutrophil dominance. There were also raised liver enzymes alanine transaminase (ALT, 240 U/L; normal range 5-49 U/L), aspartate transferase (AST, 107 U/L; normal range 9-48 U/L), gamma-glutamyl transferase (GGT, 169 U/L; normal range 4-38 U/L). The venous blood gas, clotting factors, urea and electrolytes, and glucose were within normal range. Chest X-ray and ECG were normal. Vitreous aspiration at the first hospital showed absence of bacterial and fungal growth. The second hospital continued to administer intravitreal injections without aspirating anymore vitreous humour for microbiology.
B-scan ultrasound (Figure 1) revealed a hyperechoic retina, sub-choroid and sub-tenon with orbital fluid. It was also found that there were hyperechoic, mobile streaks and clusters within the vitreous, pulling on the retina.
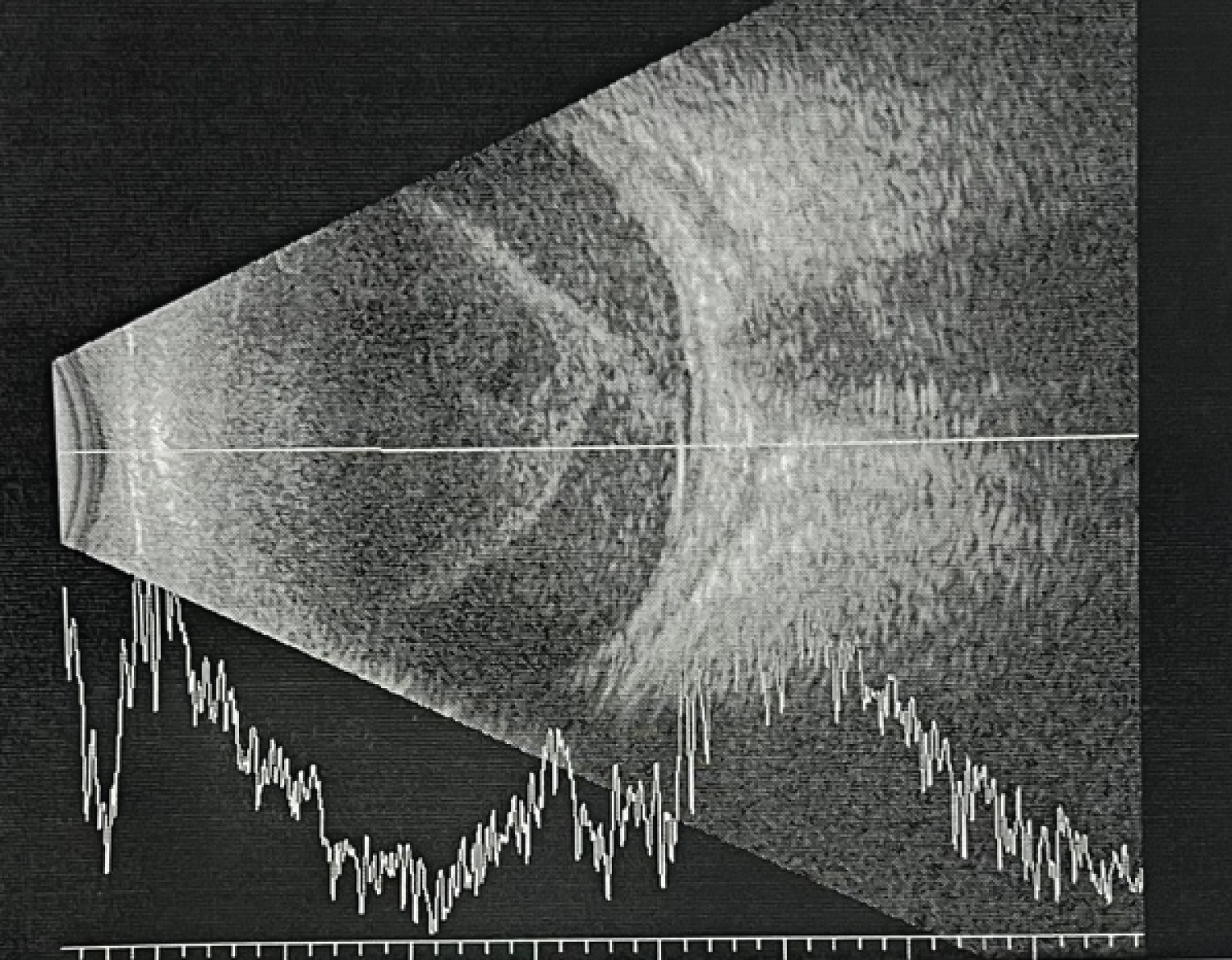 Figure 1: B scan of the right eye (OD) showcasing hyperechoic retina, subchoroid and subtenon. There are also hyperechoic, mobile streaks within the vitreous pulling on the retina.
View Figure 1
Figure 1: B scan of the right eye (OD) showcasing hyperechoic retina, subchoroid and subtenon. There are also hyperechoic, mobile streaks within the vitreous pulling on the retina.
View Figure 1
An anterior-posterior and lateral X-ray orbit at the first hospital was performed highlighting a bright foreign body in the OD measuring 42 mm following along the anterior-posterior axis of the orbit, penetrating the orbital apex into the skull base, near the pituitary sella. A CT scan with contrast followed showing a 44 mm hyperdense foreign body with the proximal end in the sclera and the distal end penetrating the orbital apex and optic canal into the right cavernous sinus (Figure 2). No intracranial lesions were found, nor any abnormalities of vessels in the cavernous sinus.
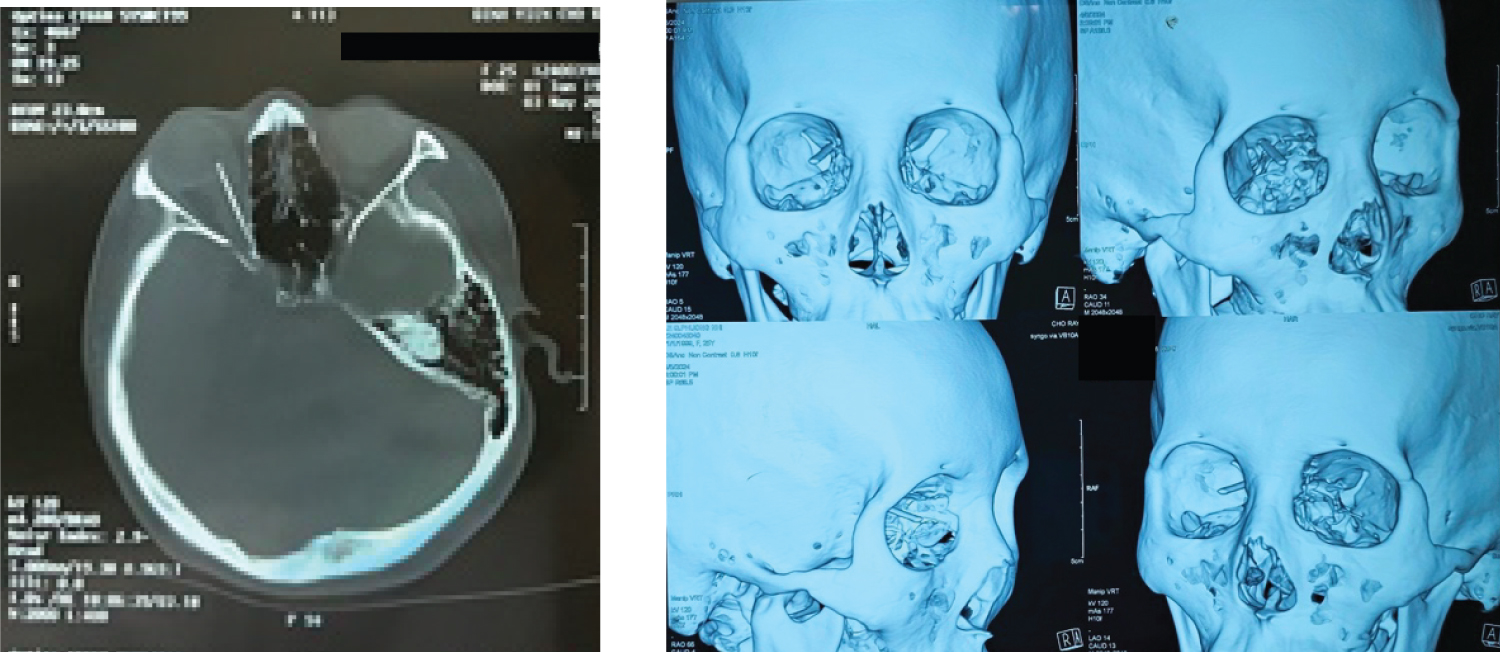 Figure 2: (a) CT head exhibiting 44 mm hyperdense foreign object penetrating the orbital apex with the distal end in the right cavernous sinus, in close proximity to the internal carotid artery; (b) 3D reconstruction highlighting the foreign body in-situ.
View Figure 2
Figure 2: (a) CT head exhibiting 44 mm hyperdense foreign object penetrating the orbital apex with the distal end in the right cavernous sinus, in close proximity to the internal carotid artery; (b) 3D reconstruction highlighting the foreign body in-situ.
View Figure 2
OD: Exogenous endophthalmitis and foreign body penetrating the orbit, the globe and skull reaching the cavernous sinus resulting in traumatic optic neuropathy.
OD: Panuveitis and foreign body penetrating the orbit, the globe and skull reaching the cavernous sinus resulting in traumatic optic neuropathy.
Ceftriaxone 2 g × 2 IV
Paracetamol 0.5 g × 3 PO
OD: Cravit 1.5% qtt 6 times a day
Intraocular injection: 2 injections with the interval of 48 hours
- mL Vancomycin (1 mg/0.1mL)
- mL Ceftazidime (2.25 mg/0.1 mL)
Surgery was performed to retrieve the foreign body with collaboration of Ophthalmology and ENT procedures.
The patient was positioned in the supine position, under general anaesthesia. The right side of face was prepared with Povidine 10%. A speculum was inserted to keep the OD open. The medial conjunctiva was dissected, and the medial rectus was fixated using Prolene 5.0. The medial rectus was then cut at its insertion. There was then further exploration until the head of the optic nerve was visualised. Here, the proximal end of the metal foreign body was located with rust. The foreign body was removed then further exploration was completed to ensure no retrobulbar haemorrhage. The medial rectus was sutured back at the insertion and the conjunctiva closed. Finally, a final intraocular injection was given at 10 o’clock including the same mix of 0.1 mL vancomycin (1 mg/0.1 mL) and 0.1 mL ceftazidime (2.25 mg/0.1 mL). As well as this, a subconjunctival dexamethasone injection was administered.
After the extraction of the foreign body, and completion of three intravitreal antibiotic injections in total, the patient’s vision improved to hand movements. Their conjunctival injection, haemorrhage, corneal oedema and anterior chamber reaction had all decreased, however, the OD RAPD remained unchanged. The patient was discharged.
Two weeks post-discharge, visual acuity in the OD had improved to counting fingers from 20 cm. B-scan ultrasound showed a hyperechoic cluster in the vitreous humour with moderate mobility like previously documented but with lesser severity.
Endophthalmitis is an inflammation that occurs within the posterior eye, typically caused by the introduction of an infectious agent. This condition often results in damage to the retina's photoreceptor cells. Despite immediate medical and surgical interventions, the infection usually leads to partial or complete vision loss within a short period, typically a few days after the infectious agent is introduced [2].
In the case of our patient, she didn't seek medical attention until about a week after the needle was inserted. As a result, the chances of her regaining any vision were very slim. However, when she arrived at the emergency eye clinic, she still had light perception in the affected eye.
Typically, infection occurs either as a complication of intraocular surgery, infection that has spread from another site (endogenous) or from an injury to the eye itself (posttraumatic). Although penetration of the globe was not directly confirmed during surgery or on investigations, it was highly suspected. In trauma-related cases presenting with severe panuveitis, despite not having an obvious penetration wound one should always have the diagnosis of exogenous endophthalmitis in mind. Furthermore, in such cases, particularly when there is a foreign body, an open globe injury should never be ruled out. In this case, when there was a reverse RAPD in the OD with imaging showing the needle’s penetration of the optic canal, the diagnosis of traumatic optic neuropathy is also made.
On review of other literature, there does not appear to be any other recorded cases of a needle being inserted into the orbit but not causing trauma to the globe. In addition, there are no other recorded cases where the patient inserted the needle deliberately. There are similar cases involving needles which have resulted in endophthalmitis however each of these has involved some form of trauma to the globe and the type of needle varies from sewing, hypodermic and veterinary needles [3-5].
Regarding the metallic foreign bodies, risk factors for these typically involve some form of trauma, whether it be from sport, violence, occupation or in our case undiagnosed psychosis. Prevention of these IOFB typically involves the use of protective eye or face wear to minimise the risk in sports, industrial jobs and in a military setting, where these injuries are seen more commonly [6]. In our case, however, a potential way in which the risk of injury could have been reduced is if the patient was able to access psychiatric interventions more promptly in order to reduce or prevent some of the auditory hallucinations she was experiencing.
Management of these foreign bodies is often on a case-by-case basis. Surgical removal of foreign bodies depends on several factors such as the size of said object, if they are organic or inorganic material (metallic needle), location within the orbit and if there has been any development of infection [7]. As in our case, the needle posed a risk to surrounding structures particularly its proximity to the right internal carotid artery as well as the development of endophthalmitis, thus surgical intervention was necessary. As the needle the patient inserted into their orbit was suspected to be iron, tetanus prophylaxis was given, however all orbital foreign bodies should be treated with prophylaxis regardless of the material [8].
Surgical extraction approaches in this particular case potentially include lateral orbitotomy either by the Stallard-Wright approach or through the upper medial eyelid and transconjunctival orbitotomy. The latter approach was chosen due to the location of the foreign body and the approach’s less invasive nature. The choice proved to be successful as the proximal end of the needle was observed in the intraconal space after conjunctival and medial rectus dissection.
In this case, while there was a delay in the patient presenting to the emergency eye clinic, the process from presentation to having the surgery was swift. Following assessment and relevant investigations carried out, she was discussed in the MDT meeting the following day for the surgery to occur the day after. The presence of a physical ophthalmological ward in the hospital potentially helped in this case as the patient was able to be monitored as well as ensuring her safety. This also allowed any updates regarding management to be communicated to the patient and to the family.
Following the surgery, while her vision had been severely affected due to the endophthalmitis that had been untreated for a prolonged period, her visual acuity had improved to hand movements.
From this case, there were some aspects of the patient’s care which could be improved upon. If documentation from the private clinic was able to be transferred, this would have allowed a better understanding of the events leading up to her presentation as well as perhaps allowing for quicker assessment and management, with time being key in endophthalmitis and the deterioration of the vision of the patient. Also, if the mental disorder that the patient was experiencing was diagnosed at an earlier date, it may have prevented this case from occurring in the first instance. Overall, though the patient is recovering well by being treated holistically from both ophthalmology and psychiatry, prompt assessment and management of cases such as this one is necessary to preserve as much vision as possible and to reduce the damage caused by orbital foreign bodies.
1. Prompt identification and treatment of intra-orbital foreign bodies is vital for the most positive outcomes.
2. Endophthalmitis is an ophthalmological emergency and prompt treatment is important to preserve vision.
3. Although no globe penetration was observed, trauma-related cases should yield a high index of suspicion for endophthalmitis in the presence of panuveitis.
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.