Transanal small bowel evisceration is a very rare presentation. However, it is associated with significant morbidity and mortality. Our case report describes an 84-year-old female with known rectal prolapse, who presented to the emergency room in sepsis with transanal small bowel evisceration after cancelation of her elective surgical repair. Due to her acutely ill presentation, she required a damage control operation, additional surgery, intensive care management, prolonged hospital stay, and a small bowel resection in addition to a colostomy. This shows the importance of timely, definitive surgical treatment for rectal prolapse, especially in healthy individuals who can tolerate surgical intervention.
Transanal small bowel evisceration was first described in 1827 by Benjamin Brodie, and based on literature, there have been about 70 cases reported to date [1]. This surgical emergency is very rare but is thought to be due to a defect in the colon or rectal wall allowing the small bowel to herniate and prolapse through the anal opening [2]. Multiple diseases can lead to perforation of the colon and rectum, such as cancer, diverticulitis, ischemic colitis, trauma, and iatrogenic injury [3]. In our case report, our patient was an elderly female with a history of rectal prolapse presenting with small bowel evisceration through her anus, who delayed her scheduled surgery.
An 84-year-old female with a medical history of hypertension, gastroesophageal reflux disease, and rectal prolapse, was referred to our Colon and Rectal Surgery office after presenting to the emergency room with rectal prolapse, which was successfully reduced. The patient reported some mild constipation requiring stool softeners and had never had a colonoscopy. On the exam, she had a reduction in anal tone, and rectal prolapse was noted with straining. After discussion with the patient and her family, the decision was made to proceed with an open rectopexy and colonoscopy. About one month after her office visit, her family canceled her scheduled surgery, reporting that the patient’s symptoms had resolved.
Two months later, the patient presented to the hospital with small bowel herniation through her anus with compromised blood supply (Figure 1), which the emergency room described to our team as irreducible “rectal prolapse.” Upon initial examination, the patient was septic with peritonitis, acute renal failure, and in the lethal triad. Due to the severity of her condition, she was emergently brought to the operating room for a damage control laparotomy with reduction of the small bowel. There was a perforated anterior wall of the very distal sigmoid colon/proximal rectum, which had allowed prolapse of the small bowel. The necrotic small bowel was resected, and the sigmoid colon was also resected down to viable rectum below the perforation. The patient was left in discontinuity with a temporary abdominal closure, and brought to the intensive care unit for further resuscitation. In 24 hours, the patient went back to the operating room for a small bowel anastomosis, creation of a colostomy and abdominal wall closure. Her postoperative course was complicated by delirium and physical deconditioning, but she was eventually discharged to rehab. Her final pathology can be seen in Figure 2.
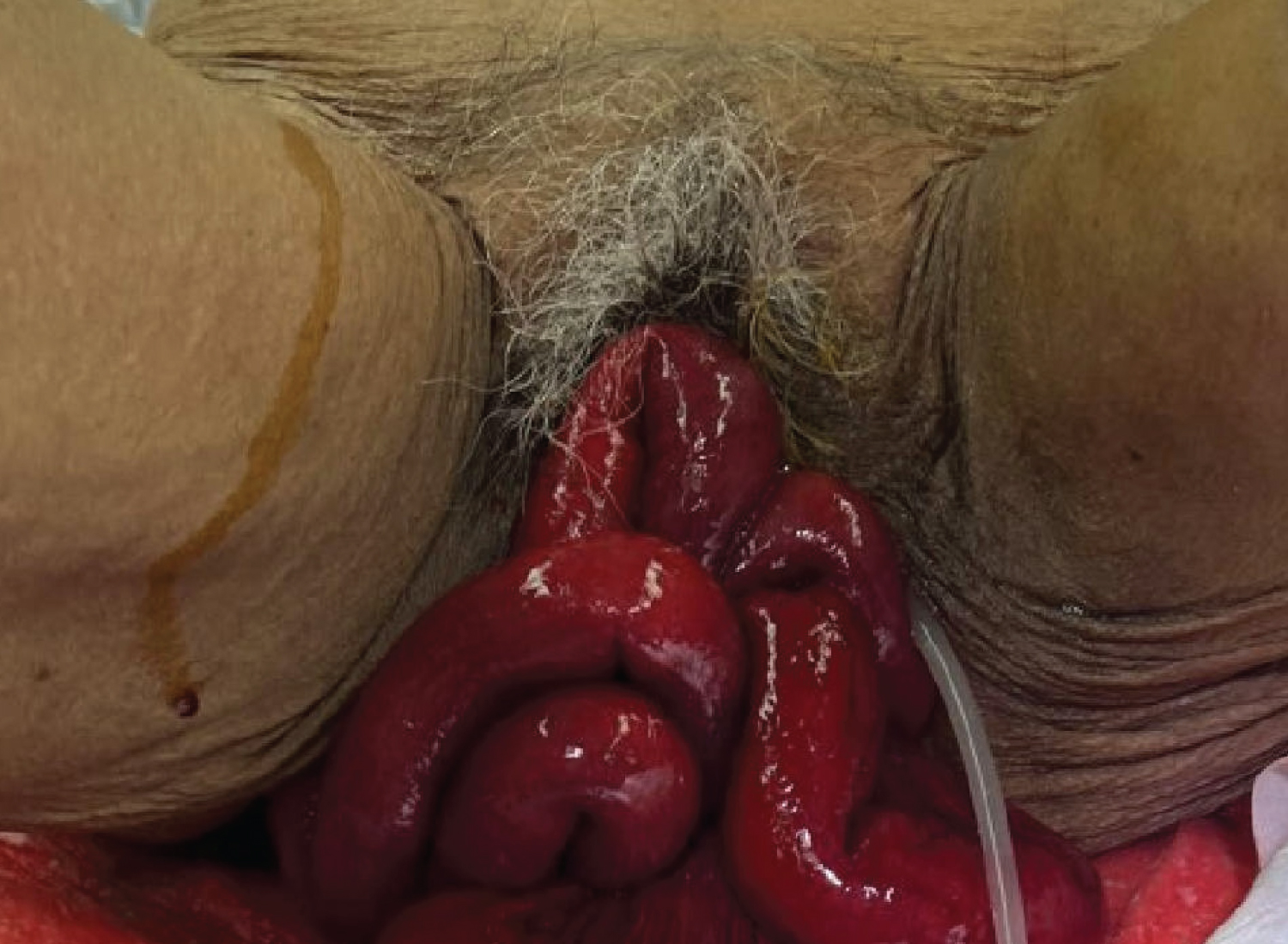 Figure 1: Evisceration of small bowel through the anus. The small bowel is showing signs of compromised blood supply.
View Figure 1
Figure 1: Evisceration of small bowel through the anus. The small bowel is showing signs of compromised blood supply.
View Figure 1
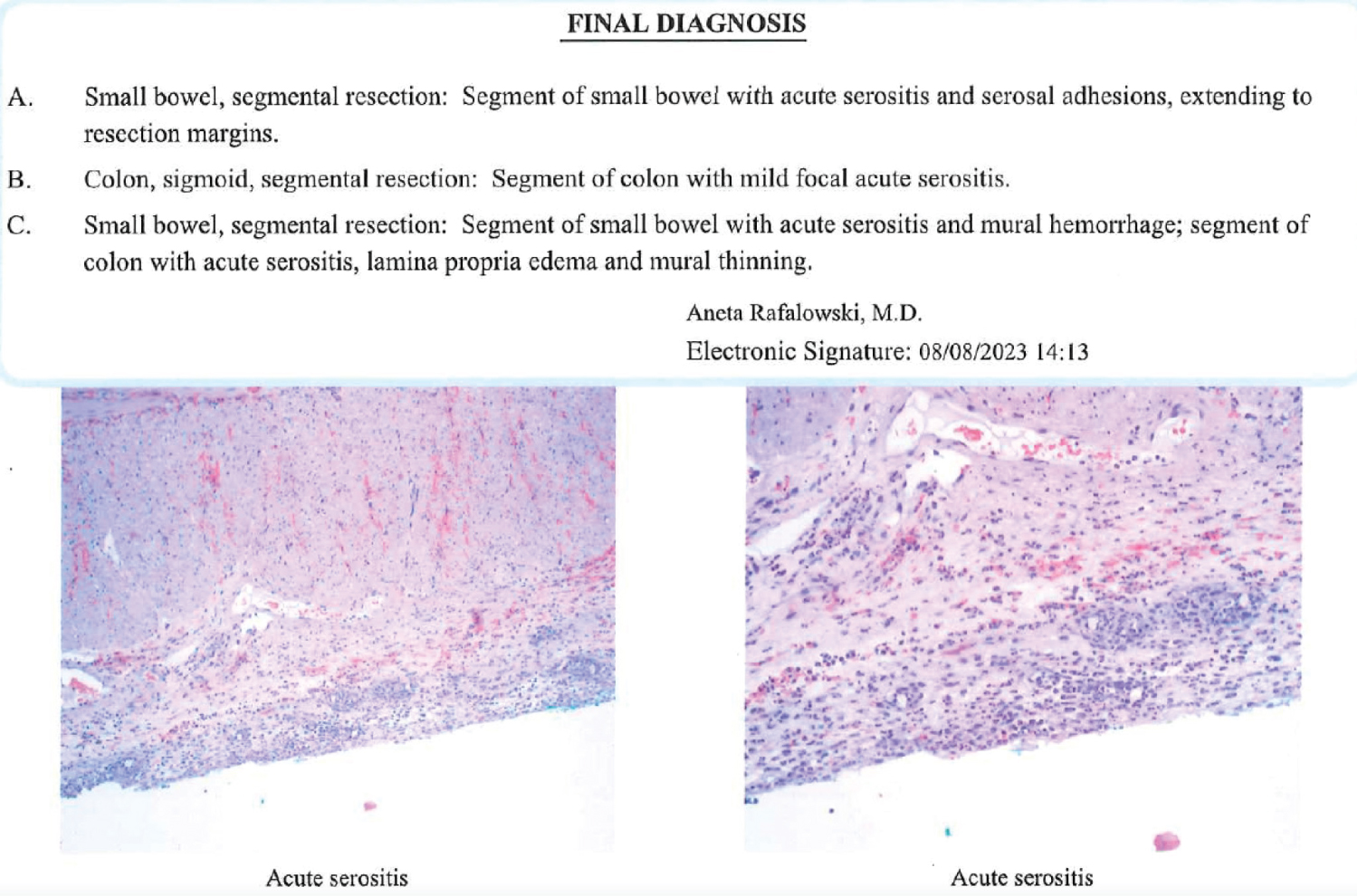 Figure 2: Final pathology results from small bowel and colon specimens. Specimens demonstrated acute serositis with no other pathology.
View Figure 2
Figure 2: Final pathology results from small bowel and colon specimens. Specimens demonstrated acute serositis with no other pathology.
View Figure 2
As demonstrated by our case report, transanal small bowel evisceration is a rare surgical emergency, which can have significant, life-threatening consequences. The exact pathophysiologic mechanism is not fully understood. However, it is thought to be caused by chronic rectal prolapse that forms a hernia sac in the pouch of Douglas [3]. This hernia sac applies pressure to the anterior wall of the rectum at the antimesenteric border. The repeated pressure to the wall results in ischemia and weakening of the wall. It is proposed that increased intraabdominal pressure from straining, vomiting, coughing, or weightlifting, can be the precipitating event that leads to perforation of the weakened wall, allowing small bowel to herniate through the defect and eviscerate through the anus [4]. Causes of spontaneous bowel perforation have been reported, such as neoplasia, colitis, diverticular disease, penetrating or blunt trauma, iatrogenic injury, chronic constipation, ulceration, suction injury, enteroptosis, forceful reduction of rectal prolapse, prolapse with chronic decubitus ulcer and pressure necrosis [1,5]. More than 75 percent of these cases were due to chronic rectal prolapse and a sudden increase in intra-abdominal pressure [2].
The management of transanal small bowel evisceration is emergent surgery. According to prior studies, when the small bowel was reduced through the anal canal without a laparotomy, these cases were predominantly unsuccessful and had a higher mortality [2]. One case that resulted in transanal reduction and repair was reported to be successful [6]. In one series, patients who were only reduced had 100% mortality [5]. When the perforation was sutured only, the mortality declined to 46%, and when the suturing was combined with a colostomy, the mortality was reduced to 23%. Importantly, patients who underwent a Hartmann’s procedure, like in our patient, demonstrated no mortalities.
In our case report, the patient presented emergently in sepsis requiring a damage control operation after canceling her scheduled surgery for her known rectal prolapse. Unfortunately, the delay in her surgical treatment resulted in her severely morbid presentation of sepsis, acute renal failure, hypothermia, and coagulopathy. Due to her acutely ill presentation, she required a damage control operation, additional surgery, intensive care management, prolonged hospital stay, and a small bowel resection in addition to a colostomy. This shows the importance of timely, definitive surgical treatment for rectal prolapse, especially in healthy individuals who can tolerate surgical intervention.
All authors contributed equally to this manuscript.