Quantiferon test (QFT) is an indirect diagnostic test for latent tuberculosis (TB) infection and active TB.
Objectives: The aim of this study is to investigate the role of Quantiferon-TB Gold test as one of the interferon-gamma release assays (IGRAs) in detecting LTBI.
Research methodology: This study was conducted at private lab in Tripoli during the period from October 2022 to January 2023, Diagnosis of 254 sample recorded. QFT was performed in accordance with the manufacturer's instructions.
Results: The study include (n = 254 cases), (58 sample 22.8%) show positive results by Quantiferon test while (196 sample 77.1%) show negative test. Females constituted 118 (46.4%) of the total cases, while the males constituted 136 (53.6%). The age (31-40 years) for the negative includes (35 cases 13.7%) while (41-50 years and (61-70 years) for positive include (11 cases 4.3%).
Discussion: This study confirmed previous reports that the QFT test had greater sensitivity for detecting active TB than the 100-year-old TST.
Conclusion: It was concluded that the quantiferon TB-2G test is a more useful diagnostic method for tuberculosis infection. QFT-Plus assay showed good sensitivity for active TB and was particularly useful for the evaluation of children with suspected LTBI, giving a low rate of indeterminate results in this group. More studies are needed to properly evaluate QFT-Plus ability in discriminating active disease from latent infection.
Tuberculosis, Quantiferon, Diagnostic, QFT-Plus, LTBI
Tuberculosis is an infectious disease caused by Mycobacterium tuberculosis. Tuberculosis typically attacks the lungs but can also affect other parts of the body. The disease has become rare in high income countries but is still a major public health problem in low- and middle-income countries [1].
Tuberculosis (TB) continues to be a global public health problem. According to the World Health Organisation (WHO) Global TB Report, one-third of the world population is infected with Mycobacterium Tuberculosis. Individuals with latent tuberculosis infection (LTBI) have a 10 percent risk of developing active TB disease during their lifetime, especially in the first two years. Diagnosis of LTBI and its treatment in high-risk populations are considered to be main components of TB control programmes [2].
Diagnosis of TB is usually based on a combination of anamnestic symptoms, clinical presentation, radiological and pathological changes, bacteriological findings of acid/alcohol-fast bacilli and molecular tests. A definitive TB diagnosis is usually based on culture of a mycobacterium of the Mycobacterium tuberculosis complex (MTB) [3].
Therefore, tools that can assist the clinician with the initial diagnosis of active TB are important because antituberculous treatment takes several months and carries a risk of serious side-effects.5 Two such diagnostic tools are the tuberculin skin test (TST) and the QuantiFERON ® -TB Gold test (QFT). The TST measures delayed-type hypersensitivity reactions to a crude mixture of mycobacterial antigens which are also present in Bacille Calmette-Guérin (BCG) vaccine strains and non-tuberculous mycobacteria. QFT is based on the the measurement of interferon-gamma (IFN-γ) secreted from T cells previously exposed to MTB when stimulated in vitro [3,4].
It is estimated that between the years 2000 and 2010, eight to nine million new cases emerged each year. Approximately 1.5 million people die from the disease each year. In adults, tuberculosis is the second leading cause of death due to an infectious disease (after AIDS), with 95% of deaths occurring in low-income countries. Tuberculosis is a major problem of children in poor countries where it kills over 100,000 children each year [5].
Tuberculosis is an airborne disease caused by the bacterium Mycobacterium tuberculosis ( M. tuberculosis ). M. tuberculosis and seven very closely related mycobacterial species ( M. bovis, M. africanum, M. microti, M. caprae, M. pinnipedii, M. canetti and M. mungi ) together comprise what is known as the M. tuberculosis complex [1].
The human tubercle bacillus ( Mycobacterium tuberculosis ) is the main cause of tuberculosis all over the world. A slightly different type of TB, Mycobacterium africanum , occurs in Africa. The only important difference is that it is often resistant to thioacetazone [1].
The bovine bacillus ( Mycobacterium bovis ) at one time caused much infection in cattle in Europe and the Americas. Infection was often passed on to man through contaminated milk. Bovine TB in milk can be killed by boiling the milk, and bovine tuberculosis rarely occurs where this is the practice. The extent of the transmission of bovine tuberculosis to humans is difficult to determine because of technical problems in isolating the organisms. One important difference is the resistance to pyrazinamide in M. bovis [1].
Diagnosing and initiating effective treatment in a patient early during their TB disease, before they can infect many people, is considered the most effective preventive measure against TB. Effective treatment substantially reduces or eliminates disease transmission from smear-positive patients in less than one month after initiation of treatment [1].
BCG is a vaccine consisting of live bacilli have lost their power to cause disease (except in persons with profound immunodeficiency). The bacilli originally came from a strain of bovine TB grown for many years in the laboratory. BCG stimulates immunity, increasing the body's defences without itself causing damage. Following BCG vaccination, in most cases the body's increased defences will control or kill any TB that enter the body [5,6].
The current recommendation by the WHO and the International Union Against Tuberculosis and Lung Disease (The Union) is that in countries with high prevalence of tuberculosis, BCG should be given routinely to all infants (but with a few exceptions, such as those known to have HIV infection and children of mothers with HIV infection at high risk of TB transmission). The normal dose in neonates and infants is 0.05 ml [1].
tuberculosis is transmitted from human-to-human and is mainly spread by airborne route. The source of infection is a patient with pulmonary or laryngeal tuberculosis (TB) who expectorates bacilli. During coughing, speaking, or sneezing, the patient produces tiny infectious droplets. These particles, called droplet nuclei, are about 1 to 5 microns in diameter-about 1-5/1000 of millimetre. Droplet nuclei can remain suspended in the air for several hours, depending on the environment [1].
Transmission may occur when these infectious droplets are inhaled. Sunlight, UV light and ventilation are effective in decreasing the ability of the droplets reaching the lung.
The other modes of transmission are far less common. Cutaneous or mucous inoculation rarely occurs, although such cases have been observed in laboratory personnel. A rare cause of digestive transmission of TB can occur with M. bovis , most commonly through cow’s milk [1].
The infectiousness of a patient is linked to the quantity of bacilli contained in his sputa. Patients with sputum smear-positive microscopy are by far the most contagious. Those with smear-negative/culture-positive results are less contagious. Patients whose sputum smear microscopy and culture are both negative are usually not contagious.
Patients who are infected with M. tuberculosis, but do not have active disease, cannot transmit TB. Extrapulmonary (EP) forms of TB are only contagious in exceptional circumstances. Children are generally much less contagious than adults. This may be due to weaker cough mechanics, less sputum production and lower bacillary load [7].
Not everyone who is exposed to an infectious TB patient becomes infected with M. tuberculosis. The probability that TB will be transmitted depends on three factors:
A. Contagiousness of the source (the greatest factor):
◦ Bacteriological status: Smear-positive being the most infectious.
◦ Virulence of the tubercle bacilli: Certain strains are very transmissible (and/or more likely to cause active disease).
B. Environment where the exposure occurred:
◦ Open air and sunlight are conditions less likely to lead to transmission, whereas small rooms/settings with no ventilation are the conditions most likely to lead to transmission.
◦ The proximity of the person to the patient is also important (i.e., sleeping next to the patient in the ward versus sleeping 20 meters away) [8].
Duration of exposure
Close contacts of TB patients are at highest risk of becoming infected with M. tuberculosis. They may be family members, roommates, friends, co-workers, or others who spend multiple hours per day with the TB patient while the person is infectious.
The best way to stop transmission is to start giving patients effective TB treatment as soon as possible. The length of time required for a TB patient to become non-infectious after starting TB therapy is not exactly known. However, once an effective TB therapy is started, if the patient follows the prescribed treatment regimen, there is considerable evidence showing the infectiousness can rapidly decline, even after a few days [9].
The skin test: The skin test is a widely used test for diagnosing TB. In countries with low rates of TB it is often used to test for latent TB infection. The problem with using it in countries with high rates of TB infection is that the majority of people may have latent TB (Figure 1) [3].
 Figure 1: Test for M. tuberculosis Infection.
View Figure 1
Figure 1: Test for M. tuberculosis Infection.
View Figure 1
The skin test involves injecting a small amount of fluid (called tuberculin) into the skin in the lower part of the arm. Then the person must return after 48 to 72 hours to have a trained health care worker look at their arm. The health care worker will look for a raised hard area or swelling, and if there is one then they will measure its size. They will not include any general area of redness [4,10].
The test result depends on the size of the raised hard area or swelling. The larger the size of the affected area the greater the likelihood that the person has been infected with TB bacteria at some time in the past. But interpreting the TB skin test result, that is whether it is a positive result, may also involve considering the lifestyle factors of the person being tested for TB. The TB skin test also cannot tell if the person has latent TB or active TB disease [11].
TB Interferon gamma release assays (IGRAs) : IGRAs are blood-based tests assessing the presence of effector and memory immune responses directed against the M. tuberculosis antigens. The IGRAs have been shown to predominantly measure the presence of M. tuberculosis specific effector memory T-cells, the presence of which are considered indicative of previous in vivo exposure to the bacilli. Blood samples might also contain central memory T-cells specific to the M. tuberculosis antigens and thus be measured in the assays. The latter is however seen as less likely, as this subset of cells react more slowly to antigen exposure and is considered to first release other cytokines during the timespan of the assays (e.g., interleukin-2) [10]. The IGRAs measure the presence of an adaptive immune response to M. tuberculosis antigens and are thus only an indirect measure of M. tuberculosis exposure (evidence is still lacking as to whether an immune response corresponds to actual infection). IGRAs have been developed for the identification of an immune response to M. tuberculosis -specific antigens, considered to be a correlate of M. tuberculosis infection, and are licensed for the use on blood specimens [11].
The Interferon Gamma Release Assays (IGRAs) are a new type of more accurate TB test. In this context referring to an assay is simply a way of referring to a test or procedure [11,12].
IGRAs are blood tests that measure a person’s immune response to the bacteria that cause TB. The immune system produces some special molecules called cytokines. These TB tests work by detecting a cytokine called the interferon gamma cytokine. In practice you carry out one of these TB tests by taking a blood sample and mixing it with special substances to identify if the cytokine is present [13,14].
There are two commercially available IGRAs:
1. Quantiferon-TB Gold In-Tube assay: The Quantiferon-TB Gold In-Tube assay (QFT-GIT), which has replaced the Quantiferon-TB Gold assay, detects the level of IFN-γ produced in response to the M. tuberculosis antigens, and uses the enzyme-linked immunosorbent assay (ELISA) detection method. This is an indirect measure of the presence of M. tuberculosis specific T-cells [15] (Figure 2).
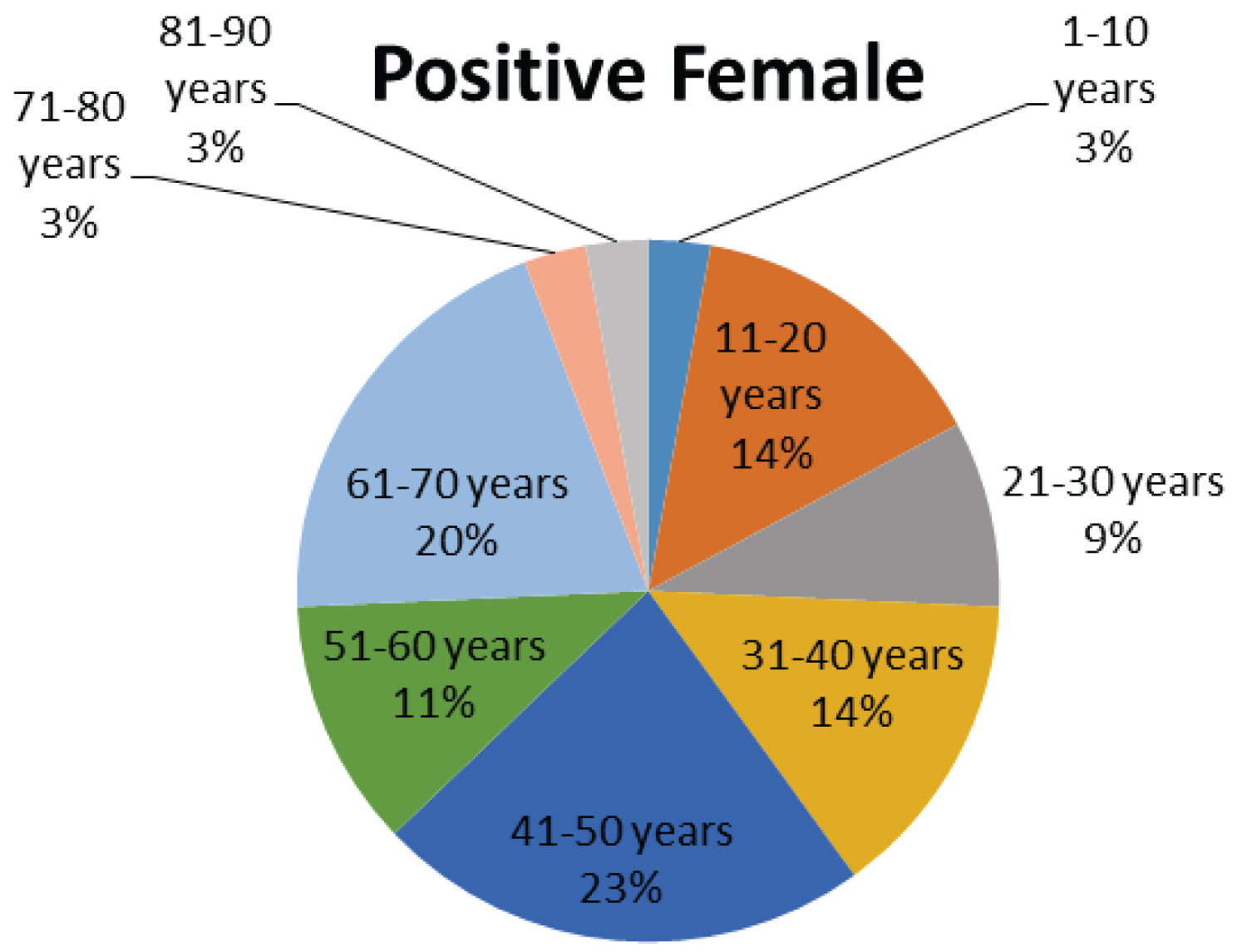 Figure 2: Shows the percentages of different age groups (positive female).
View Figure 2
Figure 2: Shows the percentages of different age groups (positive female).
View Figure 2
2. T-SPOT.TB assay: The T-SPOT.TB measures the number of IFN-γ producing T-cells in response to the M. tuberculosis antigens and is based on the enzyme-linked immunosorbent spot (ELISPOT) assay (Figure 1). Only the two commercially available IGRAs (QFT-GIT and T-SPOT.TB), both with standardised and licensed protocols that allow the comparison of study results [16-18].
QuantiFERON test (QFT) is an indirect diagnostic test for latent tuberculosis (TB) infection and active TB. The aim of this study is to investigate the role of QuantiFERON-TB Gold test as one of the interferon-gamma release assays (IGRAs) in detecting LTBI.
This study was conducted at private lab in Tripoli during the period from October 2022 to January 2023, Diagnosis of 254 sample recorded. QFT was performed in accordance with the manufacturer’s instructions.
IGRAs are performed on fresh blood specimens. The QFT-GIT is performed by drawing 1 ml of blood into one of each of the three manufacturer-precoated, heparinised tubes. Within 16 hours of blood collection, the tubes must be incubated for another 16 to 24 hours at 37 °C [19,20]. The plasma is harvested after centrifugation (QFT-GIT collection tubes contain a gel plug that separates the plasma from the cells when centrifuged) and used (immediately, or later, provided there is adequate storage) to assess the concentration of IFN-γ by ELISA test. Results are interpreted according to the manufacturer’s recommendations Table 1.
Table 1: Interpretation criteria for the QuantiFERON-TB Gold In-Tube assay (QFT-GIT) [20]. View Table 1
Table 2 shows the study include (n = 254 cases), (58 sample 22.8%) show positive results by Quantiferon test while (196 sample 77.1%) show negative test. Females constituted 118 (46.4%) of the total cases (Figure 2), while the males constituted 136 (53.6%) (Figure 3). The age (31-40 years) for the negative includes (35 cases 13.7%) while (41-50 years and (61-70 years) for positive include (11 cases 4.3%).
Table 2: Comparison of the results of the QuantiFERONTB Gold Test (QFT). View Table 2
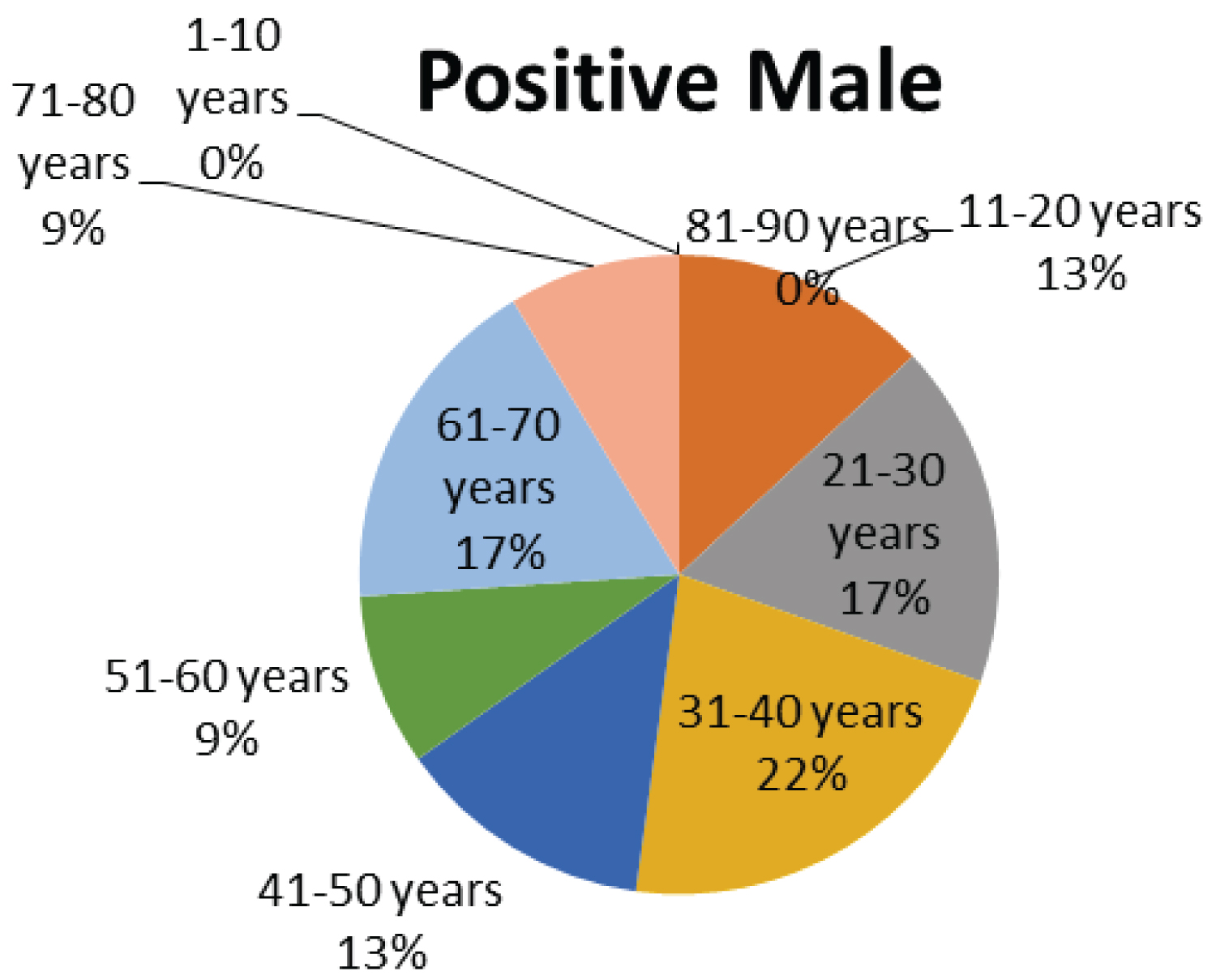 Figure 3: Shows the percentages of different age groups (positive male).
View Figure 3
Figure 3: Shows the percentages of different age groups (positive male).
View Figure 3
This study confirmed previous reports that the QFT test had greater sensitivity for detecting active TB than the 100-year-old TST.