Mycotic Aneurysms are aneurysms (or pseudoaneurysms) which result from an infectious etiology. Group-B Strep (GBS) associated mycotic aneurysms are exceedingly rare and current literature varies on presentation and diagnostic criteria. This case is a rare presentation of a likely mycotic aortic arch pseudoaneurysm induced from GBS Bacteremia and cervical osteomyelitis in a 60-year-old male.
William Osler coined the term mycotic aneurysm in 1885 to describe a mushroom-shaped aneurysm in a patient with subacute bacterial endocarditis. Originally the term was used for fungal etiologies only. The term mycotic aneurysm is now used to describe an aneurysm that results from any infectious etiology-bacterial, fungal, or viral in origin [1]. We now know that most mycotic aneurysms are precipitated by bacterial infections with Staph aureus being the most common in Western Countries [1]. Group B strep mycotic aneurysms are exceedingly rare with very few published case reports [2-12]. We report a case of mycotic aortic aneurysm suspected to be caused by GBS bacteremia in a 60-year-old male.
A 60-year-old male with a past medical history of Hypertension, Atrial Fibrillation, Insulin Dependent Type II Diabetes and remote GBS Metatarsal Osteomyelitis (2018) presented with complaints of neck pain, confusion, vomiting, and diarrhea for several days. On admission, the patient was in atrial fibrillation with rapid ventricular response and with altered mentation.
Physical examination was otherwise unremarkable except for irregular tachycardia and a left lower extremity diabetic foot ulcer. Initial labs were notable for leukocytosis 31.2, lactate 6.7, ESR 73, CRP 9.36, blood glucose 884, anion gap 41, beta hydroxybutyrate greater than 60, and creatinine of 2.42. The patient was admitted to the intensive care unit for severe sepsis, diabetic ketoacidosis (DKA) and acute renal failure (ARF). The patient was started on broad-spectrum antibiotics for sepsi and received standard medical management of his other comorbidities.
Infectious diseases work up at that time included urinalysis, urine culture, stool culture, COVID/Flu testing, and cerebrospinal fluid analysis which were all within normal limits. The patient received a computed tomograph scan of the chest, abdomen and pelvis without contrast which was also negative for an infectious source. A trans-thoracic echocardiogram revealed an ejection fraction of 55% with a small pericardial effusion and without vegetations. The patient's chronic left lower extremity ulcer was found to not be acutely infected. Due to persistent neck pain during the patient's hospitalization, an MRI of the cervical spine was obtained and revealed moderate fluid collection from C2-C6 concerning for acute discitis and osteomyelitis. Patient was evaluated by neurosurgery who recommended nonsurgical management. Blood cultures grew group B hemolytic S. agalactiae and the patient was discharged to complete a total of six weeks of intravenous Ceftriaxone.
The patient completed his outpatient antibiotic therapy and presented again to the ED two months later with recurrent neck pain. Given the patient's recent history of sepsis with cervical osteomyelitis, the patient had a repeat infectious evaluation including blood cultures, urinalysis, stool culture, and chest X-ray which were unrevealing. Included in this workup was a CT chest with contrast which revealed a pseudoaneurysm of the inferior aspect of the aortic arch measuring 3.3 × 1.6 × 2.7 cm. A CT chest without contrast one month prior to his first admission was without aneurysm. The patient was monitored with antibiotics given that there was no indication of ongoing or recurrent infection. The patient was able to be discharged home safely and ultimately received an elective minimally invasive hybrid aortic arch repair with translocation of the arch vessels and thoracic endovascular aortic repair several months later. There were no intra-operative cultures or biopsies taken. The patient recovered well from surgery.
Mycotic Aneurysms are dilations of the arterial wall caused by destruction from microorganisms [6]. They can present as true aneurysms or pseudoaneurysms [13] and are potentially fatal given their predisposition to rupture [14]. Treatment is either with intravenous antibiotics, surgical repair, or a combination of both [1,14]. GBS associated mycotic aneurysm was first described in 1989 by Blackett, et al. However, since that time GBS in the grand scheme of mycotic aneurysms has been found to be a much less common organism accounting for very few cases [2-12].
Streptococcus agalactiae is a gram-positive diplococci known for its B-hemolysis on agar plates giving its classification of Group B Strep [15]. GBS is a normal colonizer of the lower gastrointestinal tract, vagina, and upper respiratory tract. In the adult population, GBS most commonly affects patients with comorbidities such as diabetes mellitus, cardiovascular disease, and neoplasia. It is often the cause of skin and soft tissue infections as well as osteomyelitis [15].
The patient had positive blood cultures for GBS with cervical osteomyelitis and was subsequently treated with six weeks of IV antibiotics. In regard to the patient's GBS infection, the patient's comorbidities of diabetes mellitus, hypertension, and chronic diabetic ulcers predisposed him for developing GBS infections. The patient received an extensive laboratory and imaging work up for infectious source which was negative, therefore his history of GBS metatarsal osteomyelitis and chronic ulcers likely seeded the bacteremia and cervical osteomyelitis.
After his initial hospitalization, he presented two months later following completion of IV antibiotics with recurrent neck pain and was found to have a new thoracic pseudoaneurysm. Upon reviewing the medical record, the patient had received a CT of his chest without contrast one month prior to initial presentation without signs of aneurysm (Figure 1). Therefore, the patient's aneurysm likely developed from bacteremia as there was no other inciting event over this time frame. Additionally, the proximity of the patient's cervical osteomyelitis most likely played a role in the development of the aneurysm as this has been seen in other cases of mycotic aneurysm [16,17].
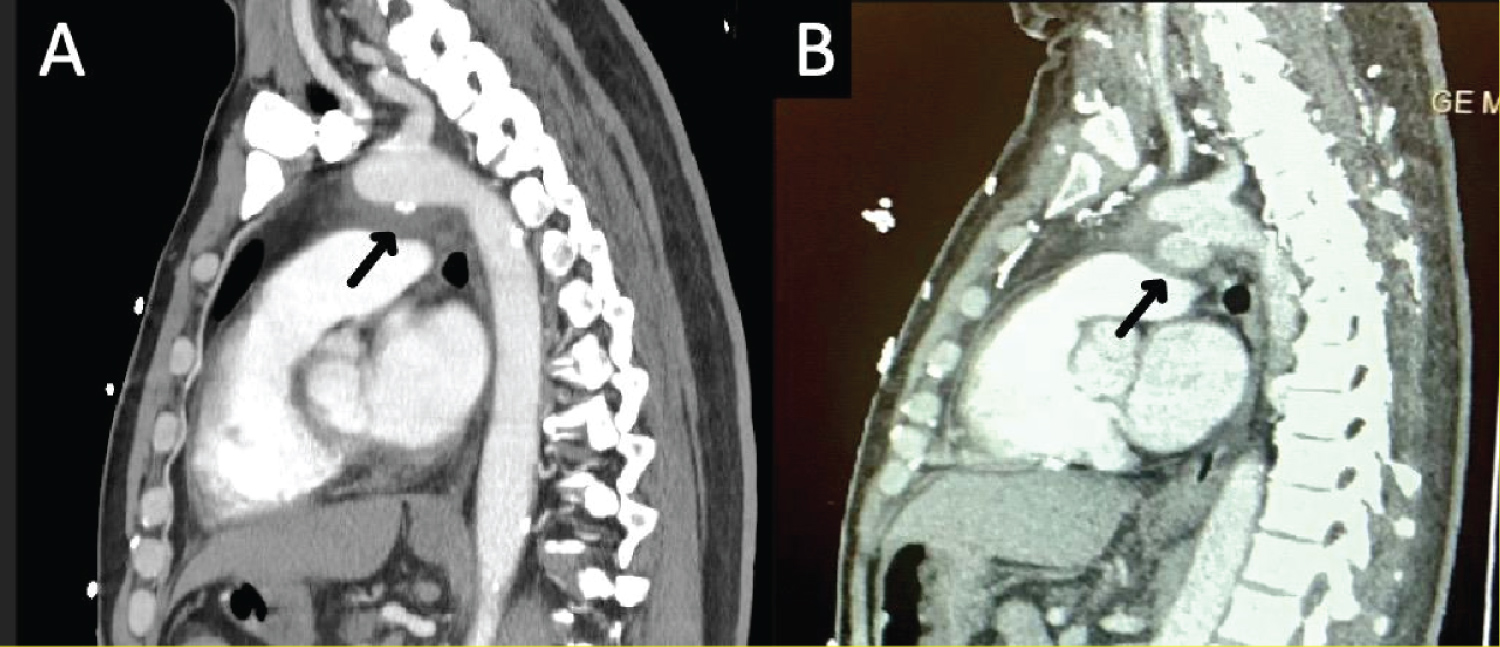 Figure 1: (A) CT chest without contrast 1 month prior to GBS bacteremia without findings of aneurysm (arrow); (B) CT chest 6 weeks after GBS bacteremia with findings of aneurysm (arrow).
View Figure 1
Figure 1: (A) CT chest without contrast 1 month prior to GBS bacteremia without findings of aneurysm (arrow); (B) CT chest 6 weeks after GBS bacteremia with findings of aneurysm (arrow).
View Figure 1
There are no official diagnostic criteria for mycotic aneurysms. However, there have been supporting criteria used in previous studies which include positive blood cultures, symptoms/signs of infection with thoracic or back pain, infectious findings on CT scans (preferred imaging modality) and intraoperative findings with positive tissue cultures [1]. The patient met the aforementioned criteria other than infectious CT scan findings and intra-operative cultures. However, the patient did complete six weeks of antibiotics which may have sterilized the aneurysm. He received surgical correction for his aneurysm five months after the initial infection and there were no infectious intra-operative findings or tissue cultures taken.
Mycotic Aneurysms are potentially fatal [14] and GBS associated aneurysms are rare. The patient reviewed in this case developed an aneurysm of the aortic arch following cervical osteomyelitis and bacteremia with GBS.
It is likely given the severity of sepsis, location of osteomyelitis and prior CT scans without findings of the aneurysm that it may have been mycotic or at least induced via GBS bacteremia.
The authors declare no conflicts of interest regarding the publication of this paper.
All authors contributed equally to prepare this article, read, and approved the final manuscript.