Through the use of imaging, liver injuries in the setting of blunt abdominal trauma have become easier to grade. These liver injury grades, formed by The American Association for the Surgery of Trauma, have been used to recommend operative versus non-operative management. However, the utilization of a relatively new approach offered by the World Society of Emergency Surgery is taking hemodynamic stability into account. As a result, more patients with severe liver injuries are being managed non-operatively. Mortality rates have improved, but morbidity continues to rise due to increased complications. This is evident in the case of C.M., a 34-year-old female involved in a motor vehicle crash who was initially managed non-operatively but was subsequently treated surgically due to progression of her hepatic injury.
Focused Assessment Sonography for Trauma, Computed tomography, Blunt hepatic trauma, Hepatic rupture, Liver trauma classification, Delayed hemorrhage
Imaging is the cornerstone of assessment in hemodynamically stable blunt abdominal trauma patients and has greatly contributed to the shift from surgical treatment to non-operative management [1]. A focused assessment sonography for trauma (FAST) exam is typically performed during the secondary survey in the trauma bay, and computed tomography (CT) often immediately follows in a stable patient. FAST exam is indicated for blunt or penetrating trauma and undifferentiated shock and/or hypotension [2]. The sensitivity and specificity of the FAST exam have been reported as 83.3% and 99.7%, respectively [3]. Currently, the Advanced Trauma Life Support (ATLS) and more than 96% of level 1 trauma centers incorporate FAST into their trauma management algorithm [2].
CT scan is the modality of choice for the evaluation of blunt hepatic trauma in hemodynamically stable patients [4] and has been shown to be more accurate in identifying intra-abdominal free fluid and organ injury. In a study conducted by Hamidi, et al. CT scan sensitivity and specificity were reported as 97% and 95%, respectively, in identifying hemoperitoneum in selected patients following blunt abdominal trauma [5]. CT scan can also accurately delineate the pathologic anatomy, help determine the severity of injuries, quantify the degree of hemoperitoneum, and reveal associated injuries to other abdominal organs, retroperitoneal structures, and the gastrointestinal tract. Lastly, it can also be used to assess complications of liver trauma and document the healing process in liver injuries while the patient is treated non-surgically [4].
The liver is the most frequently injured organ in blunt abdominal trauma [4], occurring in approximately 1-8% of cases. Roughly 85-90% of blunt hepatic traumas are treated with a non-operative approach. The published rate of successful nonoperative management of patients with isolated blunt liver injury is 91.5% for grade I and II, 79% for grade III, 72.8% for grade IV, and 62.6% for grade V injuries. Because of this shift towards non-operative management, there have been increased rates of complications, with a rise in morbidity rate to 7%. Delayed hemorrhage is the most common complication of non-operative treatment and generally occurs in the first 72 hours following the traumatic incident [6]. Delayed hemorrhage has been shown to occur in 1.7 to 5.9% of blunt abdominal injuries, most often related to either an initially small injury which has expanded or to a biloma-induced pseudoaneurysm [1].
In this report, I will review the use of imaging modalities in the assessment of a case of blunt abdominal trauma. In addition, I will cover The American Association for the Surgery of Trauma (AAST) and World Society of Emergency Surgery (WSES) liver injury grading scales. I will also review the management of blunt hepatic trauma and address the benefits and risks of the shift towards non-operative management. Finally, I will discuss the most ideal management based on our patient's presentation and hospital course.
C.M., a 34-year-old female, was a restrained driver involved in a motor vehicle crash (MVC). She was moving from a stopped position when another car hit her vehicle. It is unknown how the other car hit her vehicle or at what speed they were traveling. Airbags were deployed. Patient denied loss of consciousness as well as head and neck pain. She was ambulatory at the scene but was limping due to injury of her right foot. She was transferred to the local emergency department via ambulance for further assessment and treatment. Imaging from the outside hospital revealed a grade 2 liver laceration and confirmed a right open comminuted calcaneal fracture. The patient became hypotensive and required 1 unit of packed red blood cells (PRBCs) as well as tranexamic acid. Labs were drawn which revealed a hemoglobin 13.4 g/dL and EtOH 236 mg/dL. She was then transferred to a level 1 trauma center for further management. C.M. was given ketamine and another unit of PRBCs en route.
Upon arrival to the level 1 trauma center, C.M. underwent primary and secondary survey. She smelled of alcohol and was not in an Aspen collar. C.M. was phonating with equal bilateral chest rise and unlabored breathing. Lungs were clear to auscultation bilaterally. Heart had regular rate and rhythm with pulses 2+ dorsalis pedis, femoral, and radial bilaterally. She was GCS 15 with pupils 4mm as well as equally round and reactive to light bilaterally. Her right open comminuted calcaneal fracture presented with normal sensation, pulses, and capillary refill; right toes were limited to range of motion secondary to pain. Abdomen was soft and non-distended with right-sided tenderness. FAST exam was negative, and a small, superficial abrasion was present over the epigastric region. The pelvis was stable to anterior/posterior and lateral compression. Furthermore, she was negative for midline thoracic, lumbar, and sacral tenderness and step-offs. A normal gluteal squeeze was observed. The remainder of the physical exam showed no abnormalities.
During the initial survey, C.M. endorsed 9/10 pain in the right abdomen and right ankle that was constant and worsened with movement. She denied chest and back pain and continued to deny head and neck pain. A full review of systems was completed and was noncontributory outside of the symptoms previously mentioned. Orthopedics was consulted; irrigation and splinting of the right calcaneus was performed in the trauma resuscitation bay. Afterwards, C.M. was found to be hemodynamically stable and was transferred to the floor. Labs showed her hemoglobin rose to 15.4 g/dL, from 13.4 g/dL at the outside hospital. She was given a NPO diet as orthopedics anticipated open reduction and internal fixation of the right open comminuted calcaneal fracture the following day.
Overnight, C.M. had a vasovagal event as she used the bathroom; she did not fall or further injure herself during the event. However, she was found to have nausea and emesis during our morning rounds. When reassessed later that day, C.M. had worsening abdominal discomfort with persistent nausea. A CT scan was performed that revealed a larger liver laceration when compared to the CT scan from the outside hospital as well as extensive hemoperitoneum (Figure 1). C.M. was evaluated by the surgical team, and operative management was elected to control her bleeding, debride her liver injury, and evacuate the hemoperitoneum. The patient was informed of the findings and consented to the procedure. Blood was ordered on-call, and the operating room was informed of the emergency procedure.
 Figure 1: CT scan showing significant liver laceration with extensive hemoperitoneum.
View Figure 1
Figure 1: CT scan showing significant liver laceration with extensive hemoperitoneum.
View Figure 1
The patient was taken to the operating room and was prepped and draped in the usual sterile fashion. General anesthesia was initiated and endotracheal intubation was performed. There were no signs of cardiovascular or respiratory compromise. A time-out was taken to identify the correct patient, equipment, and operating procedure; all were in agreement and the operation proceeded as planned. Additionally, C.M. was given preoperative and perioperative doses of Ancef.
Midline laparotomy and entrance into the peritoneum demonstrated significant hemoperitoneum, as anticipated from the pre-operative CT scan. The abdomen was packed with laparotomy pads in all four quadrants, and pads were removed sequentially from least to most obvious signs of bleeding. Evaluation of the stomach demonstrated no injury. The small bowel was then investigated from the Ligament of Treitz to the ileocecal valve. After mobilization of the splenic flexure, the colon was inspected circumferentially from rectum to cecum. No injuries were noted to the large or small bowel. The diaphragm was examined without injury. A grade 5 liver laceration was noted with rupture of the dome (Figure 2). The hemoperitoneum was evacuated from the abdomen, and Evarrest was used for bleeding control. Irrigation was performed, and stoppage of bleeding was confirmed. Fascia was closed using looped PDS suture, and the skin was stapled shut. The closed skin was then covered by an abdominal pad dressing.
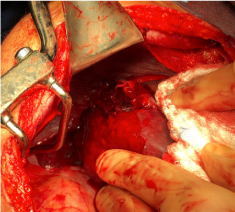 Figure 2: Intraoperative image of AAST grade 5 liver laceration with rupture of the dome.
View Figure 2
Figure 2: Intraoperative image of AAST grade 5 liver laceration with rupture of the dome.
View Figure 2
C.M. remained hemodynamically stable throughout the remainder of her care. Hemoglobin was trended and remained within normal limits. She was appropriately tender on serial abdominal exams without nausea or vomiting. Later in her hospital stay, she was taken back to the operating room for open reduction and internal fixation for her right open comminuted calcaneal fracture; she tolerated the procedure well. She remained non-weight bearing of the right lower extremity for the remainder of the hospital course. C.M. had return of normal bowel function before her discharge and was scheduled for outpatient physical therapy for her right calcaneal fracture.
The predominant cause of blunt hepatic trauma is due to motor vehicle accidents. Signs and symptoms can vary, but hepatic injuries can present with right upper quadrant pain and peritoneal symptoms, which include rebound, rigidity, and voluntary guarding. Liver enzymes may be elevated secondary to injury or a pre-existing condition, such as alcoholism and fatty liver to name a few [7]. Management of hepatic injury has transitioned from surgical to non-operative, largely due to the efficiency and accuracy of imaging modalities. Patients who are hemodynamically unstable, have evidence of peritoneal signs, or are found to have a positive FAST exam undergo immediate laparotomy.
However, most patients present to the trauma bay hemodynamically stable. A number of algorithms have been proposed for the management of hepatic injury due to blunt trauma. An excellent, simplified version of management for blunt abdominal trauma from Sabiston Textbook of Surgery can be viewed in Figure 3 [8]. The Advanced Trauma Life Support (ATLS) definition considers an "unstable" patient to have a blood pressure < 90 mmHg, heart rate > 120 bpm, evidence of skin vasoconstriction (cool, clammy, decreased capillary refill), altered level of consciousness, and/or shortness of breath [9].
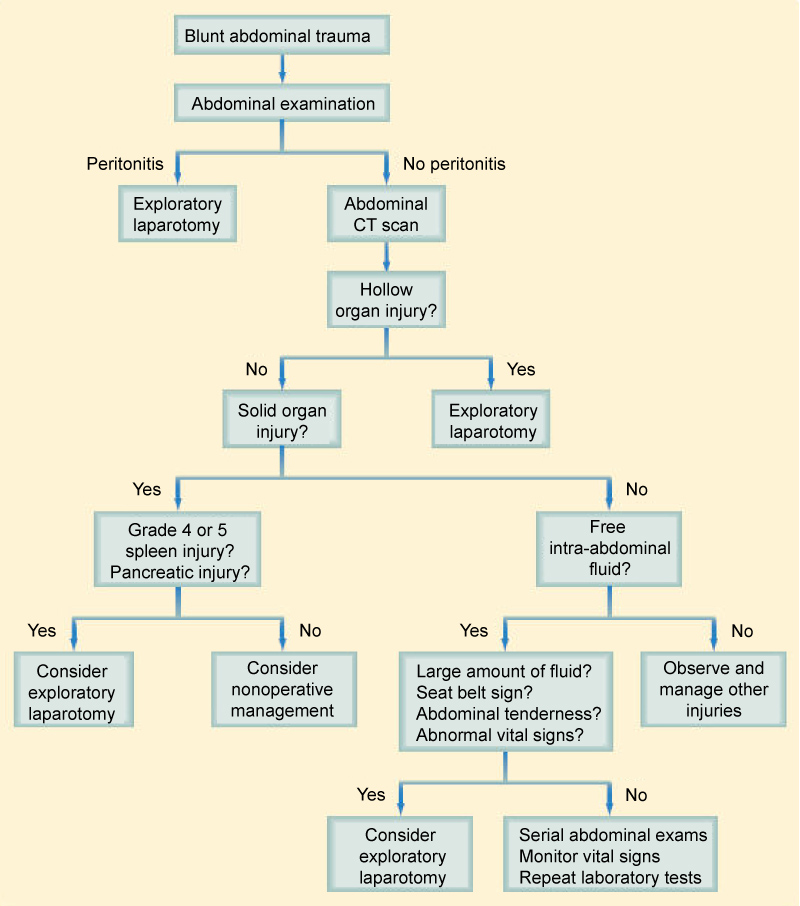 Figure 3: Algorithm for the evaluation and management of blunt abdominal trauma from Sabiston Textbook of Surgery.
View Figure 3
Figure 3: Algorithm for the evaluation and management of blunt abdominal trauma from Sabiston Textbook of Surgery.
View Figure 3
In addition to the management algorithm from Sabiston Textbook of Surgery, the World Society of Emergency Surgery (WSES) has also proposed an algorithm for management of hepatic injury secondary to blunt abdominal trauma based on a classification system similar to the American Association for the Surgery of Trauma's (AAST) liver injury scale. The AAST liver trauma classification system can be viewed in Table 1. The WSES liver trauma classification provides a new grading system of WSES I, II, and III for minor, moderate, and major/severe hepatic traumatic lesions, respectively (Table 2). AAST grades I and II are typically categorized under WSES I, AAST grade III under WSES II, hemodynamically stable patients with grade IV or V injury under WSES III, and any hemodynamically unstable patient under WSES IV. Lastly, if hemodynamic instability is present, operative management is warranted [9].
Table 1: AAST Liver Trauma Classification [9]. View Table 1
Table 2: WSES Liver Trauma Classification with corresponding AAST liver trauma grades [9]. View Table 2
Operative management via laparotomy is reserved for hemodynamically unstable patients. The laparotomy begins with a midline incision along the linea alba from the xiphoid to the pubic symphysis that often spares the umbilicus. Hemorrhage is initially controlled via direct pressure using packs but can also include compression of the aorta superior to the celiac trunk or utilization of the Pringle maneuver, if necessary. Depending on surgeon preference, experience, and the extent of injury, a surgeon can perform the finger fracture method, omental packing, resectional debridement, anatomical resection, or use polyglactin mesh [7].
Non-operative management remains the gold standard for the majority of liver injuries. It has been shown that non-operative management is associated with fewer blood transfusions as well as decreased mortality rate when compared with operative management [10]. In a study by Christmas, et al. only 2.2% of high-severity liver injuries (Grades III-V) that were managed non-operatively resulted in death. Furthermore, non-operative management succeeded in > 95% of cases when patients are appropriately selected, and only 11% of cases initially managed non-operatively required an adjunctive procedure for successful management [11]. When managing a patient non-operatively, it is imperative to perform serial clinical evaluations and have access to an operating room in case urgent operative management is required. Both the risk of delayed hemorrhage and hollow organ injury, although minimal, is increased in non-operative management of blunt hepatic injuries secondary to trauma [7]. If a patient is hemodynamically stable with active contrast material extravasation noted on CT or there are clinical signs of ongoing hemorrhage without another identifiable source, they may undergo transarterial embolization (TAE) [4]. However, if they progress to a hemodynamically unstable condition, operative management becomes the treatment modality of choice.
As the number of non-operatively managed severe, hemodynamically stable liver injuries has risen, so has the prevalence of delayed complications. The reported percentage of delayed complications ranges from 5-23% and includes but is not limited to: Delayed hemorrhage, abscess, biloma, pseudoaneurysm, hemobilia, and bile leak [4].
Delayed hemorrhage is the most frequently seen complication of non-operative management, occurring in roughly 1.7-5.9% of cases. It is more commonly associated with severe liver injuries (grades IV-VI). However, it can also occur secondary to either a small injury that continues to grow or biloma-induced pseudoaneurysm that results in an expanding hematoma or free intraperitoneal rupture [1]. The proposed mechanism of delayed bleeding is due to clot breakdown from fluid absorption. The absorbed fluid causes an increased size and pressure within the injured liver parenchyma that eventually results in tearing of the tissue and bleeding. If sustained, bleeding can form a pseudoaneurysm, arteriovenous fistula, or rupture into the peritoneal cavity [6]. Delayed bleeding can be treated through TAE in the hemodynamically stable patient with a success rate of 90% and all-cause mortality < 10%. Complications of TAE are rare but include: bile leak, hepatic necrosis, abscess formation, and gallbladder infarct if the cystic artery is accidentally embolized. Most of these complications can be managed non-operatively or through endovascular approaches [12].
Abscesses are found in 0.6-4% of non-operatively managed cases and are typically identified on follow-up CT as focal areas of fluid with or without bubbles or air-fluid level. Patients present with abdominal pain and tenderness, fever, and leukocytosis days to weeks after the traumatic event. Like delayed hemorrhage, it is also associated with severe liver injuries that are managed non-operatively. Percutaneous catheter drainage has become the first-line treatment of abscesses secondary to blunt hepatic trauma [4].
Bilomas can occur in 2-12% of cases and present on CT as a "well-circumscribed intraparenchymal or perihepatic collection, with low attenuation and progressive growth". Most resolve spontaneously over the course of weeks to months [1].
Hepatic artery pseudoaneurysms are a rare complication of blunt abdominal trauma, only occurring in 1% of cases. Decompression of the pseudoaneurysm into the biliary system causes hemobilia. Expression of blood from the biliary system into the duodenum can then result in melena or hematemesis. Arterial embolization is the treatment modality of choice, which can be performed immediately following diagnostic arteriography [4].
Lastly, bile leaks can occur as a result of hepatic laceration. The majority of cases resolve on their own with intervention rarely needed. However, when injury to an intrahepatic duct occurs, passage of bile into a hematoma can result in an increased pressure within the hematoma, leading to tissue necrosis and biloma formation [4].
Hematomas and bilomas may persist for years, but hemoperitoneum, subcapsular hematoma, and lacerations will resolve within weeks. Most of these complications do not impact overall mortality but do increase the length of hospital stay [4].
Osteopathic considerations can be made in hemodynamically stable patients whose pain is adequately managed. Trauma can cause muscle strain, lymphedema, and overactivation of the sympathetic nervous system. Therefore, strain counterstrain, myofascial release, rib raising, and various forms of muscle energy, such as crossed extensor reflex, respiratory assist, and oculocephalogyric reflex, can be performed to address these concerns but are also dependent on the extent and location of the traumatic injuries. In addition, osteopathic manipulative medicine can also be performed on an outpatient basis [13].
Advancements in imaging modality and the introduction of TAE have led to the new gold standard of non-operative management in hemodynamically stable patients following blunt hepatic trauma. ATLS and roughly 96% of level 1 trauma centers have incorporated FAST into their trauma management algorithm [2]. Although the sensitivity of FAST exams have been reported around 83.3% [3], false negative studies were not associated with increased mortality, prolonged time in the ICU, or lengthened hospital stay. Additionally, patients with false negative FAST exams were actually less likely to undergo a laparotomy [14]. In hemodynamically stable patients with blunt abdominal trauma, serial FAST exams or an early CT should be considered if it is believed that the result of the FAST exam is a false negative [15]. Despite C.M.'s CT scan from the outside hospital, we could have immediately performed a CT scan after our secondary survey in the trauma bay. This could have prevented the progression of C.M.'s liver injury and allowed for earlier intervention with possible TAE.
Regardless of our shortcoming in non-operative management, the published rate of success of such treatment in patients with blunt hepatic injury is 91.5% for grades I and II, 79% for grade III, 72.8% for grade IV, and 62.6% for grade V. The overall 90-day morality rate ranges from 0-8%, with up to 4% directly contributed from the extent of liver injury [12]. Yet, the non-operative mortality rate remains superior when compared to operative management. However, the increase in non-operative management has resulted in increased morbidity, now at 7%. The most common of these complications is delayed hemorrhage, which typically occurs within the first 72 hours following the traumatic incident [6].
There are very few changes that could have been made in the management of C.M.'s case that would have offered a more ideal outcome. Fluid boluses could have been given to C.M. at the outside hospital and en route to the trauma center instead of PRBCs. Also, a CT scan after initial survey in the trauma bay or immediately following her vasovagal event could have been performed. Likewise, serial FAST exams could have been done instead of a CT scan. These imaging modalities may have caught the expansion of C.M.'s injuries and allowed for the utilization of TAE instead of operative management. By the time the second CT scan was performed, the extent of injury and the questionable stability of C.M. deemed operative management necessary.
This report was meant to address the significance of imaging, the similarities and differences of the AAST and WSES liver trauma classifications, and the risks, benefits, and indications of non-operative versus operative management in the setting of blunt hepatic trauma.
• Dr. Mary Froehlich, for the provision of patient notes and images in the case of C.M.
• There are no conflicts of interest to disclose.
• There is no financial support to disclose.