Quite a few studies have focused on the postoperative blood loss of total knee arthroplasty, However, these studies have generally not reported the difference of the blood loss with or without haemostasis after the tourniquet released in minimally invasive total knee arthroplasty (MIS-TKA).
Eighty-four patients were recruited for a cohort study of the minimally invasive total knee arthroplasty (MIS-TKA) for the treatment of osteoarthritis. They were divided into two groups, 42 patients with thorough haemostasis in the minimally invasive total knee arthroplasty (group A) and the other 42 patients without a thorough haemostasis procedure in the minimally invasive total knee arthroplasty (group B). The surgery in both groups was carried out by a single surgeon at one institution using a uniform approach. The blood loss in each group was evaluated and analyzed for the statistical difference.
The result showed that the mean blood loss from the drainage of the group A (329.69 ± 195.31 milliliters) was slightly lower than the group B (406.31 ± 239.33 milliliters), which had no significant difference (p-value 0.552). Moreover, the whole blood loss in the group A (826.45 ± 391.63 milliliters) was slightly lower than the group B (975.22 ± 389.76 milliliters). The difference was also not statistically significant.
With a thorough haemostasis procedure did not reduce blood loss in the minimally invasive surgery total knee arthroplasty (MIS-TKA).
Total knee arthroplasty (TKA) is one of the most commonly performed elective orthopaedic procedures for osteoarthritis patients. TKA can be associated with significant postoperative blood loss and requirie blood transfusion and hematinics [1,2]. Femoral canal is one of the major sources of bleeding during and after operation, which is breached to allow passage of an intramedullary rod in the operation procedure. In 1988 Berman, et al. [3] estimated that recording drain outputs was not adequate to allow quantification of overall blood loss. Post-operative blood loss may be considerable in reference to calculated blood loss [4], even if the use of a tourniquet allegedly minimises intraoperative blood loss. We wonder whether a thorough haemostasis after the tourniquet is released during the operation is helpful to decrease postoperative drainage blood loss. So we assessed the effects of using a thorough haemostasis by releasing the tourniquet during the operation of MIS-TKA in a prospective randomised study with special reference to measured blood loss in suction drainage, total calculated blood loss, transfusion requirements. To our knowledge it is the first such study on total calculated blood loss with or without thorough haemostasis by releasing the tourniquet during the operation.
84 consecutive patients (41 males and 43 females) who underwent primary TKA between September 2010 and December 2012, were included in the study. The study population was divided evenly into two groups of patients who underwent surgery with the same surgeons in: group A (20 males and 22 females) and group B (21 males and 21 females) Table 1, following the same arthroplasty model and similar pre and postoperative procedures. All patients suffered from knee osteoarthritis, which had not improved with medical treatment and which presented a less than 10° deformity in the coronal and sagittal radiographic projections. Patients who underwent revision surgery and complex primary total knee arthroplasty in cases with significant deformity or bone defects which would require any procedure other than a standard primary arthroplasty procedure were excluded.
Table 1: Comparing the demographics, clinical and surgical details of patients in both groups. View Table 1
We explained to the patient the type of surgery in the moment of random assignment. Written informed consent was obtained from all patients, and the study was approved by the National Ethics Committee. Clinical data were collected and measured by the authors or their research assistants.
All procedures were performed using the same fixed bearing posterior stabilized implant (Link GEMINI MK Ⅱ, Germany) and using a minimally invasive mini midvastus approach. This technique utilizes small incision and down-sized instruments, which help in minimizing soft tissue dissection with no patellar eversion and no tibiofemoral joint dislocation. Patients had general anaesthesia. No fibrinolytic agents were used. The tourniquet pressure was at 280-300 mmHg according to the patients` artery pressure. The incision was typically less than 9-cm long, which represented no more than twice the length of the patella. The patients of group A underwent a thorough haemostasis by releasing the tourniquet after the cemented prosthesis fixed during the operation (we used either electrocoagulation or bone wax to stop the significant bleeding from the tissue and bone). In group B, we used the tourniquet all through the operation and there were no significant bleeding at all, since the tourniquet worked through the operation. After the closure of the wound, we used elastic bandage for both group and one redivac suction drain was routinely used in all patients and removed within 24 h. The threshold for transfusion was hemoglobin (Hb) concentration less than 7.5 g/dL in accordance with hospital protocol. Demographic and clinical data were recorded.
Statistical analysis was performed using the Student's t-test (Graph Pad Prism software, Graph Pad, California, USA). The level of significance for this study was set at P < 0.05.
In group A, we did a thorough haemostasis by releasing the tourniquet after the cemented prosthesis fixed during the operation by using either electrocoagulation or bone wax to stop the significant bleeding from the tissue and bone. In group B, we used the tourniquet all through the operation and there were no significant bleeding at all, since the tourniquet worked through the operation. And we did not perform any haemostasis action at all. After the closure of the wound, we used elastic bandage for both group and one redivac suction drain was routinely used in all patients and removed within 24 h. (Figure 1, Figure 2 and Figure 3). Comparing the demographics, clinical and surgical details of patients in both groups (Table 1).
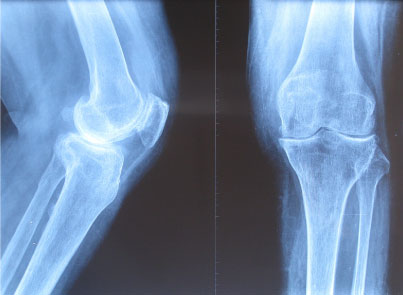 Figure 1: Case 1 Female, 68-years-old, with stiffness knee and continuous pain. Preoperation x-ray. View Figure 1
Figure 1: Case 1 Female, 68-years-old, with stiffness knee and continuous pain. Preoperation x-ray. View Figure 1
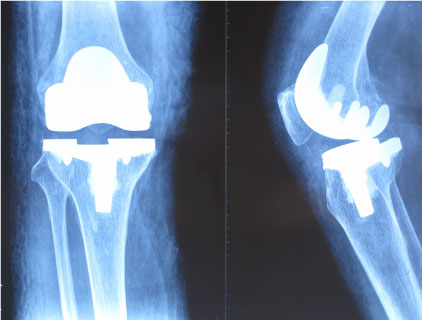 Figure 2: X-ray of the post-operation with a total knee arthroplasty. View Figure 2
Figure 2: X-ray of the post-operation with a total knee arthroplasty. View Figure 2
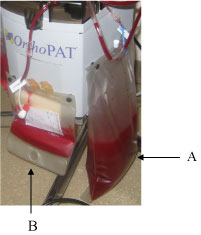 Figure 3: The drainage of the two groups, A was the drainage from the group A (without the tourniquet release during the operation), B was from the group B (with the tourniquet release during the operation). View Figure 3
Figure 3: The drainage of the two groups, A was the drainage from the group A (without the tourniquet release during the operation), B was from the group B (with the tourniquet release during the operation). View Figure 3
The average preoperative Hb was 12.78 g/dL (range 8.6-16.4 g/dL) (SD: 1.59, 95% CI: 11.28-13.75) in the group A and 13.37 g/dL (range 9.5-15.9 g/dL) (SD: 1.38, 95% CI: 12.41-13.76) in the group B (P = 0.82). The average tourniquet time was 68 min (range 45-65 min) in the group A and 89.7 min (range 70-135 min) in the group B (P = 0.47). The average postoperative Hb in the group A was 10.54 g/dL (range 7.6-14.6 g/dL) (SD: 1.54, 95% CI: 9.79-10.89) and 10.21 g/dL (range 7.2-12.4g/dL) (SD: 1.25, 95% CI: 9.79-10.57) in the group B (P = 0.15). Six patients in group B and four in group A required blood transfusions. Six patients of group B and eight patients in the group A were placed on hematinics (Table 2). The mean drain collection was 199 mL (range 150-400 mL) in the group A and 462 mL (350-600 mL) in group B (P = 0.163).
Table 2: Parameters used to estimate blood loss in the group A and B. View Table 2
TKA can result in significant blood loss [5]. The average reduction in Hb concentration after TKA has been estimated to be 3.85 g/dL.6 Up to 18% of these patients are graded III-IV according to the American Society of Anaesthesiologists, implying that they have significant co-morbidities [1]. The potential cardiovascular risks of acute blood loss and low Hb in this group mean that they often require blood transfusions to maintain hemodynamic stability. There are concerns, however, about the risks of immunological adverse reactions and disease transmission after allogenic blood transfusion [5].
Several techniques have been employed to minimize bleeding during TKA. These include the use of diathermy, tourniquets [6], local infusions of norepinephrine [7], minimally invasive surgery [8], antifibrinolytic agents [9], and sealing of the intramedullary canal after removal of the intramedullary jigs [10]. The position of the knee also influences blood loss as well as the use of low power suction drains [11], along with keeping these clamped for 4 h post surgery [12,13] (Table 2).
The current study has also demonstrated no significant difference in blood loss between our two groups when performed using the same surgical technique. There was no significant difference in postoperative limb alignment, drop in postoperative Hb, or transfusion requirements between the two groups. The tourniquet time was increased in the group B. While this was not statistically significant, it is in keeping with previous reports [14,15]. There also is no convincing evidence of significant clinical benefits in TKA thorough haemostasis by releasing the tourniquet during the operation. Added to this is a significant increase in operative time for navigated procedures. The results of this study suggest that with thorough haemostasis do not reduce blood loss during primary TKA. The results of this study suggest that if surgery is performed carefully and done well, the amount of bleeding is unaffected with or without thorough haemostasis techniques.
The main limitations of this study are that it is retrospective and nonrandomized. It does, however, present the results of a well matched consecutive series of patients from a nonspecialist center. We believe that these results are therefore relevant to the majority of practicing orthopedic surgeons. There is a need for a large multicenter prospective randomized controlled trial is to be performed before a consensus can be reached on the influence of blood loss during primary TKA.
In conclusion, our results suggest that there is no difference in the blood loss with or without haemostasis after the tourniquet released. However, haemostasis after the tourniquet released during the operation is necessary to reduce the blood loss for our patients. So we believe that with a thorough haemostasis during the operation is necessary and strongly recommend this procedure to all surgeons who are working with TKA patients.
This work was funded by National Science Foundation for Young Scholars of China (Grant No 81101362 and 81401784) and Key Project of National Natural Science Foundation of China (81330042). No benefits in any form have been or will be received from any commercial party related directly and indirectly to the subject of this manuscript.
The authors declare no conflict of interest.