Vein of Galen aneurysm is a rare vascular condition commonly diagnosed in children. This type of aneurysm arises from the persistence of the embryonic median prosencephalic vein, precursor to the Galen vein. This paper highlights the rarity of this phenomenon in a 40-year-old woman. The aim of this study is to demonstrate that conservative treatment of this malformation can be a valid option in oligosymptomatic cases without signs of hydrocephalus. While the literature emphasizes interventional procedures as the primary choice, especially arterial embolization, this case underscores the relevance of conservative treatment, particularly in neurologically stable patients.
Vein of Galen aneurysm, Congenital vascular malformation, Adult
Vein of Galen malformations represent unique congenital abnormalities among intracranial vascular malformations. They are considered rare, constituting ≤ 1% of intracranial vascular malformations [1]. The clinical spectrum varies widely depending on the timing of presentation. From birth to two months, high-output cardiac failure is the primary manifestation, while from two months to two years, hydrocephalus becomes prevalent. In older patients, symptoms such as headache, developmental delays, and headaches are described. This study presents a rare case in the literature, depicting an adult with an aneurysmal dilation of the Vein of Galen presenting with complaints of headache.
A. M. O., a 40-year-old woman, reports an 8-year history of headaches associated with dizziness. On neurological examination, she presents as alert, attentive, and oriented in both time and space, demonstrating coherence in speech and naming. Her mini-mental state examination scores 28 out of 30 (losing 2 points in calculation). Pupils are isochoric and react to light, with preserved extrinsic ocular motility and no abnormalities in cranial nerve pairs. Strength, coordination, and balance are all well-preserved.
A cranial magnetic resonance imaging (MRI) reveals a vascular lesion in the pineal gland region suggestive of an aneurysmal dilation of the Vein of Galen, measuring 1.8 × 2.5 × 1.8 cm (length × height × width). The lesion drains into the superior sagittal sinus through the falx cerebri, exhibiting no signs of thrombosis. It shows arteriovenous communication with branches originating from the bilateral posterior cerebral arteries (Figure 1). The cerebral parenchyma maintains its morphology and signal intensity, with a normopositioned and symmetrical ventricular system, conserving dimensions (Figure 2).
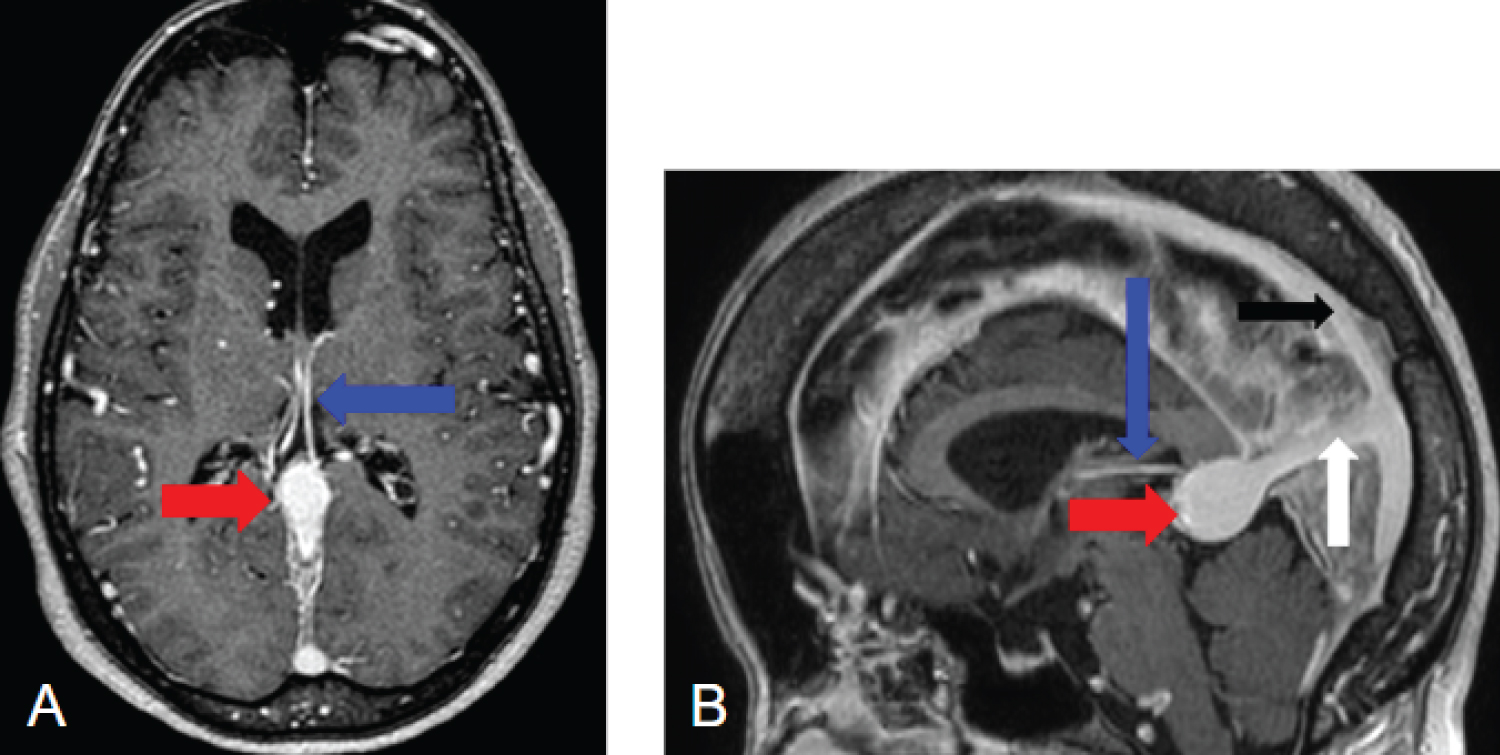 Figure 1: A) Cranial MRI in post-contrast T1-weighted images, axial section; B) Sagittal section demonstrating choroidal arteries branching from the posterior cerebral arteries (blue arrow), aneurysmal dilation of the Vein of Galen (red arrow), falx cerebri (white arrow), and superior sagittal sinus (black arrow).
View Figure 1
Figure 1: A) Cranial MRI in post-contrast T1-weighted images, axial section; B) Sagittal section demonstrating choroidal arteries branching from the posterior cerebral arteries (blue arrow), aneurysmal dilation of the Vein of Galen (red arrow), falx cerebri (white arrow), and superior sagittal sinus (black arrow).
View Figure 1
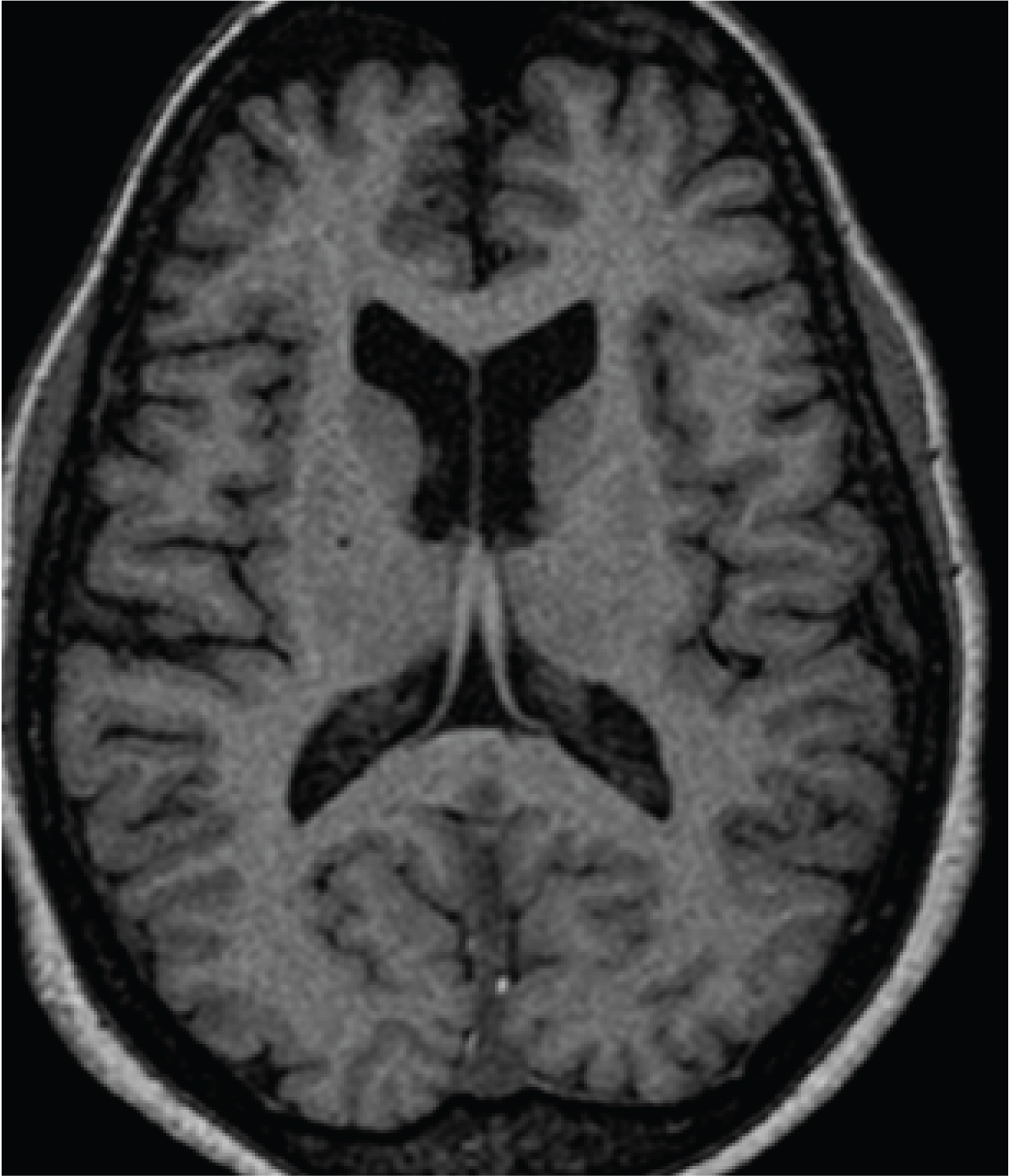 Figure 2: Cranial MRI in axial T1-weighted section displaying the ventricular system with preserved dimensions, and the cerebral parenchyma maintaining morphology and signal intensity without alterations.
View Figure 2
Figure 2: Cranial MRI in axial T1-weighted section displaying the ventricular system with preserved dimensions, and the cerebral parenchyma maintaining morphology and signal intensity without alterations.
View Figure 2
Cerebral angiography reveals a small cerebral arteriovenous shunt in the region of the Vein of Galen, with an aneurysmal dilation nourished by branches of the posterior cerebral arteries (Figure 3). Additionally, a fetal pattern of the right posterior cerebral artery is observed (Figure 4).
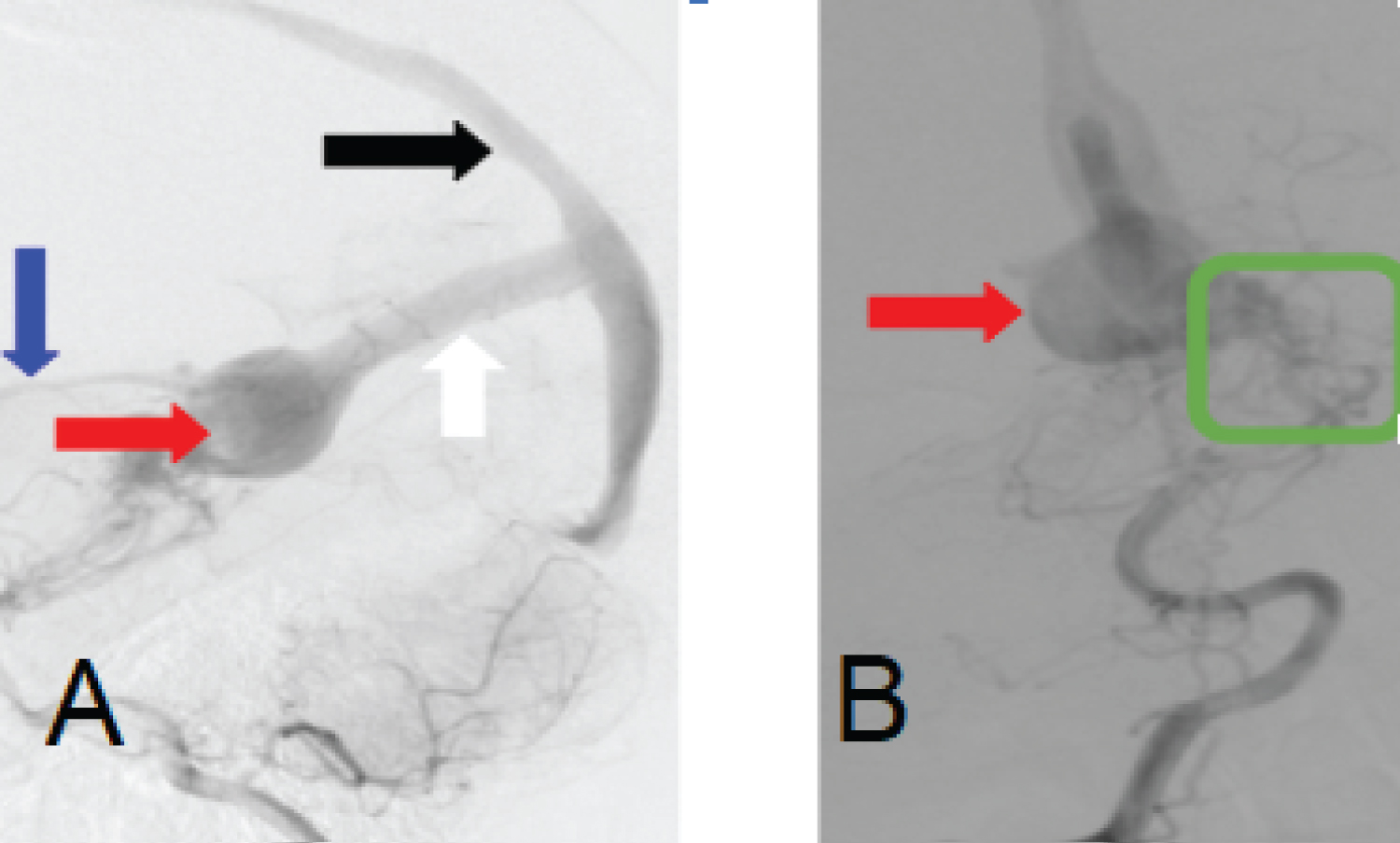 Figure 3: A) Right vertebral artery angiography in the arterial phase, lateral view; B) Anteroposterior view demonstrating: choroidal artery (blue arrow), aneurysmal dilation of the Vein of Galen (red arrow), superior sagittal sinus (white arrow), superior sagittal sinus (black arrow), and a fistulous connection of branches from the posterior cerebral artery with the anterolateral wall of the aneurysmal dilation of the Vein of Galen (green square).
View Figure 3
Figure 3: A) Right vertebral artery angiography in the arterial phase, lateral view; B) Anteroposterior view demonstrating: choroidal artery (blue arrow), aneurysmal dilation of the Vein of Galen (red arrow), superior sagittal sinus (white arrow), superior sagittal sinus (black arrow), and a fistulous connection of branches from the posterior cerebral artery with the anterolateral wall of the aneurysmal dilation of the Vein of Galen (green square).
View Figure 3
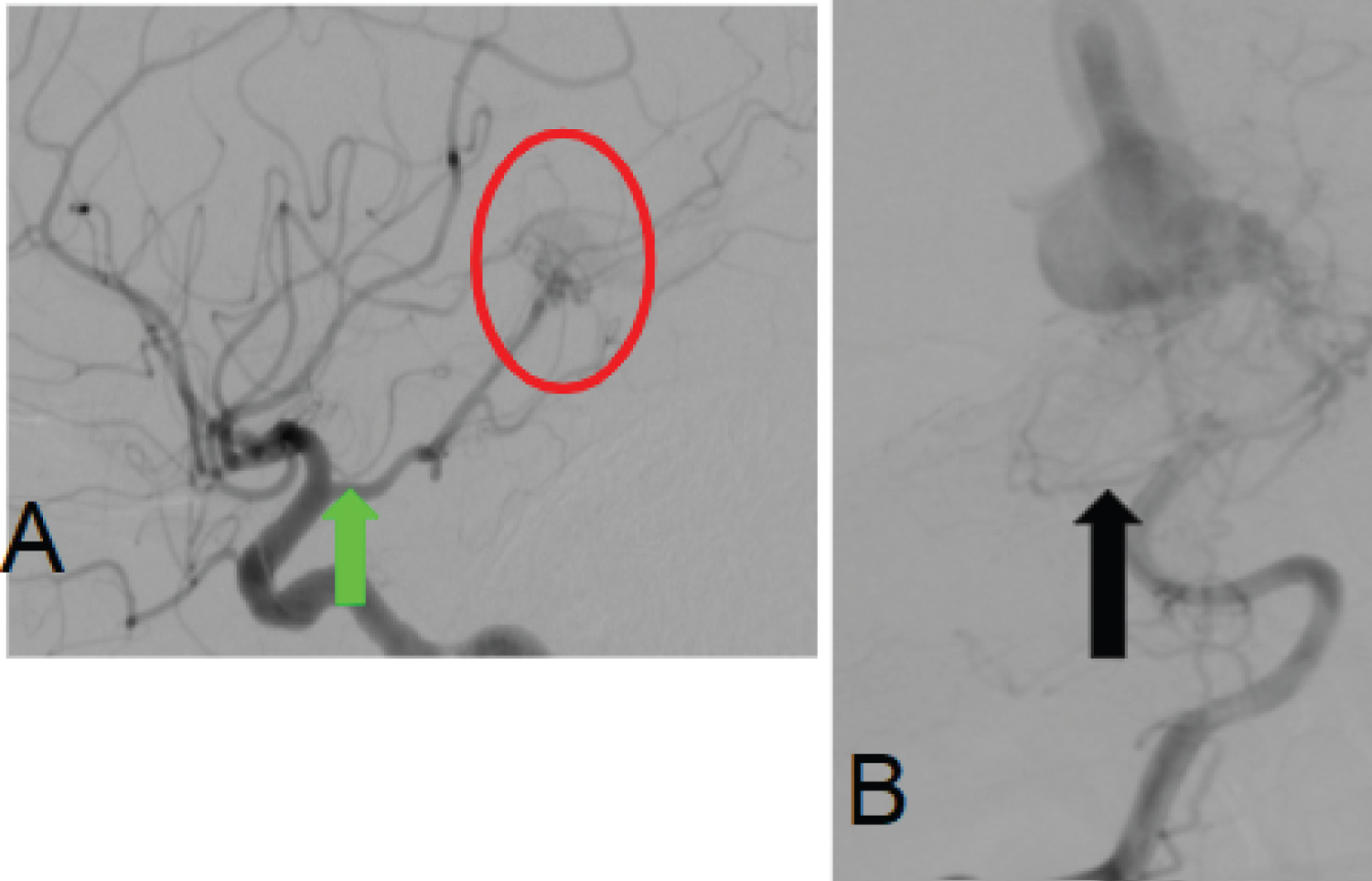 Figure 4: A) Profile view of an angiography of the right internal carotid artery showing a fetal posterior cerebral artery (PCA) (green arrow). In this case, the posterior communicating artery (P-com) has the same diameter as the PCA and appears to originate directly from the internal carotid artery (ICA). Fistulous connection of branches from the right PCA with an aneurysmal dilation of the Vein of Galen; B) Anteroposterior view of the right vertebral artery angiography in the same patient, demonstrating a hypoplastic P1 segment of the PCA (black arrow).
View Figure 4
Figure 4: A) Profile view of an angiography of the right internal carotid artery showing a fetal posterior cerebral artery (PCA) (green arrow). In this case, the posterior communicating artery (P-com) has the same diameter as the PCA and appears to originate directly from the internal carotid artery (ICA). Fistulous connection of branches from the right PCA with an aneurysmal dilation of the Vein of Galen; B) Anteroposterior view of the right vertebral artery angiography in the same patient, demonstrating a hypoplastic P1 segment of the PCA (black arrow).
View Figure 4
The aneurysmal dilation of the Vein of Galen results from the persistence of the median prosencephalic vein, which typically regresses between the fifth and seventh weeks of development. This persistence, along with its primitive arteriovenous connections, leads to a true malformation of the Vein of Galen, characterized by high flow and low resistance. Anatomically, it is a midline structure, with arterial supply through the choroidal arteries, a subependymal arterial network originating from the posterior circle of Willis, and rare branches from thalamoperforating arteries. Venous drainage occurs through the prosencephalic vein, which courses toward the falx cerebri and, at times, towards the superior sagittal sinus, with the straight sinus being absent in most cases [2-5].
The most commonly used classifications for this congenital vascular malformation are proposed by Yasargil [6] and Lasjaunias, et al. [7]. Yasargil [6] divides it into four types, with types 1, 2, and 3 representing direct fistulas between malformations and the Vein of Galen, while type 4 consists of parenchymal arteriovenous malformations that drain directly into the Vein of Galen. Lasjaunias, et al. [7] categorize it as mural and choroidal, with the choroidal type typically being more severe, characterized by an arterial network resembling a nidus, while the mural type has one or more arterial feeders connecting directly to the dilated median prosencephalic vein.
Vein of Galen malformation is typically diagnosed in the neonatal period, with signs of heart failure. The severity ranges from asymptomatic patients to multiple organ failure, depending on the Bicêtre classification [8]. Children between 2 months and 2 years, often with low-flow fistulous connections, may present with hydrocephalus or developmental delay.
In adults, descriptions of this occurrence are rare. Lasjaunias, et al. describes only one incidental case of this type of malformation in a series of 157 cases. Since the aneurysmal dilation of the Vein of Galen is exceptional, we lack sufficient information regarding its progression in adults [9]. The present study aligns with the literature, detailing a case of a 40-year-old female patient with headaches, whose diagnostic workup revealed an aneurysmal dilation of the Vein of Galen in cerebral angiography. This examination is considered the gold standard for diagnosing this vascular malformation. The management of this type of malformation is based on reports from small case series in the literature, given the rarity of the pathology.
Despite advances in interventional neuroradiology, which have ensured positive outcomes and are the preferred procedures in treatment, arterial embolization with n-butyl cyanoacrylate (nBCA) remains a favored option due to its resistance when compared to particles and coils [8]. However, conservative treatment should be considered, especially in asymptomatic, oligosymptomatic, and neurologically stable patients, as in the presented case [5]. In the context of the presented case, the choice for conservative treatment, based on the absence of hydrocephalus and neurological stability, contributes to the discussion about the variety of therapeutic options available.
Aneurysmal dilation of the Vein of Galen is extremely rare, with management based on small case series. The case presented, involving an adult diagnosed with VGAM, opted for conservative treatment and radiological follow-up, as the patient remained neurologically stable. This clinical case enriches the scientific literature by providing a comprehensive view of management and outcomes in patients of this age group. The discussion on the emerging role of interventional neuroradiology and the implications of conservative treatment serves as a valuable contribution to future research and clinical approaches.
Dantas Mageste Ferreira provided guidance at all stages of the research. Jéssica Aguilar da Silva, Vitor de Deus da Rocha Ribeiro Gonçalves and Lano de Sousa Moreira wrote the main manuscript text. Taianne Fiore Schumann made tables and prepared figures. All authors reviewed the manuscript.
The authors whose names are listed immediately below certify that they have NO affiliations with or involvement in any organization or entity with any financial interest, or non-financial interest in the subject matter or materials discussed in this case report. Author names: Dantas Mageste Ferreira, Lano Sousa Moreira, Taianne Fiore Schumann, Jéssica Aguilar da Silva, Vitor de Deus da Rocha Ribeiro Gonçalves.
None.