Deep brain stimulation, Mohr-tranebjaerg syndrome, Deafness-dystonia-optic neuronopathy syndrome, TIMM8A
Mohr-Tranebjaerg syndrome (MTS), also known as deafness-dystonia-optic neuronopathy syndrome is an X-linked recessive, progressive, and neurodegenerative disorder resulting from mutations in the nuclear-encoded deafness dystonia peptide 1 (DDP1)/translocase of mitochondrial inner membrane 8A ( TIMM8A ) gene. This genetic disorder was first described in 1996, when the deafness dystonia peptide (DDP) gene was identified in a family with deafness, dystonia, and cognitive decline [1].
MTS is characterized by sensorineural hearing loss, the usual feature in early childhood, followed by infancy onset progressive dystonia, ataxia, spasticity, cognitive impairment, psychiatric disease, and optic atrophy [2]. A combination of dystonia and sensory-neural deafness, referred to as dystonia-deafness syndrome (DDS), is a clinical presentation within the dystonia spectrum. DDS may have several genetic and acquired causes, but the etiology remains undetermined in most patients [3]. Here, we report a genetically confirmed case of MTS presenting with progressive generalized dystonia, deafness, and cognitive and behavioral abnormalities that were treated by internal globus pallidus (GPi) deep brain stimulation (DBS).
A 41-year-old man presented with sensory-neural deafness since the age of 18 months, followed by progressive generalized dystonia and cognitive and behavioral impairments. During childhood, he had shown language delay development and motor symptoms characterized by dystonia in the lower limbs, with short steps. Despite optimal pharmacological and non-pharmacological treatment, he presented with gradual dystonia worsening of the gait and upper limbs, cervical, and face (Video 1). Additionally, he presented with impaired cognitive and behavioral function after the third decade of life. Visual evoked potential detected impairment in both eyes.
Brain magnetic resonance imaging (Figure 1) demonstrated atrophy of the head of caudate nuclei and abnormal iron deposition in the nigra substance and globus pallidus. MTS was genetically confirmed by identifying hemizygosis in the TIMM8A gene (ChrX variant 100.603.526) (Translocase of Inner Mitochondrial Membrane 8, Yeast, Homolog of, OMIM*300356) through exome sequencing. There is not reported family history of neurological disease.
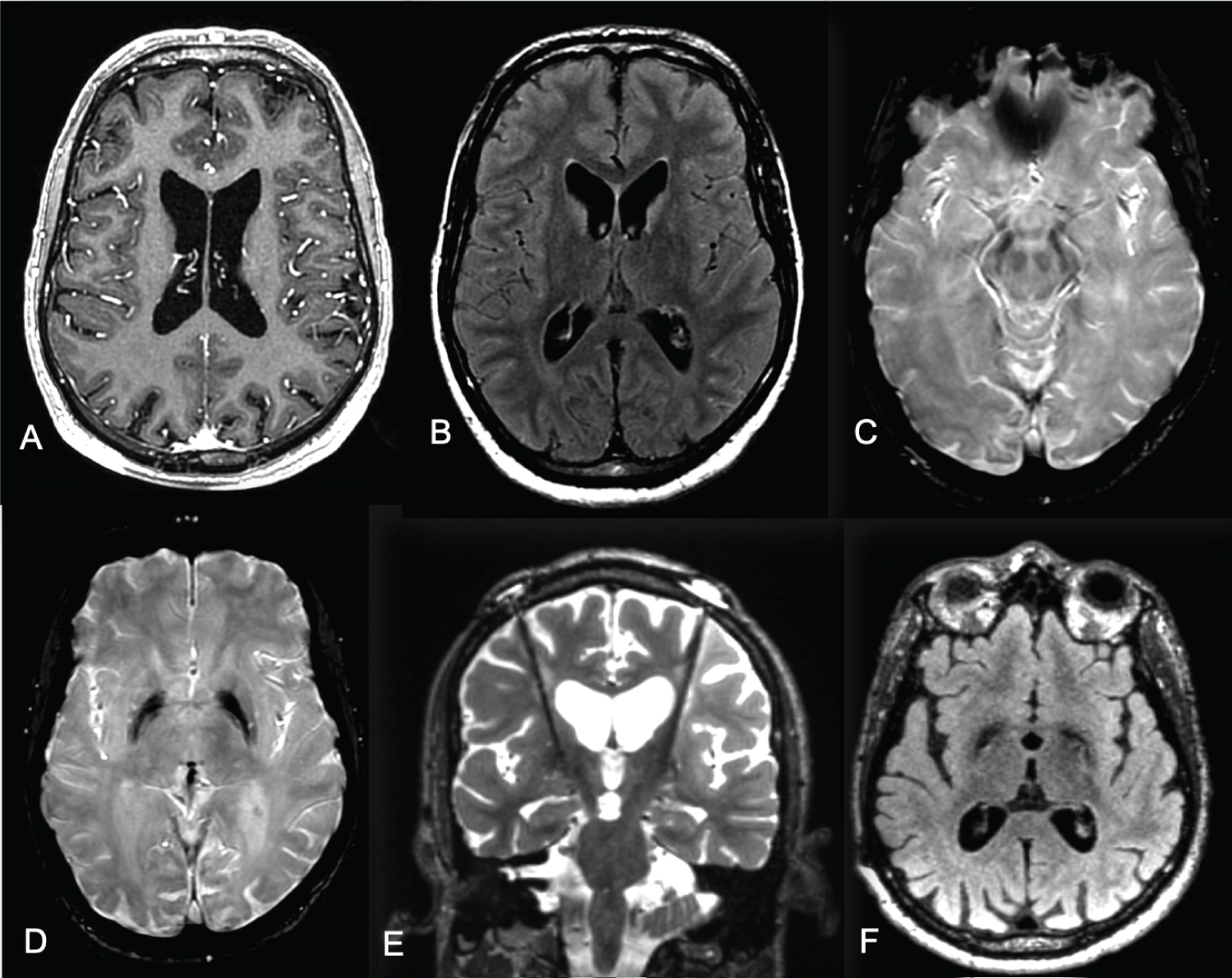 Figure 1: Brain MRI in axial T1 (A), axial FLAIR (B) and axial SWI (C and D) sequences showing brain atrophy more evident of the parietal lobes, atrophy of the head of caudate nuclei with abnormal iron deposition in the nigra substance and globus pallidus. Brain MRI coronal T2 (E) and axial FLAIR sequences (F) with deep brain stimulation electrodes at globus pallidus internus.
View Figure 1
Figure 1: Brain MRI in axial T1 (A), axial FLAIR (B) and axial SWI (C and D) sequences showing brain atrophy more evident of the parietal lobes, atrophy of the head of caudate nuclei with abnormal iron deposition in the nigra substance and globus pallidus. Brain MRI coronal T2 (E) and axial FLAIR sequences (F) with deep brain stimulation electrodes at globus pallidus internus.
View Figure 1
Pharmacological treatment with levodopa, trihexyphenidyl, baclofen, clozapine and clonazepam had limited effect. Botulinum toxin injections resulted in only a partial reduction of blepharospasm, cervical dystonia, and pain. After treatment failure, we decided to perform GPi DBS.
DBS GPI was performed with stereotaxic computed tomography guidance under general anesthesia. Electrophysiology was used to identify the target regions and guide DBS electrode placement. There was no evidence of microlesion effect due to electrode insertion during the postoperative period, and the maximum DBS benefit occurred 6 months post-surgery. Brain MRI (Figure 1) represents the postoperative imaging of Gpi DBS electrode localization.
Final stimulation settings were: left GPi channel 0-1+, 3.0V, 90 μs, 130 Hz; right GPi channel 8-9+, 3.0V, 90 μs, 130 Hz.
At preoperative assessment, the Burke-Fahn-Marsden Dystonia Rating Scale (BFMDRS) total score was 24 for disability and 100 for dystonia movement. After 2 years follow-up, he had a BFMDRS score of 24 for disability and 68 for dystonia movement (Table 1). Therefore, after the 2-year follow-up, he showed a 32% greater improvement in the cervical region and upper limbs on the dystonic movement scale.
Table 1: Preoperative and after 2 years follow-up Burke-Fahn-Marsden dystonia rating scale score. View Table 1
Complex hereditary dystonia includes the Mohr-Tranebjaerg syndrome, an X-linked disease caused by mutations in the TIMM8A gene. The disease is characterized by sensorineural hearing loss in early childhood and generalized dystonia in adolescence with predominantly orofacial and cervical distribution; it can also progress to pyramidal signs, optic atrophy, psychiatric disturbances, and cognitive decline.
Our case patient experienced improvement of cervical and limbs dystonia, which remained stable during the 2-years outcomes. Besides that, there was a significant improvement in chronic pain in the limbs. Unfortunately, we could not observe changes in the patient's gait (Video 2). Another interesting aspect in our report was the presence of abnormal iron deposition in the globus pallidus, similar to diseases in the neurodegeneration with brain iron accumulation spectrum.
There are a few cases reported on DBS in MTS. Havránková, et al. described the first dystonia-deafness syndrome successfully treated by GPi DBS. The antidystonic effect of GPi DBS gradually occurred over a course of several months and maximum improvement was expressed by a 75% decrease in motor scores of the BFMDS [4].
Cif, et al., reported a genetically confirmed MTS patient who presented progressive generalized dystonia, deafness, and mild cognitive and behavioral abnormalities successfully treated by GPi DBS with significant improvement at 1-year follow-up [5].
Our case is in line with those discussed previously, showing a significant effect on cervical control and slight improvement in mouth dystonia.
One recent study showed successful implantation and management of a bilateral GPi DBS system in patients with bilateral cochlear implants. Most of the dystonic symptoms improved. Post-operation, there was a remarkable improvement in the orofacial dystonia, and score on BFMDRS showed 82% improvement at 2 years [6].
We reported successful implantation and management of a bilateral GPi DBS system in an MTS patient. Overall, improvements of dystonic symptoms were maintained at a 2-year-follow-up. GPi DBS can be considered in severe disabling dystonia in MTS. Further research with a series of patients is needed to confirm these findings.
All authors have read and complied with the Journal’s Ethical Publication Guidelines. “We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this work is consistent with those guidelines.” Patient gave written informed consent to print and online publication. Local ethics committee per guidelines does not need to approve single case reports; only the informed consent of the patient is necessary.
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for the previous 12 months: The authors declare that there are no specific financial disclosures to declare for the previous 12 months.
We thank the patient and her family for cooperating in the publication of this material and providing written informed consent.
A video accompanying this article is available in the supporting information here.
Video 1: Preoperative assessment of dystonia shows marked generalized dystonia.
Video 2: Patient with the stimulator turned on showing improvement in generalizes dystonia follow-up of 24 months after DBS.