Neurosarcoidosis is a rare manifestation of sarcoidosis, comprising 5-15% of cases. We present a case of a 44-year-old man with no prior medical history who experienced two episodes of diffuse tonic-clonic seizures. Imaging showed a dural-based lesion with evidence of brain parenchymal involvement, suggestive of an aggressive, atypical meningioma with brain invasion. He underwent resection and recovered well; histopathological assessment and tissue diagnosis demonstrated perivascular granulomatous inflammation with negative markers for mycobacterium, suggestive of neurosarcoidosis. The non-specific presentation of neurosarcoidosis, with radiographic features that can resemble high grade meningioma and histopathological features that can resemble mycoplasma, can portray an unclear clinical picture. Thus, we highlight neurosarcoidosis as an important differential when dural-based lesions with CNS involvement are discovered on imaging.
Neurosarcoidosis, Sarcoidosis, Meningioma, Dural-based lesion
AFB: Acid Fast Bacillus; CD 3, 20, 68: Cluster of differentiation; CMV: Cytomegalovirus; CNS: Central Nervous System; CT: Computed Tomography; EMA: Epithelial Membrane Antigen; GMS: Grocott Methenamine Silver; HSV: Herpes Simplex Virus; IHC: Immunohistochemistry; IV: Intravenous; MRI: Magnetic Resonance Imaging; PR: Progesterone Receptor; SSTR2: Somatostatin Receptor 2
Sarcoidosis is a systemic inflammatory disease of unclear etiology characterized by noncaseating granulomas in various organ systems [1]. Pulmonary, cutaneous, and lymphatic involvement are most common; however, estimates suggest neurological involvement in 5-15% of patients diagnosed with systemic Sarcoidosis [2]. Iwai, et al. found that an antemortem diagnosis of sarcoidosis was made in only 50% of autopsy-verified cases of neurosarcoidosis [3]. Neurosarcoidosis is often suspected when a patient with systemic sarcoidosis develops neurological symptoms; however, in some rare cases, patients have been diagnosed with isolated neurosarcoidosis [4]. In these circumstances, the non-specific neurological symptoms that patients may or may not present with and radiologic resemblance to other CNS (central nervous system) growths such as meningioma can lead to misdiagnosis. Previous reports have identified instances of neurosarcoidosis mimicking meningioma [5]. We present the following rare case of isolated dural-based neurosarcoidosis with extensive CNS parenchymal involvement radiographically mimicking atypical meningioma with brain invasion, in a patient without systemic manifestations of sarcoidosis.
A 44-year-old man with no significant prior medical history and taking no medications presented to the emergency department in the early morning after two episodes of a new onset seizure. Around midnight, he had a diffuse, tonic-clonic seizure with foaming of the mouth lasting 2-3 minutes that spontaneously resolved. The patient felt tired after the episode and resumed sleep, but had another similar 2-3 minute seizure episode several hours later. Emergency medical services were subsequently called. The patient had some right shoulder pain but denied recollection of the seizures, incontinence, tongue injury, and headaches. Further, he denied, fevers, nausea, vomiting, recent illness, loss of appetite, unintentional weight changes, and family history of malignancy. He endorsed recent travel to India. Upon neurological exam, the patient had pain in the right upper and lower extremities due to trauma from the seizure, but cranial nerves were grossly intact and the patient had no focal deficits. Laboratory studies showed a mild leukocytosis. Otherwise, they were unremarkable with no hypercalcemia.
Axial non-contrast head computed tomography (CT) showed a slightly hyperdense dural-based mass in the right frontal cortex measuring 19 mm in maximal dimension with adjacent vasogenic edema in the right frontal lobe causing regional sulcal and right lateral ventricular effacement without midline shift-suggestive of possible meningioma. Chest, abdomen, and pelvis CT with contrast were negative for primary sites. Head magnetic resonance imaging (MRI) with IV (intravenous) gadolinium contrast with coronal imaging through temporal lobes was obtained. Post-gadolinium enhancement, the mass measured 20 × 24 × 20 mm in maximal dimension (Figure 1). Peripherally, the mass appeared to have a broad dural-base; however, it was more representative of an eccentrically located intra-axial lesion with isolated enhancing foci-suggestive of brain invasion. There was leptomeningeal enhancement in the adjacent frontal sulci, with vasogenic edema contributing to regional sulcal effacement and mild effacement of the frontal horn of the right lateral ventricle, without midline shift. The vasogenic edema extended into the right lateral aspect of the genu of the corpus callosum. Imaging findings were suggestive of a meningioma, with differential diagnoses including atypical meningioma with brain invasion, infectious etiology, and lymphoma.
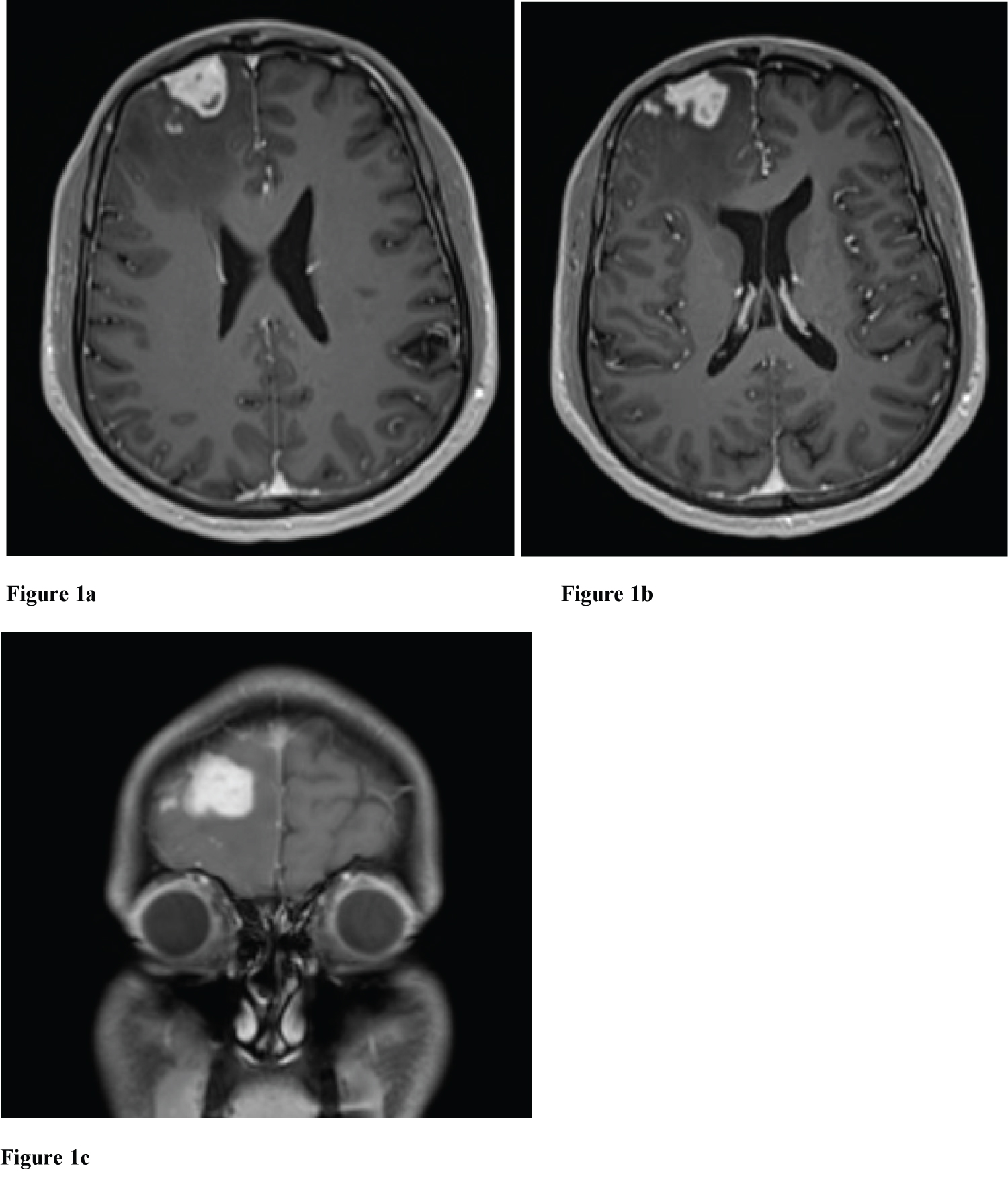 Figure 1: (a-c) Radiology. Axial T1 MRI (a-b) and Coronal T1 MRI (c) with contrast demonstrating an enhanced dural-based mass in the right frontal cortex with adjacent vasogenic edema. Of note, isolated foci with enhancement are seen within the brain parenchyma. There is protrusion of the mass lesion, which further suggests brain invasion.
View Figure 1
Figure 1: (a-c) Radiology. Axial T1 MRI (a-b) and Coronal T1 MRI (c) with contrast demonstrating an enhanced dural-based mass in the right frontal cortex with adjacent vasogenic edema. Of note, isolated foci with enhancement are seen within the brain parenchyma. There is protrusion of the mass lesion, which further suggests brain invasion.
View Figure 1
The patient underwent craniotomy for tissue diagnosis and resection of mass. A three-quarters coronal plane incision was planned and executed for access to the relatively low, right frontal position of the tumor. The lesion was grossly extra-axial with dense attachments to the frontal dura. This was sharply dissected away from the nearby normal dura and from the pial surface of the brain. The attached portion of the dura was sharply removed. This process was continued until the tumor was removed en bloc entirely. Grossly, the tumor had a dense, fibrous, and rubbery consistency.
Post-operative MRI with contrast showed gross total resection of the mass lesion with persistent vasogenic edema and residual remote leptomeningeal enhancement. The patient recovered well and was discharged; he has been asymptomatic to date. MRI on long term follow up shows no evidence of recurrence and stable leptomeningeal enhancement.
Histology revealed a dural-based mass lesion with extensive necrosis characterized by multiple nodules of granulomas containing multinucleated giant cells, with associated reactive lymphocytic inflammation exhibiting mixed populations of CD20 positive B-cells and CD3-positive T-cells. The lesional cells also appeared to infiltrate into the adjacent CNS tissue, predominantly associated with perivascular spaces. Immunohistochemistry (IHC) results were positive for histiocytic marker (CD68) in the lesional cells. Other IHC results were essentially negative for markers for meningioma; EMA (epithelial membrane antigen), PR (progesterone receptor), SSTR2 (somatostatin receptor 2), cytokeratin markers, mesenchymal markers, and other markers for CNS neoplasms. Lastly, results for microorganisms were negative for mycobacterial (AFB; acid fast bacilli), fungal (GMS; Grocott Methenamine Silver), bacterial (Gram) organisms. CMV (Cytomegalovirus), and HSV (Herpes Simplex Virus) 1&2 were negative by IHC. In addition, the specimen was sent for molecular study with genetic sequencing, which came back as negative for mycobacterial species (Figure 2).
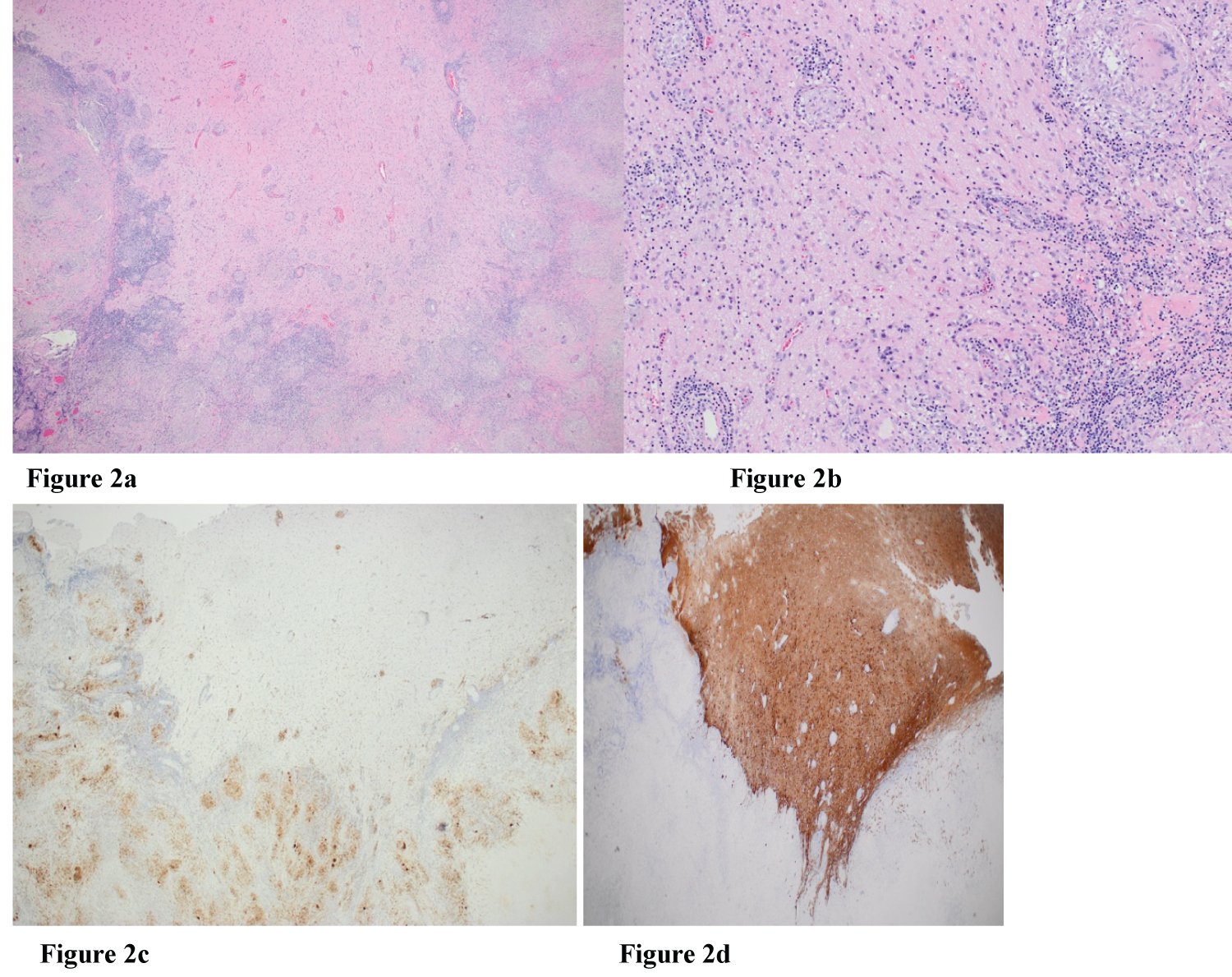 Figure 2: (a-d) Pathology. Low power view at 20x magnification (2a) shows interfacing between the lesion and adjacent brain parenchyma. Multiple nodules with giant cell formation of granuloma are recognized. On high power view at 200x magnification (2b), small foci of granulomatous inflammation are identified in the perivascular space of cortical blood vessels. Immunohistochemistry (IHC) for macrophage marker (CD 68) highlights multifocal granuloma (2c). Adjacent brain parenchyma exhibits reactive astrogliosis at the interface with granuloma (2d).
View Figure 2
Figure 2: (a-d) Pathology. Low power view at 20x magnification (2a) shows interfacing between the lesion and adjacent brain parenchyma. Multiple nodules with giant cell formation of granuloma are recognized. On high power view at 200x magnification (2b), small foci of granulomatous inflammation are identified in the perivascular space of cortical blood vessels. Immunohistochemistry (IHC) for macrophage marker (CD 68) highlights multifocal granuloma (2c). Adjacent brain parenchyma exhibits reactive astrogliosis at the interface with granuloma (2d).
View Figure 2
The incidence of sarcoidosis is relatively low, with estimates of 5-40 cases per 100,000 with significant geographic variability, worldwide [6]. Within the United States, sarcoidosis has a greater incidence, chronicity and mortality among Black Americans than White Americans [6]. Across racial and ethnic groups, the prevalence of sarcoidosis is greater among women than men [6]. Neurosarcoidosis comprises 5-15% of sarcoidosis cases, which typically manifests as a part of systemic sarcoidosis.
Clinical presentations of neurosarcoidosis are non-specific, as they depend on the intracranial location of the lesion. Intra-axial neurosarcoid lesions can involve the CNS parenchyma, whereas extra-axial lesions can involve leptomeningeal spaces. This patient experienced two seizure episodes in absence of other neurological and systemic symptoms-including those that would suggest infectious etiology.
Imaging studies demonstrated a solitary dural-based mass; the differential includes meningioma, dural metastatic diseases or other rare entities of mesenchymal neoplasms arising in the leptomeningeal spaces for neoplastic processes. Differential diagnoses of non-neoplastic processes include infectious etiologies such as mycobacterial and fungal organisms, and non-infectious etiologies such as granulomatosis with polyangiitis or sarcoidosis. Diagnosis is difficult due to non-specific symptoms and low radiographic specificity.
Neurosarcoid lesions radiographically mimicking a meningioma have been described in a number of reports [4,5,7-14]. This case further underscores the difficulty of diagnosis radiographically, due to the additional finding of intraparenchymal involvement. The radiographic findings of this case were concerning for a meningioma with brain invasion, which is one of the key pathological features of a WHO Grade 2 atypical meningioma. CNS parenchymal and leptomeningeal involvement in neurosarcoidosis have also been described in the literature.
Radiographic findings however, are insufficient for definitive diagnosis. Evidence of granulomatous inflammation on histopathology suggests a differential diagnosis of neurosarcoidosis and infectious etiologies, especially mycobacterial species, and excludes meningioma. In this case, the special stains for microorganisms including mycobacteria were negative. Additionally, molecular study with mycobacterial species sequencing was negative, further supporting neurosarcoidosis as the principle diagnosis.
Due to the presence of a large intracranial mass lesion with associated seizure episodes, surgical excision of the lesion with histopathological assessment and tissue diagnosis were the appropriate interventions. It is important to note that pre-operative radiological findings were concerning for brain invasion by a meningioma, which would have necessitated adjuvant radiation therapy.
Neurosarcoidosis is a rare disease; the patient’s clinical presentation and laboratory results were inconsistent with neurosarcoidosis. Thus, as demonstrated in this case-it is important to raise awareness of this entity which mimics meningioma with worrisome features of biologically aggressive subtypes such as atypical meningioma with brain invasion.
None.