Vascular neurosurgery has been established through an on-site fellowship programme in Cameroon. With a less technically sophisticated basic equipment, high quality surgeries with good outcomes could still reached. We present two cases of big cavernous-segment aneurysms treated by distal ICA-occlusion in an awake surgery. To our knowledge these are the first awake neurosurgical procedures in Cameroon.
Two patients with symptomatic big aneurysms of the cavernous ICA were treated. The treatment was performed by two time surgeries. In the first surgery (general anesthesia), we dissected the ICA and identified the ophthalmic- and the pcom artery, as well as the position of the ICA clip occlusion. In a second surgery (local anaesthetised and not sedated), we approached immediately the dissected ICA and occluded the ICA distal to the aneurysm. The patients were asked to move the limbs every 60 seconds and the sight was tested. Postoperative CTA showed a thrombosed ICA and aneurysm, an excellent collateral perfusion and both patients were in an excellent clinical condition.
In limited resource environments with no ICG, neurophysiology or microdoppler, awake clip occlusion, distal to an aneurysm is the procedure of choice. Since the patient is not sedated, the ICA is dissected in a first surgery under general anesthesia. Manipulation of the intracranial vessels in a non sedated patient is painful and leads to increase of ICP, therefore dissection of the ICA should not be performed in an unseated awake patient with a brain aneurysm.
Awake vascular neurosurgery, Clip occlusion, Internal carotid artery occlusion, Brain aneurysm, Africa, Limited resources environments
AVF: Arteriovenous Fistula; AVM: Arteriovenous Malformation; CNS: Central Nervous System; Cct: Cranial Computed Tomography; CTA: Computed Tomographic Angiography; ICP: Intracerebral Pressure; Pcom: Posterior Communicating Artery; ICA: Internal Carotid Artery; ECA: External Carotid Artery; MCA: Medial Carotid Artery; ACA: Anterior Carotid Artery; ICG: Indicyanine Green Angiography
A vascular neurosurgery on-site fellowship program has been developed in Yaounde General Hospital, in order to train the local neurosurgeons in microsurgical treatment of CNS vascular pathologies. At the moment more than 40 cases have been treated. Forty brain aneurysms, one pediatric spinal AVF and one AVM of the lateral ventricle. Only the locally available equipment has been used with some added equipment ordered and organised by the last author, who is directing the program. During the treated cases improvisations and treatment strategies have to be chosen under the limits of the given circumstances (i.e. no neurophysiological monitoring, no ICG or intraoperative microdoppler). We present two cases of big cavernous-segment-ICA aneurysms treated by distal ICA-occlusion under awake surgery.
The first case is a 32-years-old male patient presented to the outpatient clinic 2 months before surgery with progressive diplopia. A partially thrombosed 2 cm aneurysm of the right ICA was identified (Figure 1a). Through a pterional craniotomy the ICA on the right side was inspected and dissected under general anesthesia (Video 1). The aneurysm was extraduraly and was pushing the dura upwards. The ICA immediately proximal to the ophthalmic artery was ectatic. After dissecting the ICA we applied a temporary clip distal of the ophthalmic artery and inspected the ICA filing distal of the clip. No vascular collapse could be seen. Still we decided against an ICA occlusion and planed the occlusion in a second, awake surgery. The patient was informed about the second surgery, which would be in a fully awake state and consented. In the second surgery following 3 days after the first, the already dissected ICA, was approached (under local anesthesia and no sedation) and clip-occlusion was performed between the ophthalmic and pcom arteries (Video 2). The ophthalmic artery was occluded with a second clip to exclude aneurysm filling from the ECA circulation. Immediately after the clip application the patient was asked to move his left and right extremities every 60 seconds until the wound was closed (Video 3). We also asked him of any changes of his sight. After skin-closure the patient stayed one night in the ICU and after cCT and CTA he was transported to the ward and was discharged 5 days after occlusion. The double vision persisted, but as could be seen in the CTA (Figure 1b) the aneurysm and the ICA proximal to the clip were completely thrombosed. Distal to the clip a regular, ICA flow could be seen (Figure 1c).
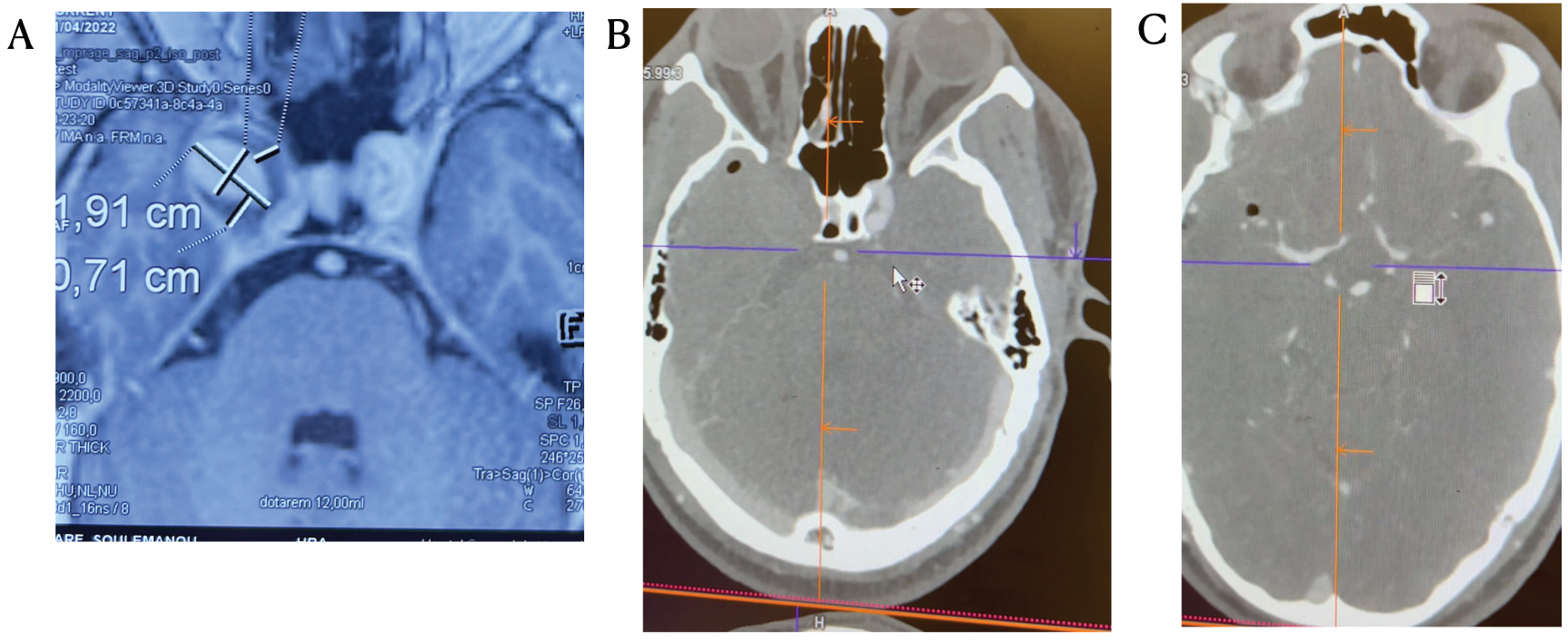 Figure 1: (A) Right ICA aneurysm of the cavernous sinus causing diplopia; (B) Postoperative CTA showing a completely thrombosed aneurysm and ICA on the right side; (C) The ICA and intracerebral circulation distal of the clip is completely intact as can be seen on the MCA and ACA the right side.
View Figure 1
Figure 1: (A) Right ICA aneurysm of the cavernous sinus causing diplopia; (B) Postoperative CTA showing a completely thrombosed aneurysm and ICA on the right side; (C) The ICA and intracerebral circulation distal of the clip is completely intact as can be seen on the MCA and ACA the right side.
View Figure 1
Video 1: First surgery under general anesthesiato dissect the ICA and prepare the region in which the clip for permanent ICA occlusion will be applied. Since the patient is not put under sedation in the second, awake neurosurgery "manipulation and dissection of the vessel would put the patient under high stress and pain levels which could even lead to premature ending of the procedure. Also the ICP is raining under painful condition making surgical manipulation around the vessel difficult.
Video 2: Awake neurosurgery without sedation. During contact with the ICA the patient is pressing and as can be heard under pain. The time of contact with the already dissected ICA from a surgery few days ago is kept to a minimum (exactly the time seen on the video).
Video 3: Immediately after clip occlusion of the right ICA the patient is asked to move his left arm, left leg, right arm, right leg in 60 sec. Time intervals until the skin is sutured. He was also asked if he has any visual disturbance since the ophthalmic artery was also occluded by a second clip to prevent any flow from the ECA to the aneurysm.
Video 4: Postsurgical CTA of the second case. The sound is kept since the CTA was discussed by the senior author with fellows and residents of the neurosurgical department. Therefore an impression of the educational aspect of the vascular neurosurgery program in Yaounde general Hospital can be given.
The second case is a 60-years-old female patient with double vision and headaches for the last 6 months. The cerebral CTA scan showed a giant 3 cm aneurysm of the left cavernous segment ICA (Figure 2). In the same fashion as in the first case we dissected the ICA in a surgery under general anesthesia. Three days after the first surgery we occluded the ICA distally to the aneurysm in the segment proximal to the ophthalmic artery in an awake surgery under local anesthesia. The postoperative cranial CTA shows again a complete thrombosis of the aneurysm and the regular signal of all arteries distal to the clip (Video 4).
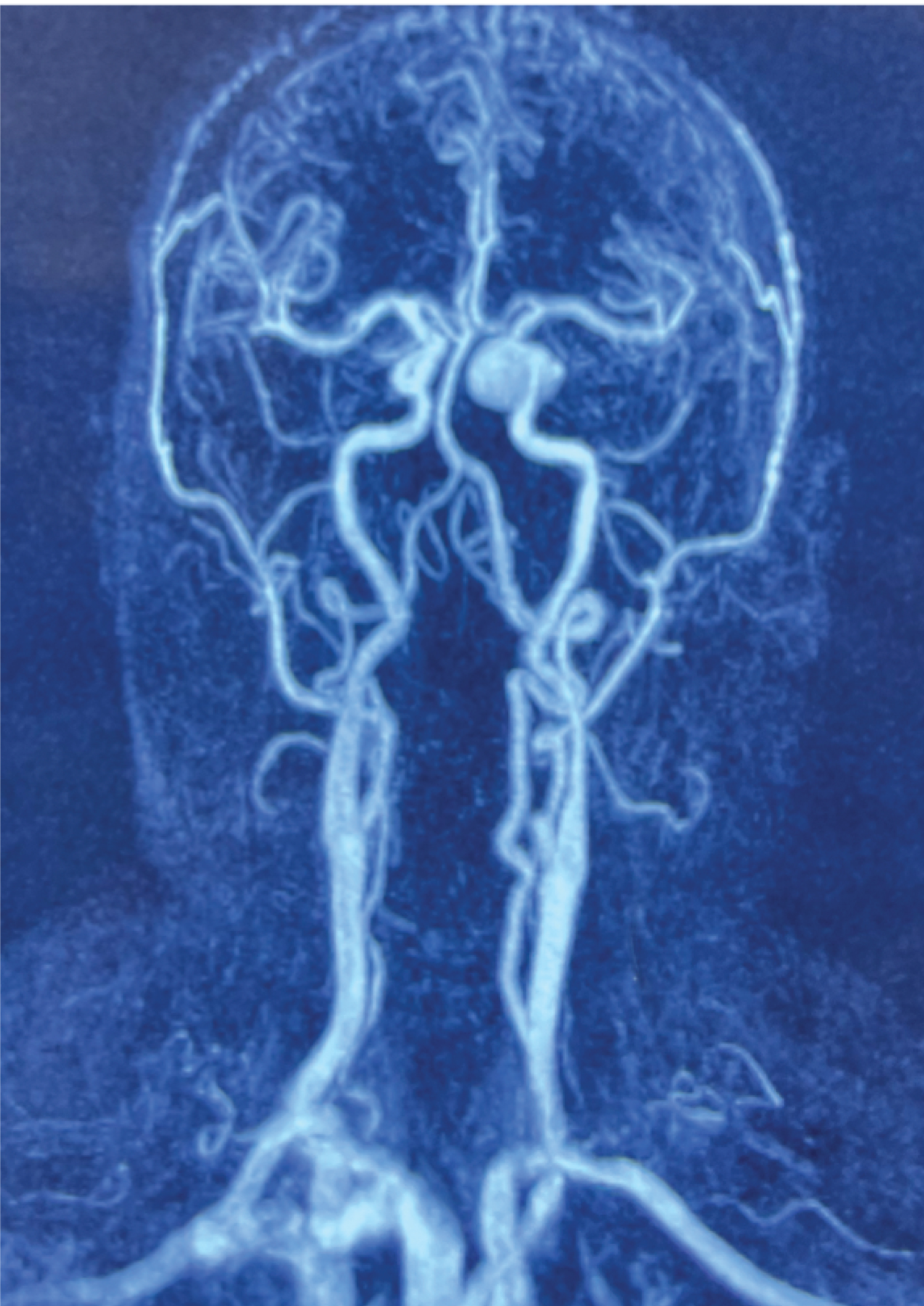 Figure 2: Intracavernous left giant ICA aneurysm. The ICA was occluded distal to the aneurysm in an awake surgery.
View Figure 2
Figure 2: Intracavernous left giant ICA aneurysm. The ICA was occluded distal to the aneurysm in an awake surgery.
View Figure 2
In the present two cases we stood in front of an operative dilemma. We had big symptomatic ICA aneurysms which required treatment. Endovascular treatment was not an option, since it was not available. Distal ICA occlusion with aneurysm thrombosis the only feasible option. However, a reliable method of occluding the ICA without causing an ischemia had to be chosen. Neurophysiology was not available. The best treatment option was dissecting the ICA in a first surgery in global anaesthesia and occlude the ICA in an awake second surgery. The patient was not sedated in the second surgery, therefore the surgery time was kept under 60 min and there was a short time of pain when the ICA was manipulated and the clip was placed. Another option would be to perform an asleep-awake surgery instead of two different surgeries, which was not feasible because of inexperience with such procedures. Awake aneurysm surgery was reported by Abdulrauf, et al, in which the patients were prevented from permanent ischemia during clipping procedures [1].
Proximal occlusion control by compressing the ICA in the patient's neck would not be reliable enough to allow us to proceed with permanent ICA occlusion under general anesthesia, therefore we omitted this manoeuvre. Awake neurosurgery in African countries are reported and mostly used in glioma and epilepsy surgery [2]. Reason for awake neurosurgery were lesions close to eloquent areas, which required more equipment and sophistication compared to the ICA occlusion we have done in the present cases. Neurophysiology, neuronavigation, brain-mapping, required in brain tumor surgery was not needed in vascular occlusion, making our procedure independent from multidisciplinary teams [2]. What is absolutely necessary though, are in-person visits and internet based consultations. We have established a high quality care of patients with vascular pathologies of the CNS through our on-site fellowship program. The locally trained neurosurgeons are now able to treat satisfactorily the majority of aneurysm cases. Patients in some African countries are extremely reluctant of having a brain surgery, mainly based on cultural and economical reasons [2].
To proceed with an awake surgery the patient has to overcome his/her fears, and since sedation was not used the patient has to be extremely collaborative. To achieve this aim and overcome cultural boundaries a relationship of trust has to be established between doctor and patient, as well as the patient's relatives. The one and only information source of the patient is the treating physician (no google, no wikipedia etc.). Since ICG angiography or microdoppler are not available, arterial occlusion is only feasible with an awake surgery, especially when a bypass is not performed. Awake vascular neurosurgery in Africa is not just another option of treatment, but the only one. With time, the senior author has also learned to rely on visual and tactile senses of arterial perfusion after clipping, which is highly needed in an environment where intraoperative tools (ICG, microdopppler) are not available.
The main limitation of ICA occlusion in limited resources environments is the lack of ICG angiography, microdoppler and very limited resources for a bypass procedure. Cultural limitations, which need to be overcome can be also problematic for the patients decision to allow brain surgery. A multidisciplinary team (speech therapist, neuropsychologist) to examine higher brain functions was not available, therefore awake neurosurgery in brain tumors , would need a different setting as the one described here.
In cases were technology is insufficiently and an aneurysm has to be treated by arterial ocllusion, awake surgery is the only feasible option. We describe two cases of big symptomatic carotid artery aneurysms needed distal ICA occlusion. The postoperative outcome was excellent and the aneursysms completely thrombosed. It is also important to dissect the area around the vessel in a first surgery under general anesthesia, since manipulating the vessel in awake neurosurgery is causing pain, leading to increased ICP during the occlusion. The time of contact with the vessel in an awake, non sedated patient has to be limited for only some seconds.
Not applicable.
None.
AKP wrote the manuscript and performed the surgeries. All author authors corrected the manuscript and are responsible for surgical planing and organisation.
Brainglobal sponsored microinstruments and aneurysm clips.
Datasets are records on the corresponding authors camera. The movie clips are originals.
The vascular neurosurgery program of Yaounde General Hospital is partially funded by Brainglobal non-profit organisation. The authors have no conflict of interest.