Extracranial internal carotid carotid aneurysms are rare, surgical treatment is complex if they are at the high cervical level and if the artery is tortuous. We present the case of a patient with an upper cervical internal carotid aneurysm (ICA), treated by high-flow bypass surgery, using a radial artery (RA) graft between the external carotid artery (ACE) and the middle cerebral artery (MCA).
A 60-year-old female patient with an upper, pulsatile and painful right cervical tumor diagnosed as a cervical aneurysm of the C1 segment of the internal carotid is decided by surgical treatment by high-flow bypass between the cervical external carotid and the M2 segment of the middle cerebral and closure of the cervical ACI. Patient in the postoperative period presents good evolution.
Closure of the ICA after a high-flow bypass with RA graft is a technically complex but safe procedure in the treatment of large, tortuous and high-cervical ACI extracranial aneurysms.
Cerebral revascularization, Extracranial carotid aneurysm, High flow bypass, Radial artery graft
Extracranial carotid artery aneurysms are rare, constituting approximately 0.3% of all extracranial aneurysms. The presentation of a giant, tortuous aneurysm represents a rare variation of this pathology [1]. Its rupture rate is low, however, morbidity and mortality rates associated with thromboembolism are high, so definitive treatment is recommended [2-4]. Without treatment, about 50% of patients may develop cerebral ischemia. These extracranial aneurysms are difficult to treat surgically, especially if they are tortuous, large, and located at a high cervical level [5-7].
Astley Cooper performed the first ligation of an extracranial carotid aneurysm on a symptomatic patient in 1805, since then the techniques have improved dramatically [8,9]. The largest review of these aneurysms was based on case reports published through 2014, covering a total of 1239 patients. The main treatment alternative was invasive therapy (89%), of which 94% had a surgical approach while 5% had an endovascular approach. The 30-day mortality rate and stroke rate in conservatively treated patients was 4.67% and 6.67%, and 1.91% and 5.16% after surgery, respectively [10]. Among the conclusions, limitations were found in the quality of evidence in the literature, which is why there is a need to increase clinical experiences in order to develop a treatment scheme. A review of institutional experience with Asian patients found that surgical and endovascular therapy offered the best long-term outcomes, however, the choice of treatment was based primarily on the surgeon's experience and difficulty of treatment [11].
We present the case of a patient who presents a right extracranial internal carotid artery (ICA) aneurysm at the upper cervical level. The aneurysm was successfully treated, without complications, by a high-flow bypass using a radial artery (RA) graft between the external carotid artery (ACE) and the M2 segment of the middle cerebral artery (ACE-RA-M2).
A 60-year-old female patient, natural and from Cajamarca, Peru, with no relevant pathological history, no surgical or family history, presenting with a sensation of pulsatile mass in the upper cervical region for 4 years that progressively increased in size. The patient reported difficulty swallowing, cervicalgia and headache, so she went to the cardiovascular surgery office of a national hospital in Lima where the diagnosis of an aneurysm of the cervical segment C1 of the internal carotid artery was made, which is why she is referred to neurosurgery for treatment. CT angiography and craniocervical angiography studies were performed in which the right extracranial aneurysm measuring 32 × 28 mm at level C1 was evidenced (Figure 1). To determine the anatomy of the donor vessels, vascular studies of the upper limbs were performed (Figure 2).
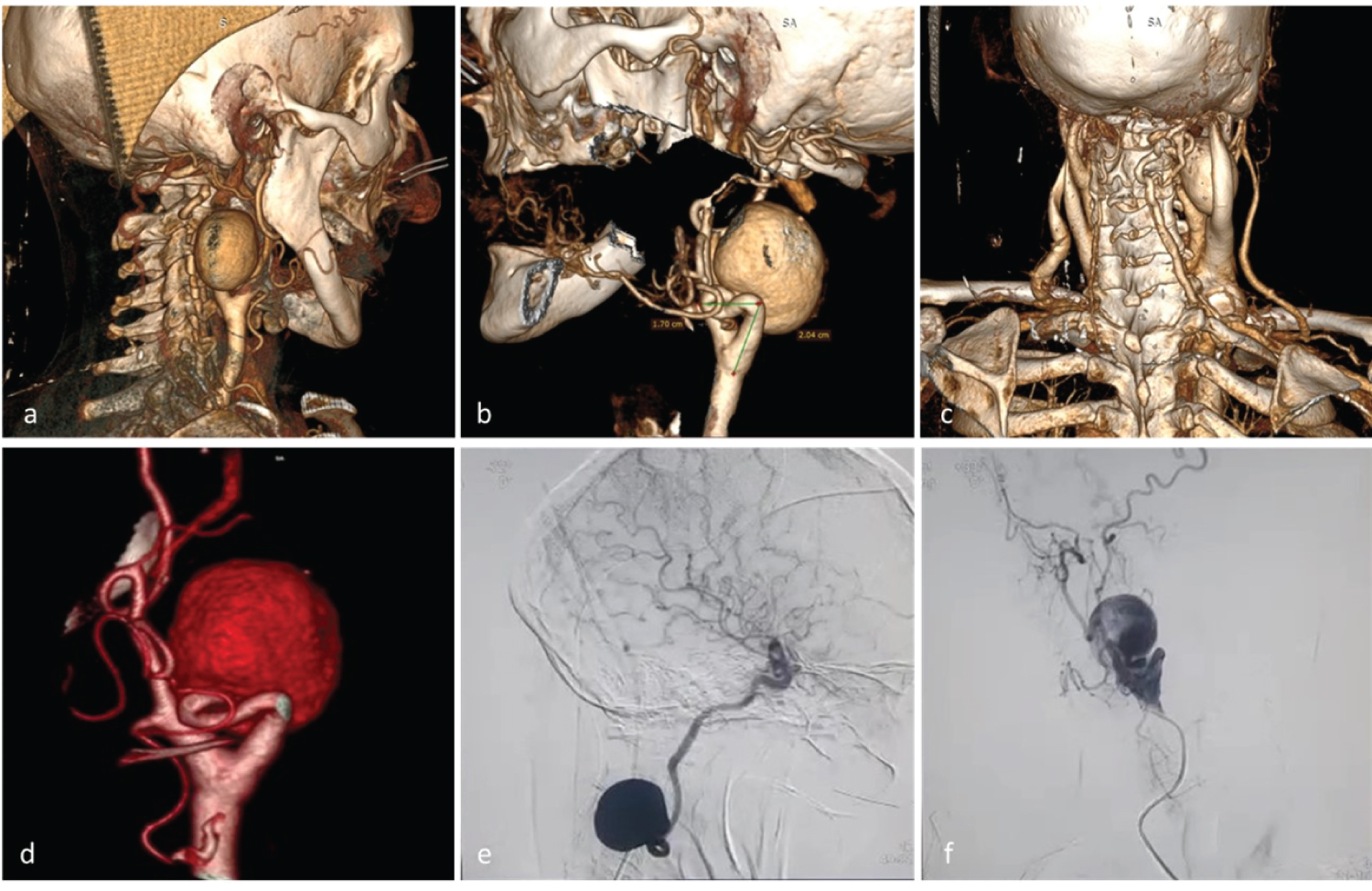 Figure 1: a,b,c) Cervical CT angiography show an extracranial internal carotid artery aneurysm of 32 × 28 mm. a) The upper end of the aneurysm partly behind the mandible; b) Tortuous cervical ACI proximal to the aneurysm; c) Posterior view C1 aneurysm; d,e,f) Cervical angiography. The angiogram of the right carotid artery shows a tortuous ICA with an irregular wall at the level of C1.
View Figure 1
Figure 1: a,b,c) Cervical CT angiography show an extracranial internal carotid artery aneurysm of 32 × 28 mm. a) The upper end of the aneurysm partly behind the mandible; b) Tortuous cervical ACI proximal to the aneurysm; c) Posterior view C1 aneurysm; d,e,f) Cervical angiography. The angiogram of the right carotid artery shows a tortuous ICA with an irregular wall at the level of C1.
View Figure 1
 Figure 2: a) Preparation of the left upper limb to proceed with graft collection; b) 3D reconstruction allows to determine the anatomy of the donor vessel (left radial artery); c,d) Head placement and positioning, marking of cranial and cervical approach areas.
View Figure 2
Figure 2: a) Preparation of the left upper limb to proceed with graft collection; b) 3D reconstruction allows to determine the anatomy of the donor vessel (left radial artery); c,d) Head placement and positioning, marking of cranial and cervical approach areas.
View Figure 2
After evaluating the studies, taking into account the location of the aneurysm, size, characteristics of the neck and tortuosity of the cervical internal carotid, surgical treatment was decided by a high-flow bypass using a radial artery graft (RA) and communicating the cervical external carotid artery with the M2 segment of the middle cerebral artery, subsequently ligation and closure of the cervical internal carotid artery (ACI).
After anesthetic induction, the vascular surgery surgical team, through a linear incision in the skin above the path of the artery, initiates the dissection and preparation of the left radial artery (RA), obtained the graft is prepared with heparinized saline and both ends are conditioned for anastomosis. Next, we proceed to the preparation of the right frontotemporal and cervical surgical area. A team of neurosurgeons performs frontotemporal craniotomy centered on the Silvian fissure. Another surgical team performs the cervical approach, dissecting and exposing the common carotid artery (ACC) to the bifurcation into internal carotid artery (ICA) and external carotid artery (ACE) preparing it for anastomosis, exposing the ACI aneurysm to the upper cervical region.
Exposed segment M2 of the middle cerebral artery (MCA), prepares to perform lateral term anastomosis, between the distal branch of the RA graft and segment M2 of the MCA, using a suture with separate points of nylon 10/0. After confirming that there were no leaks in the anastomosis, the radial graft was passed by subcutaneous tunneling under the skin prior to the swallow, avoiding rotation of the graft under the skin and confirmed permeability, temporarily releasing the clip in the graft near the MCA. A smooth, pulsating flow is observed through the non-anastomosed end of the graft. Another cervical proximal lateral term anastomosis is performed between the RA graft and the ACE. Subsequently, a definitive clip is placed at the proximal base of the aneurysm in the cervical ICH, again the vascular patency and anastomosis is corroborated by direct observation of the flow, microvascular Doppler and video angiography with sodium fluorescein, standard methods to corroborate the adequate patency of the graft and exclusion of the ICA and aneurysm (Figure 3).
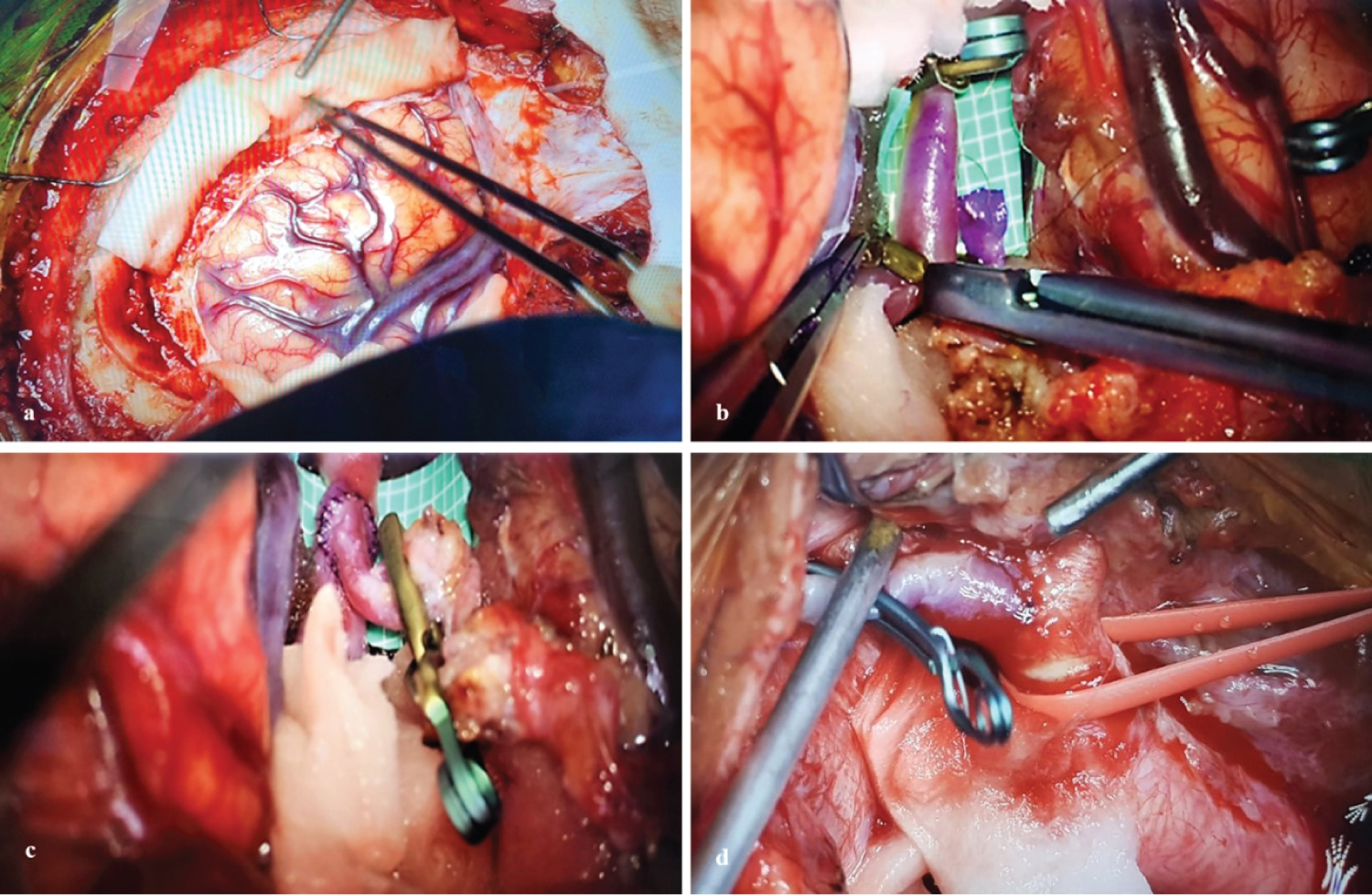 Figure 3: a) Right frontotemporal craniotomy with approach to the Silvian valley; b,c) Lateral term anastomosis between distal M2 - RA; d) Dissection and preparation ACE where distal anastomosis will be performed AR-ACE.
View Figure 3
Figure 3: a) Right frontotemporal craniotomy with approach to the Silvian valley; b,c) Lateral term anastomosis between distal M2 - RA; d) Dissection and preparation ACE where distal anastomosis will be performed AR-ACE.
View Figure 3
Hemostasis and technically regulated closure are carried out in order to allow the facing of the tissues without involvement of the vascular graft.
The postoperative evolution is favorable, remaining in the neurocritical care unit for 5 days, then hospitalization of the service for 3 days. Hemodynamically stable, glasgow: 15 and without motor or sensory deficit. During hospitalization control, the cervical mass is palpated with less volume, tension and pulsatile, no complications are shown and in the control CT angiography studies the patency of the high-flow bypass and clipping of the portion proximal to the ACI aneurysm can be observed (Figure 4). She was discharged with indications and a month later she went to outpatient check-ups where she was neurologically unchanged (Figure 5).
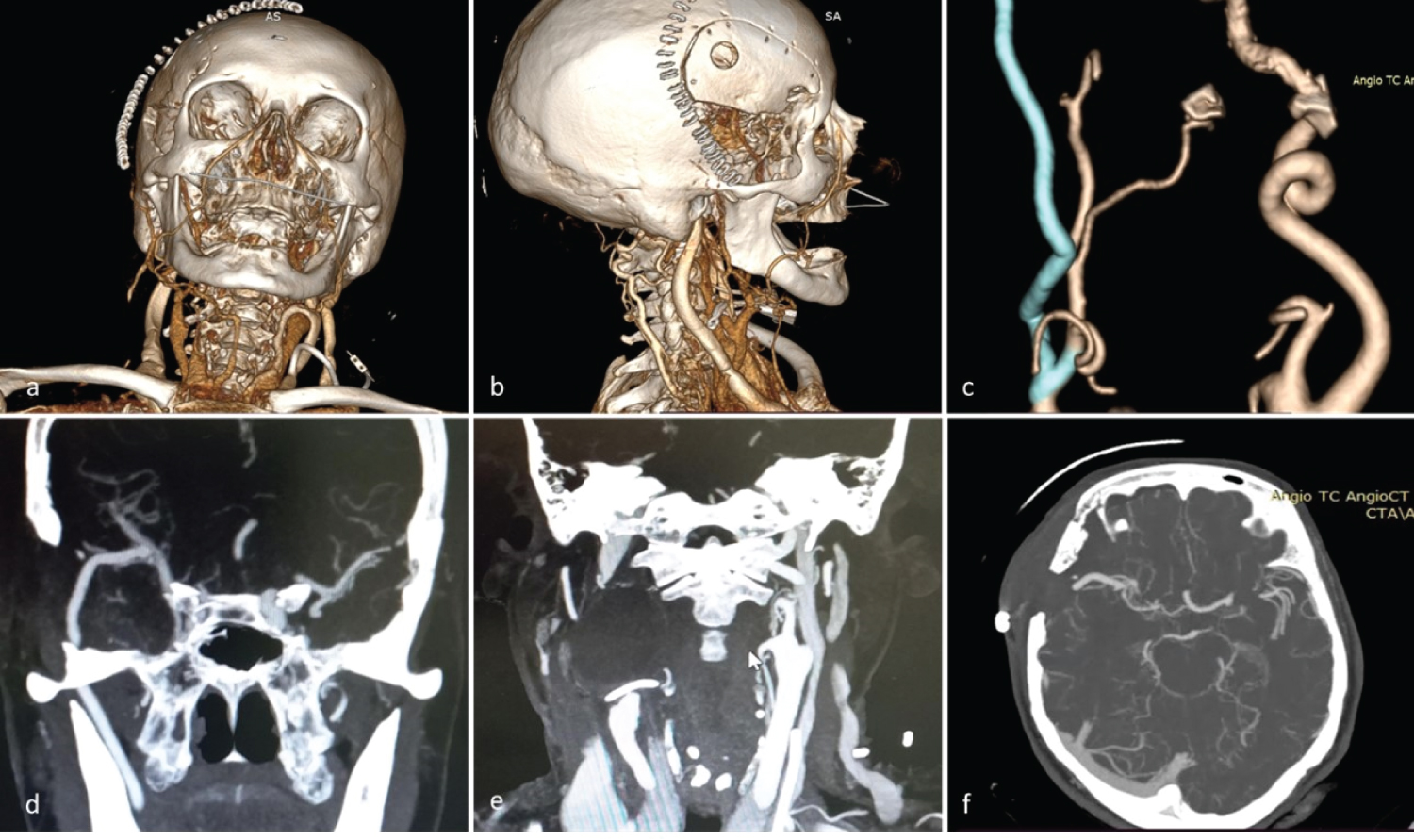 Figure 4: Post-surgical angiotem. a,b) 3D reconstruction evidences absence of extracranial ACI C1 aneurysm; c) 3D reconstruction of high-flow bypass with AR graft; d) Evidence permeable anastomosis AR - M2; e) Clip in ACI and exclusion of the aneurysm; f) Axial cut shows permeability of the high-flow bypass.
View Figure 4
Figure 4: Post-surgical angiotem. a,b) 3D reconstruction evidences absence of extracranial ACI C1 aneurysm; c) 3D reconstruction of high-flow bypass with AR graft; d) Evidence permeable anastomosis AR - M2; e) Clip in ACI and exclusion of the aneurysm; f) Axial cut shows permeability of the high-flow bypass.
View Figure 4
 Figure 5: Patient with good evolution. a) Limb mobilization and preserved strength; b) Adequate healing in the region of RA graft taking; c) Adequate cervical scarring and decreased volume of cervical mass.
View Figure 5
Figure 5: Patient with good evolution. a) Limb mobilization and preserved strength; b) Adequate healing in the region of RA graft taking; c) Adequate cervical scarring and decreased volume of cervical mass.
View Figure 5
Aneurysms in the extracranial internal carotid artery represent a rare but important disease, resulting from atherosclerotic degeneration, local infection, traumatic injury, radiation, dissection or as a complication after carotid endarterectomy [12,13]. Given the risk of ruptured aneurysms, as well as the neurological sequelae of cerebral thromboembolism, surgical intervention is recommended for extracranial carotid aneurysms to prevent complications [14,15]. The main symptoms of extracranial carotid aneurysms are headaches, sensation of pulsatile mass in the neck and focal neurological symptoms due to compression of the cranial nerves [3].
Surgical treatment is indicated for the management of these complex cervical aneurysms. There are potential risks as part of surgical treatment: Embolisms, difficulty in distal control or injury to adjacent structures (mainly the cranial nerves). The postoperative mortality rate is 2-6%, with morbidity due to neurological complications between 5.5-10% [6,16].
There is a risk of iatrogenic injury to a cranial nerve between 2.2-44%, with the highest risk when the aneurysm is at the high cervical level [5,7,15]. Direct clipping is recommended if the aneurysm is feasible to be excluded, otherwise it is not recommended if there is adhesion to adjacent tissues or the aneurysm is at a high cervical level [17].
In the present case, a high cervical aneurysm and tortuous ACI are reported, so it was decided to close the internal carotid artery (ICA) without direct repair of the aneurysm and perform a high-flow bypass using a radial artery (RA) graft. An excellent surgical clinical outcome is obtained, indicating that this strategy is a viable treatment option. An anastomosis is performed from the external carotid artery (ACE) to the M2 segment of the middle cerebral artery (MCA).
Some extracranial carotid aneurysms can be treated endovascularly [4,7], thus avoiding head nerve injury from exposing the neck to a high cervical level [18]. However, stroke, ruptured aneurysms, and blood vessel damage following endovascular stenting were also reported in endovascular procedures. A review of institutional experience cases found that 4.1% of patients died; 1.8% had a stroke; 6.3%, a late stroke and in 1% the carotid artery ruptured [2]. Surgical treatment of carotid artery tortuous aneurysms is complex; however, high-flow shunt offers a better alternative for patients in whom greater complications could be expected with endovascular treatment and neck clipping surgery of the aneurysm [19].
The technique used in this case is known as high-flow bypass surgery with radial artery grafting, which consists of taking a segment of the radial artery from the patient's arm and using it as a new blood vessel to divert blood around a blocked or damaged artery, thus, radial artery grafting being a common option in this technique due to its availability, ability to maintain blood flow and lower incidence of complications compared to other grafts [20].
The choice of high-flow bypass surgery with radial artery grafting is because this technique provides a good long-term patency rate and a lower complication rate compared to other techniques. In addition, the radial artery is an available and reliable graft for bypass surgery, with a high long-term patency rate and a low complication rate. In the case of the 65-year-old patient with extracranial internal carotid artery aneurysm, this technique was chosen because it was considered the best option to restore blood flow and prevent future cerebrovascular events [21,22].
It has been chosen to graft with the radial artery, because it is an artery of caliber suitable for use as a graft in bypass surgery, and it has been shown that radial artery grafting can have some advantages over other types of grafts, such as greater durability, lower rate of wound complications and a lower risk of infection [23].
Extracranial carotid aneurysm corresponds to a rare lesion of diverse etiology and poses a constant problem in the possibility of neurological complications such as cerebrovascular disease. Treatments include medical, surgical and endovascular management, with surgery being the main treatment for years. In recent decades, endovascular therapy has been shown to be effective for certain types of carotid aneurysms. Patients with tortuous carotids or extracranial carotid artery aneurysms that were located at a high cervical level were successfully treated by clipping the internal carotid artery and placing a high-flow bypass using a radial artery graft. The individualization of the treatment for each patient considering the characteristics of the aneurysm (size, type, location, height and adjacent structures possible to be affected) allow obtaining better results during surgery and with fewer complications in the postoperative period.
We have not had any source of financial support nor do we have any conflict of interest.