Oblique lumbar interbody fusion (OLIF) can achieve better reconstruction of the lumbar spine via the anatomic corridor between the psoas muscle and the great vessels. Despite OLIF is considered as an effective and relatively safer procedure, congenital anomalies of the main vessels surrounding the oblique corridor may pose higher risk of vascular damage, which should bear in mind in deciding to use the OLIF procedure. We presented a case of an anomalous left-sided inferior vena cava (IVC) who underwent an OLIF procedure alternatively through a larger corridor between the aorta and the right psoas muscle. The lumbar sympathetic trunk (LST) could be observed and subsequently protected at the medial border of the right psoas muscle. Eventually, the right-side OLIF procedure was successfully performed, and there were no perioperative or postoperative complications. The presence of a left-sided IVC can bring a major pitfall to the OLIF procedure, despite rarely occurred in clinical practice. A preoperative recognition of this IVC anomaly is critical to the safe performance of the OLIF procedure. Detailed preoperative consideration should be taken to make the optimal choice of accessible approach and prevent potential complications associated with the vascular interference. The protection of LST should be taken into full consideration in either left or right sided approaches.
Oblique lumbar interbody fusion, Left-sided inferior vena cava, Lumbar interbody fusion
Oblique lumbar interbody fusion (OLIF) has become an increasingly common minimally invasive surgical intervention for treating lumbar spine pathologies, involving degenerative disc disease, spondylolisthesis and deformity [1-4]. The OLIF procedure generally utilizes the anatomical plane between the great vessels and psoas muscle to access the target disc space, with the theoretical advantages of preserving musculoligamentous structures, avoiding the psoas muscle and lumbar plexus injury, and simultaneously obtaining deformity correction and indirect decompression. Recently, several published literatures have demonstrated the early favorable clinical outcomes of the OLIF procedure in lumbar spine surgery [2,5].
Despite OLIF is considered as an effective and relatively safer procedure, a variety of perioperative complications have been reported to range from 3.7% to 66.7% [5-10]. Damage to the main vessels is the most threatening complication among the OLIF procedure [2,9,10]. Therefore, a careful preoperative analysis of the vascular anatomy is of paramount importance for surgical safety of the OLIF procedure. The anatomic variation of the main vessels surrounding the oblique corridor, evidenced by the preoperative images, can downsize the surgical window and increase the incidence of vascular complication during the exposure, which should bear in mind in deciding to use the OLIF procedure. In the current study, we present a case of ananomalous left-sided inferior vena cava (IVC) underwent an OLIF procedure through an alternative right-sided approach who have been successfully treated by the right-side OLIF procedure [11,12].
A 77-year-old man was presented with progressively worsen low back pain and neurogenic claudication after failure of conservative management of approximately 6 months. His medical history was unremarkable except for hypertension. Physical examination revealed tenderness in the region of the lower lumbar spine, but the neurological assessment was intact. Preoperatively, his standing lateral radiograph of the lumbar spine showed that spondylolytic spondylolisthesis was noticed at the level of L4-L5 (Figure 1a). Dynamic flexion-extension lateral radiographs demonstrated markedly segmental instability within the olisthetic L4-L5 level (Figure 1b and Figure 1c). An magnetic resonance imaging (MRI) scan of the lumbar spine revealed an hourglass form of the thecal sac in the sagittal view at the level of L4-L5 (Figure 1d). Based on the physical and radiographic assessment, the OLIF technique combined with posterior pedicle screw instrumentation were selected for minimally invasive treatment of the patient. However, the dimension of the left oblique access corridor to the L4-L5 disc space between the main vessels and the left psoas muscle was significantly reduced by the abnormal prevertebral vascular structure (Figure 1e). All axial and sagittal computed tomography (CT) images were carefully reviewed, indicating a rare anatomical vascular variation, with an anomalous left-sided IVC and an anomalous aorta (Figure 2). The aberrant pathway of IVC was noticed to initially be on the left side of the abdominal aorta, then crossing over anterior to the aorta above the level of the renal veins, and eventually ascending to its normal right-sided anatomical position. The congenital anomalies of the IVC were also visualized vividly in reconstruction computed tomography angiography (CTA) of the retroperitoneal vessels (Figure 3).
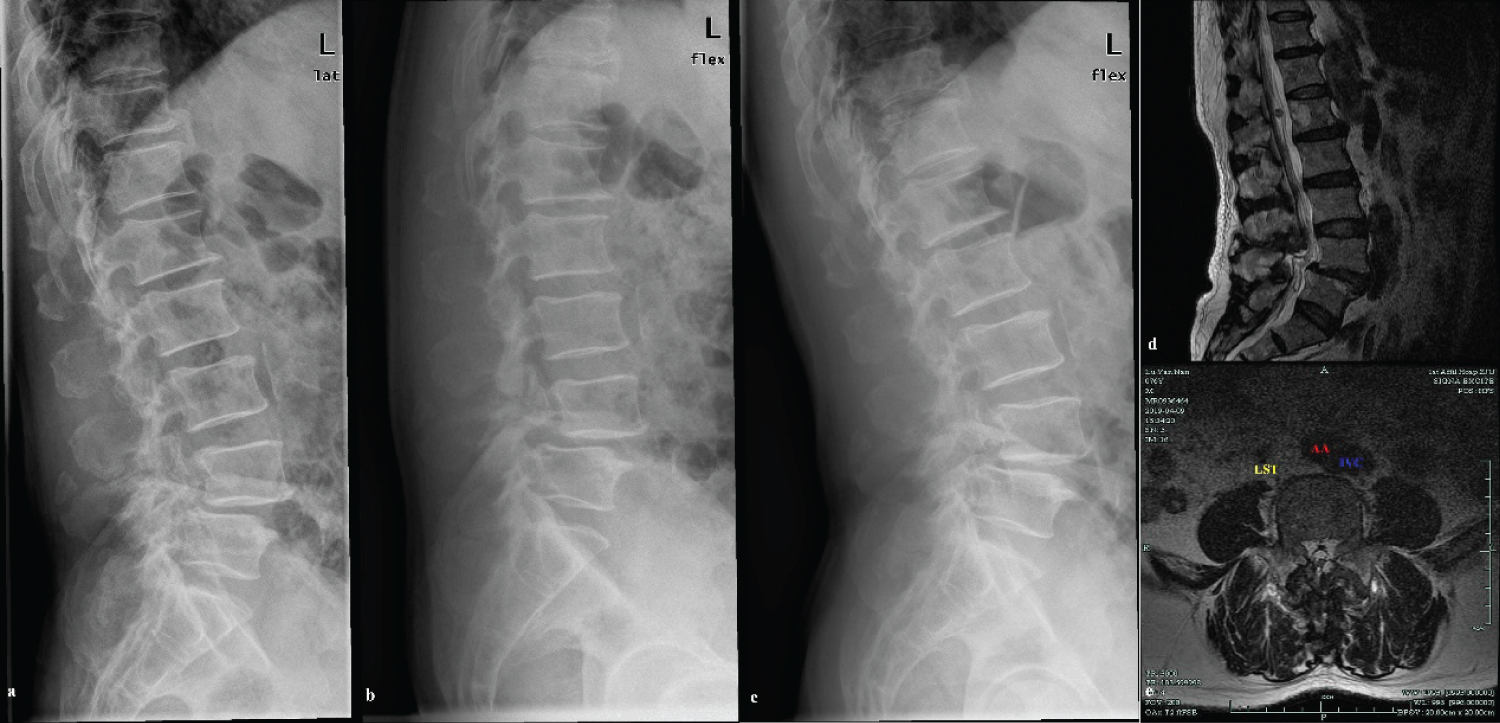 Figure 1: (a-c) Preoperative lateral and dynamic flexion-extension radiographs of the lumbar spine showed that spondylolytic spondylolisthesis at the level of L4-L5; (d) A midline preoperative T2-weighted MR image demonstrated stenosis the olisthetic L4-L5 level; (e) An axial T2-weighted MR image showed the abnormal prevertebral vascular structure and position of the LST. View Figure 1
Figure 1: (a-c) Preoperative lateral and dynamic flexion-extension radiographs of the lumbar spine showed that spondylolytic spondylolisthesis at the level of L4-L5; (d) A midline preoperative T2-weighted MR image demonstrated stenosis the olisthetic L4-L5 level; (e) An axial T2-weighted MR image showed the abnormal prevertebral vascular structure and position of the LST. View Figure 1
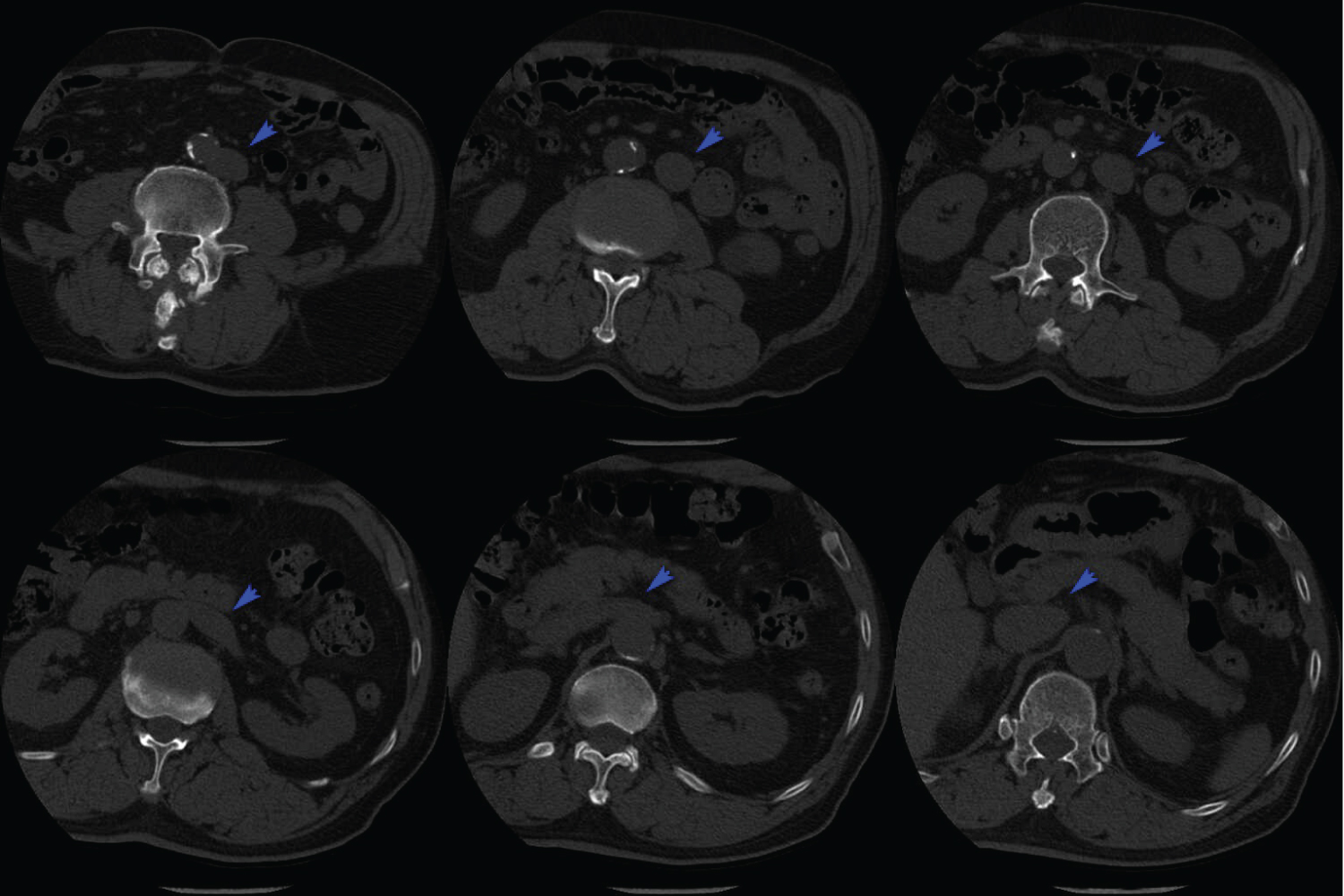 Figure 2: Axial CT images of the lumbar spine from L4-L5 inferiorly to T12-L1 superiorly, showed the pathway of left-side IVC (Blue arrow). The dimension of the left oblique corridor at the level of L4-5 is significantly downsized by the anomalous left-side IVC. View Figure 2
Figure 2: Axial CT images of the lumbar spine from L4-L5 inferiorly to T12-L1 superiorly, showed the pathway of left-side IVC (Blue arrow). The dimension of the left oblique corridor at the level of L4-5 is significantly downsized by the anomalous left-side IVC. View Figure 2
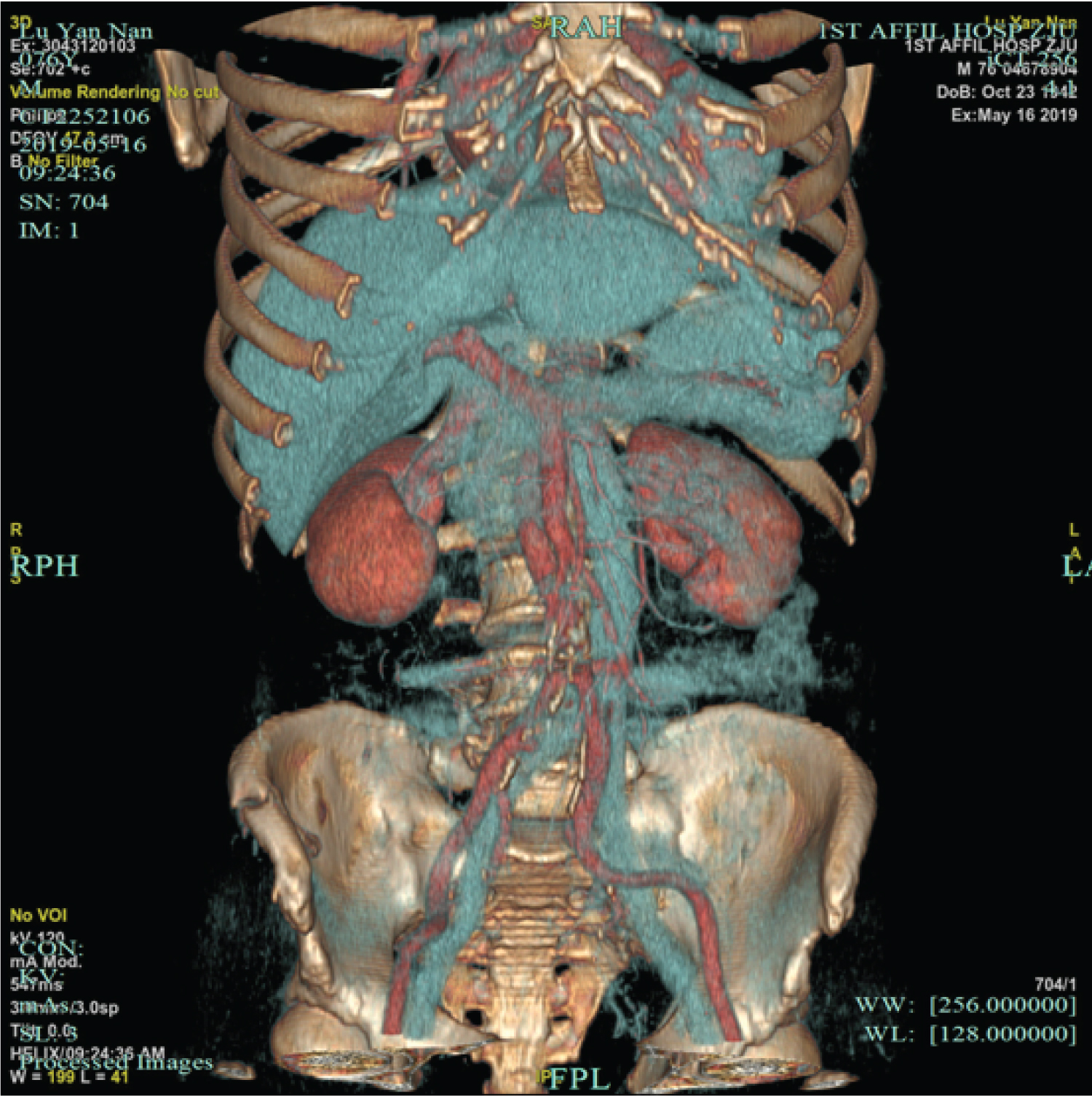 Figure 3: A reconstructed CTA of retroperitoneal vessels confirmed that the inferior vena cava was located on the left side. View Figure 3
Figure 3: A reconstructed CTA of retroperitoneal vessels confirmed that the inferior vena cava was located on the left side. View Figure 3
Considering the anomalous vascular anatomy of the patient, the OLIF procedure was selectively approached on the right side for the sake of surgical safety. The patient was positioned in the left lateral decubitus. A 4 cm oblique anterolateral incision was made, centered towards the landmark midpoint of the L4-5 disc. After performing a skin incision, the external oblique, internal oblique, and transversus abdominis muscles were split successively. Blunt finger split was used to open transversal fascia and access the retroperitoneum. The retroperitoneal fat could be observed and the peritoneum was swept anteriorly using tonsil sponges. The lumbar sympathetic trunk (LST) could be observed and subsequently protected at the medial border of the psoas muscle (Figure 4). A probe was inserted anterior to the psoas muscle into the L4-5 disc, located at the junction of the anterior one-third and posterior two thirds portions. Then the discectomy and endplate preparation are performed through the anatomical space between the aorta and the right psoas muscle. Different sizes of the trials were sequentially used to distract the disc space and release the contralateral annulus. Finally, a proper sized cage (Medtronic Clydesdale, Memphis, Tennessee) was inserted with the guide of C-arm. Incision closure was performed in a layered fashion and posterior placement of pedicle screws was used to provide supplemental fixation.
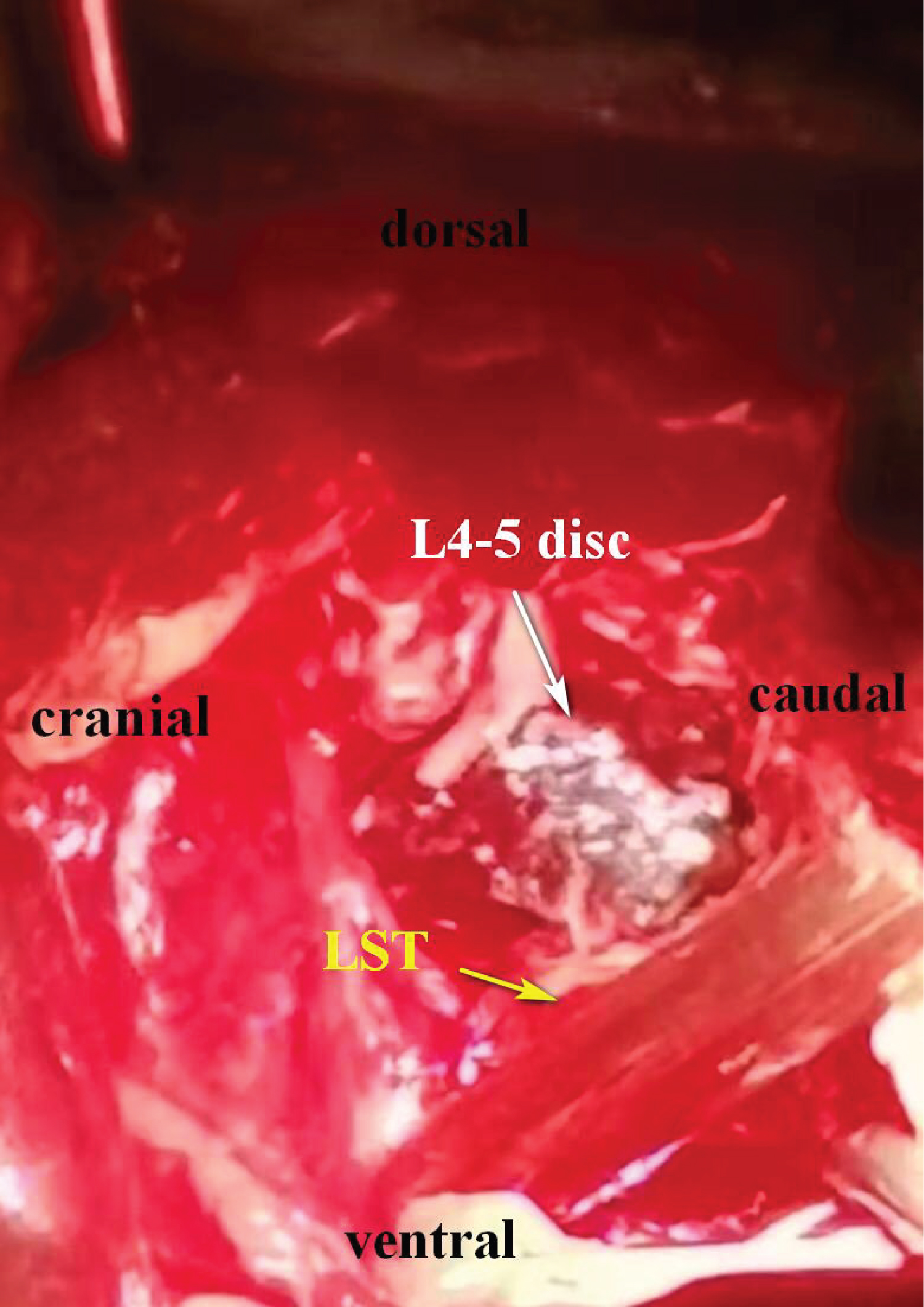 Figure 4: An intraoperative image of lumbar sympathetic truck. View Figure 4
Figure 4: An intraoperative image of lumbar sympathetic truck. View Figure 4
The blood loss was approximately 100 ml and there were no perioperative or postoperative complications. Immediate postoperative radiographs of the lumbar spine demonstrated a satisfactory L4-5 reconstruction with good cage position (Figure 5a and Figure 5b). There were no perioperative complications during his hospitalization, and the patient was discharged 5 days after surgery. At 12-week postoperative follow-up, his symptoms improved markedly and the good position of both cage and pedicle screws were maintained (Figure 5c and Figure 5d).
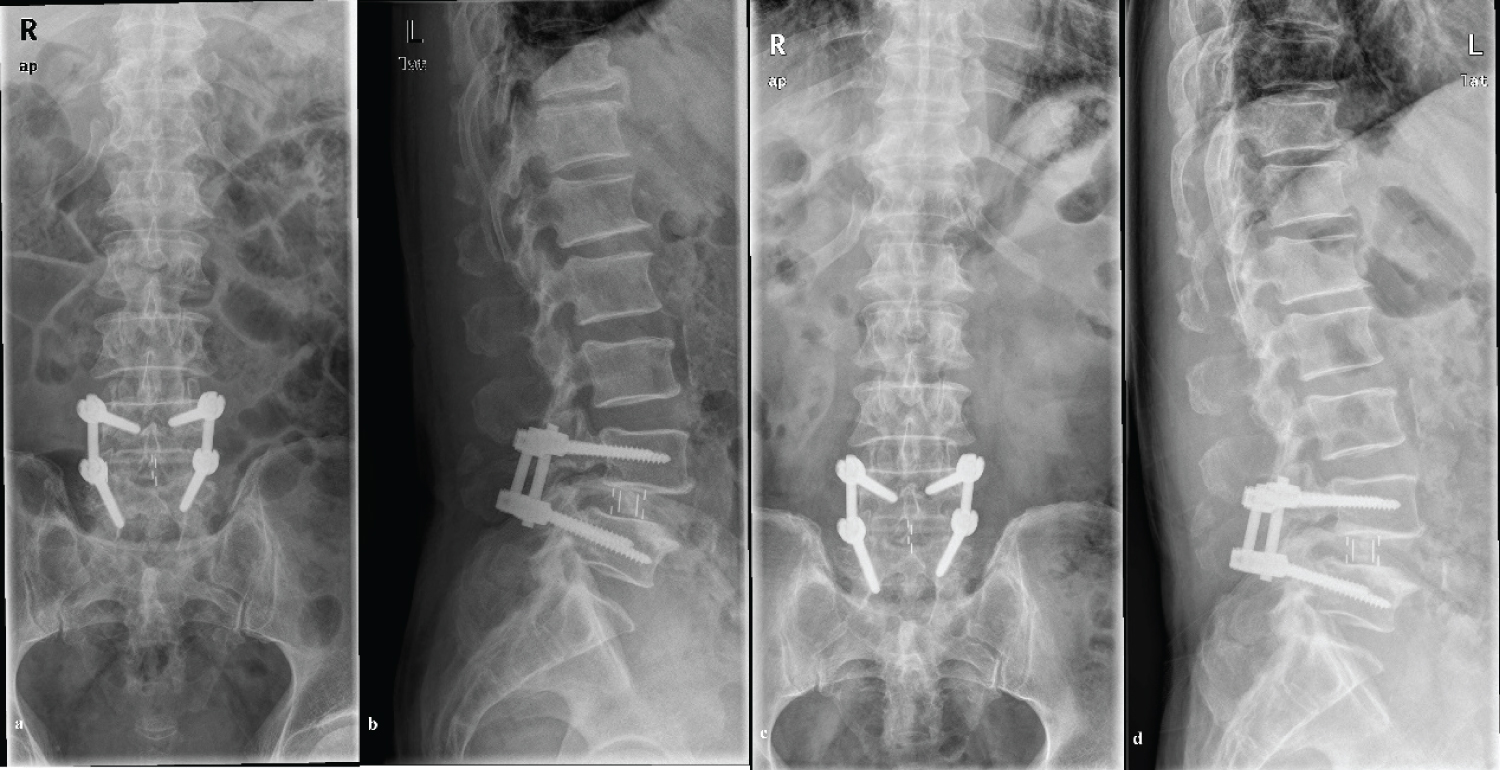 Figure 5: Immediate postoperative (a,b) and 3-month follow-up (c,d) radiographs of the lumbar spine showed a satisfactory L4-5 reconstruction with good cage position. View Figure 5
Figure 5: Immediate postoperative (a,b) and 3-month follow-up (c,d) radiographs of the lumbar spine showed a satisfactory L4-5 reconstruction with good cage position. View Figure 5
A left-sided IVC is a rare congenital inferior cava anomaly in the normal population, with the estimated incidence of 0.2% to 0.5% [13]. The vast majority of the left-sided IVC anomalies is asymptomatic, and can be discovered incidentally on abdominal imaging examination [13]. The undiagnosis of left-sided IVC can bring greater difficulty to the certain surgical procedures, which may result in iatrogenic venous damage. So the importance to identify the left-sided IVC has been previously stressed in a variety of surgeries [14-17]. However, there yet have been few clinical reports of the OLIF procedure utilized in patients with left-sided IVC. To our knowledge, including our patient, only 3 patients with such conditions have been reported in readily available published English-speaking literatures (Table 1).
Table 1: Published cases with left-sided IVC underwent OLIF operation. View Table 1
The OLIF procedure is an innovative surgical technique for reconstruction of the lumbar spine via the anterior oblique retroperitoneal approach. Commonly in the standard protocols of OLIF, the oblique corridor between the abdominal aorta and the left psoas major is recommended to consistently access the L2-5 disc space, due to the relatively larger size of surgical window and obviating the need for venous retraction on the left-side approach [2,9]. However, among these patients with left-sided IVC, a transposed IVC markedly decrease the dimensions of the left oblique corridor, which poses more technical difficulties for the access surgeons [11,12]. Therefore, retraction of the IVC will be essentially required to obtain adequate exposure for discectomy, which may significantly enhance the risk of intraoperative vascular damage. Instead, the right-side approach becomes one alternative choice for performing an OLIF in this situation. Eventually, all these three patients have been successfully treated by the right-side OLIF procedure [11,12].
Despite the larger oblique corridor available on the right-side approach, another important structure the LST crossing the surgical field, make it susceptible to injury in the OLIF procedure [18]. Incidentally injury to the unilateral LST can lead to vasodilation induced warmth and edema in the affected limb [19,20]. Thus, the LST protection should be taken into consideration whether either left or right sided approaches will be chosen. Surgeons can individually analyze the preferred oblique corridor on axial MR images to identify the position of the LSC (Figure 1e) [18,19]. Referring to the preoperative radiographic assessment, meticulous manipulation should be done intraoperatively to avoid iatrogenic damage of the LST.
Currently, there is consensus among the spine surgeons that detailed preoperative evaluation of the prevertebral anatomy is of vital importance in the anterior or anterior oblique lumbar surgery, especially the variation in vascular anatomy [2,9,11,12,21]. The presence of a left-sided IVC can be initially identified on preoperative CT or MRI cross-sectional images of the lumbar spine. Furthermore, the anatomic course of the anomalous IVC and its relationship with the oblique corridor to the disc space can be thoroughly analyzed based on available axial or coronal CTA images. The seradiographic evidences may provide comprehensive valuable information for the diagnosis of left-sided IVC and the plan of the optimal approach, which will warrant the safety of the OLIF procedure. Therefore, we still emphasized the importance of the preoperative imaging assessment to the utilization of the OLIF procedure.
In conclusion, despite rarely occurred in clinical practice, the presence of a left-sided IVC can bring a major pit fall to the OLIF procedure. A preoperative recognition of this IVC anomaly is critical to the safe performance of the OLIF procedure. Detailed preoperative consideration should be taken to make the optimal choice of accessible approach and prevent potential complications associated with the vascular interference. The protection of LST should be taken into full consideration in either left or right sided approaches.