Resection of a cavernous sinus tumor may be performed utilizing three primary approaches: The middle cranial fossa epidural approach, the combined transsylvian-subtemporal approach, and the medial transsphenoidal approach.
Herein, we describe an exceedingly rare cavernous sinus chondroma in an 18-year-old male who presented with a history of binocular diplopia and trochlear nerve palsy. Brain CT scan detected a left sided cavernous sinus calcified mass and the MRI confirmed an enhancing lesion in the left cavernous sinus and the patient subsequently underwent successful resection of the mass via a pre-temporal trans-cavernous approach. Histopathological biopsy provided the definitive diagnosis of a cavernous sinus chondroma.
In this report, we discuss diagnostic imaging and review the current literature on management strategies for the treatment of cavernous sinus chondromas in the pediatric population.
Cavernous sinus, Chondroma, Middle cranial fossa, Transsylvian-subtemporal approach, Sellar chondroma, Pretemporal transcavernous resection
Intracranial chondromas are rare benign tumors with a prevalence of only 0.2-0.3% in the general population [1]. Such tumors are most often diagnosed in the third decade of life and have no gender predilection [2]. Chondromas predominantly arise at the base of the skull in the sellar region from embryonic chondrocytic cell remnants, and are also common in the falx and convexity dura [3-5]. Though rare, chondromas may present in the cavernous sinus as well.
The cavernous sinus (CS) is a dural venous plexus traversed by neurovascular structures including the cavernous segment of the internal carotid artery (ICA), oculomotor nerve, trochlear nerve, abducent nerve and ophthalmic and maxillary divisions of the trigeminal nerve. Clinical presentation of CS lesions may vary in accordance with neurovascular disturbances; CS syndrome is characterized by paresis of one or more cranial nerves (III-VI), with or without associated ophthalmoplegia [6,7]. Common tumors of the cavernous sinus include meningiomas, neurogenic tumors, hemangiomas, epidermoid cysts, dermoid cysts, schwannomas, and pituitary adenomas [6,8].
Germ cell tumors and tuberculomas are also rare entities found in the cavernous sinus in the pediatric population [9-11]. Although chondromas of the cavernous sinus are extremely rare in the pediatric population; common lesions in the cavernous sinus include B cell lymphoma, Hodgkin lymphoma, Burkitt lymphomas as well as Tolosa-Hunt syndrome (Table 1) [8,12]. A study by Su J, et al., reported one chondroma in a case series of 31 cavernous sinus tumors in adults [12]. Another case report detailed the management of a chondroma in a 40-year-old patient [8,13]. Further management of intracavernous tumors is described over an 11-year time period by Sepehrnia, et al., with mention of only one Chondroma [14].
Table 1: Historical cavernous sinus lesions. View Table 1
In the case described below, we highlight a pediatric cavernous sinus chondroma and describe the incidence and management of such tumors.
An 18-year-old male with no significant past medical history presented with a three week history of worsening left monocular diplopia and compensatory head tilt. Five months prior to presentation left sided neglect was noted by his father. He denied any associated symptoms including headaches, nausea, fatigue, bone/back/neck pain, or changes in cognition/speech/hearing. Initial neurological examination revealed left abducens nerve palsy and partial left trochlear nerve palsy, as well as anisocoria with left pupil larger than the right. The patient underwent brain and orbital magnetic resonance imaging (MRI) revealing a 27.3 × 29.0 × 18.6 mm left cavernous sinus mass arising from the petrous apex with extension into the cavernous sinus and the Dorello's canal; such findings are consistent with the presenting symptoms (Figure 1A and Figure 1B). The CT scan confirmed a calcified mass (Figure 2A and Figure 2B). Patient was hospitalized and scheduled for resection of the left cavernous sinus.
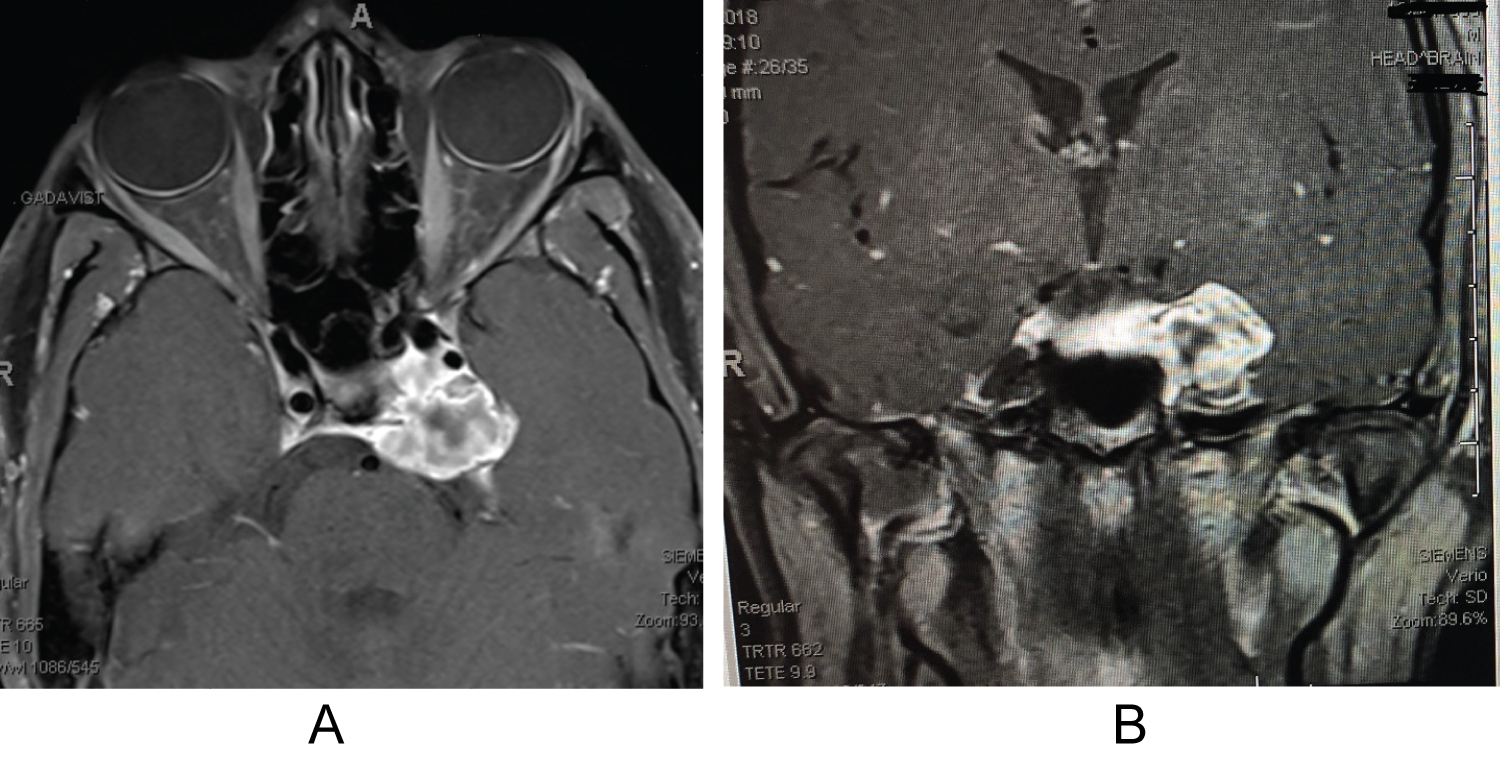 Figure 1: (A,B) Pre-operative axial and coronal brain MRI imaging using T1 sequence with contrast shows the heavily enhancing mass arising from the left cavernous sinus with mass effect on mesial temporal lobe and displacement of the ICA artery. View Figure 1
Figure 1: (A,B) Pre-operative axial and coronal brain MRI imaging using T1 sequence with contrast shows the heavily enhancing mass arising from the left cavernous sinus with mass effect on mesial temporal lobe and displacement of the ICA artery. View Figure 1
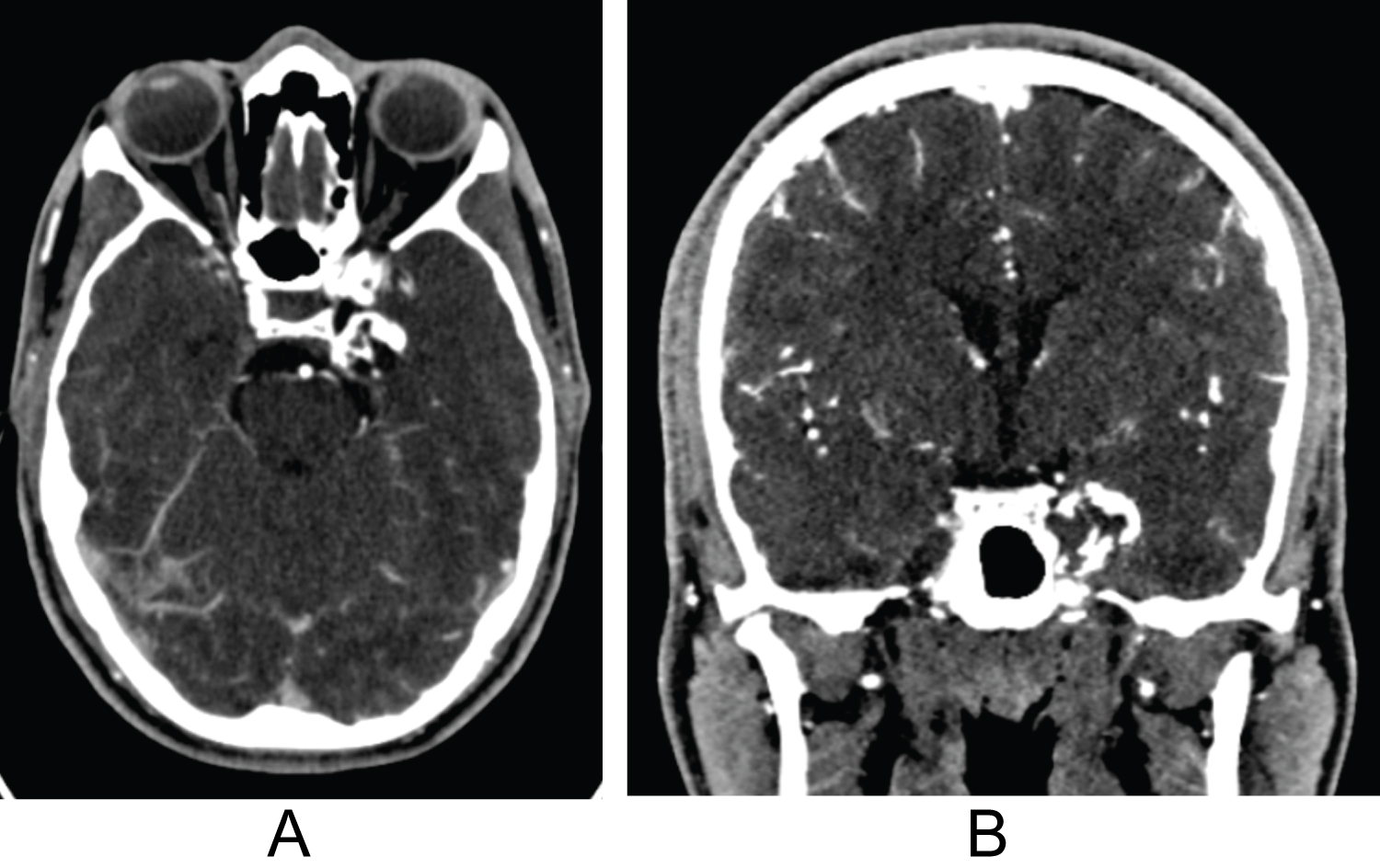 Figure 2: (A,B) Pre-operative axial and coronal brain CT with contrast shows the partially calcified mass arising from the left cavernous sinus with mass effect on mesial temporal lobe.
View Figure 2
Figure 2: (A,B) Pre-operative axial and coronal brain CT with contrast shows the partially calcified mass arising from the left cavernous sinus with mass effect on mesial temporal lobe.
View Figure 2
Under general anesthesia, the patient underwent resection of the left cavernous sinus mass via a combined extra-dural and intra-dural pre-temporal middle fossa skull-base approach to the cavernous sinus. Stereotactic navigation was employed to ensure accurate localization of the mass. A lumbar drain was placed in the cal sac with drainage of 50 ccs for relaxation of the temporal lobe prior to resection of the mass. Upon entering the tumor sac, soft grayish material as well as a heavy calcified component was noted. Internal debulking of the tumor ensued though the cavernous sinus and into the posterior fossa (Dorello's canal). Cranial nerves III, IV, V1, V2 and VI were all identified and preserved. A component of the tumor displaced the cavernous segment of the carotid artery; the artery was carefully decompressed by further debulking of the mass. After successful successful resection of the cavernous sinus lesion, duraplaty was performed followed by cranioplasty of the pre-temporal skull defect using the autologous bone flap and titanium mesh. Throughout the procedure there were no changes in continuous SSEP, MEP and EEG neurophysiologic monitoring.
Histopathological examination of the mass revealed a benign chondroma with no signs of atypia. The patient remained hospitalized for 4 days with no complications. The lumbar drain was opened hourly to drain 10 ccs and removed on day 3 post-surgery with total drainage of 420 ccs. An alternating eye patch for 6th cranial nerve palsy was started post-operatively. Three-day post-operative MRI demonstrated successful resection of the cavernous sinus mass with no signs of hemorrhage or infaction.
During the three month follow up visit, there was residual diplopia and decreased sensation upper part of left forehead (V1 distribution). At the 12-month follow up visit, the patient reported persistent but much improved CN VI palsy with intermittent conjunctival irritation and persistent decreased sensation at left cranial nerve V1 distribution. 12-month post-op MRI noted improved decompression of the cavernous sinus and residual postoperative enhancement along left petroclinoid ligament with extension toward the cavernous sinus (Figure 3A and Figure 3B).
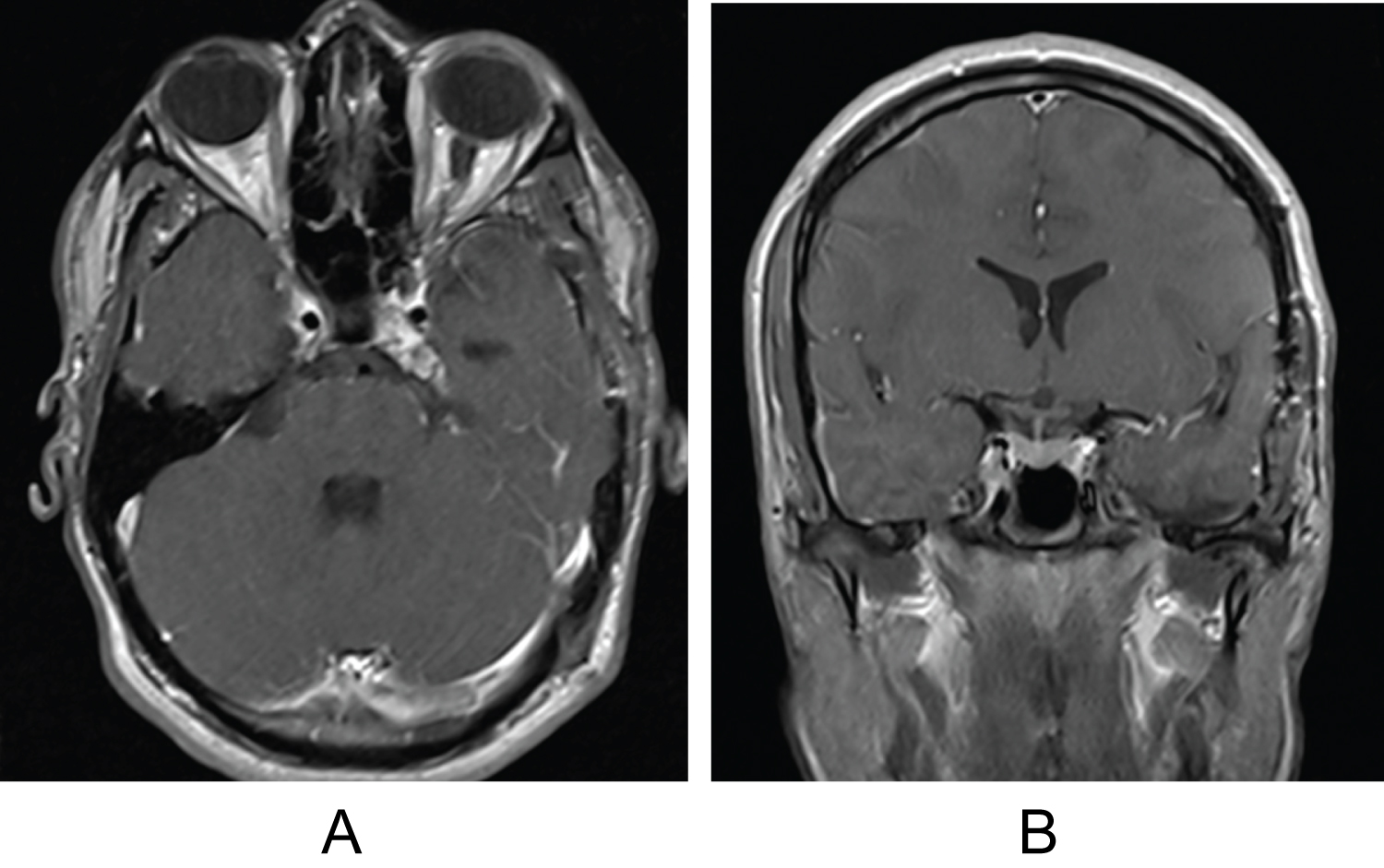 Figure 3: (A,B) 12 months post-operative axial and coronal brain MRI imaging using T1 sequence with contrast shows gross total resection of the cavernous sinus mass with improved mass effect on mesial temporal lobe and ICA artery.
View Figure 3
Figure 3: (A,B) 12 months post-operative axial and coronal brain MRI imaging using T1 sequence with contrast shows gross total resection of the cavernous sinus mass with improved mass effect on mesial temporal lobe and ICA artery.
View Figure 3
At the 18-month follow up visit, the patient reported resolution of the diplopia. Examination revealed near total resolution of the cranial nerve VI palsy as well as improved left cranial nerve V1 distribution sensory deficit.
Despite the rarity of cavernous sinus chondromas, the incidence of cranial basal chondromas is well documented; these tumors generally arise in the sellar, clival or parasellar region. Origins of basal chondromas stem from residues of primordial cartilaginous cranium replacing synchondroses. Clinical presentation of these masses varies by location; sellar chondromas may present with chiasma syndrome, quadrantanopia, decline of visual acuity and/or hypophyseal insufficiency. Parasellar and clival chondromas are often characterized by symptoms of cranial nerves III-VI disruption [14].
Cavernous sinus chondromas can be managed via application of standard cavernous sinus mass resection protocol. Initial magnetic resonance imaging should include T1-weighted and T2-weighted sequences in axial and coronal planes, fluid attenuated inversion recovery (FLAIR) sequences in the axial plane (including brain), 3D heavily T2- weighted sequences in the axial plane which aids in definition of cranial nerves, and contrast-enhanced imaging. Additional T1-weighted fat-saturated sequences in the axial and coronal planes may aid in the discrimination of the normal cavernous sinus anatomy. Standard cavernous sinus imaging demonstrates intense homogenous enhancement following contrast administration with central flow void due to the traversing ICA, and a filling defect posterolaterally due to Gasserian ganglion in the dural recess, commonly referred to as Meckel's cave [8].
Chondromas often present as solid masses which firmly adhere to adjacent structures. Such anatomic tendencies, in addition to traversing the densely packed landscape of the cavernous sinus, pose a challenge to safe resection [15]. Major CS afferent venous channels include the sphenoparietal sinus, the superior and inferior ophthalmic veins, and the sylvian vein; while the notable efferent venous channels include the superior and inferior petrosal sinuses. The cavernous segment of the ICA and the 6th cranial nerve traverse medially through the CS; the abducens nerve positioned inferolateral to the ICA. The oculomotor, trochlear, and ophthalmic and maxillary divisions of the trigeminal cranial nerves are positioned laterally in the cavernous sinus - anteriorly to posteriorly [16].
Due to significant improvements of the neurovascular techniques, the study of the cavernous sinus anatomy has been the object of great interest due to the well-known advantages of the trans-cavernous approach in the treatment of selected aneurysms such as basilar tip aneurysms or posterior fossa tumors with petrosal extensions [17,18].
Given its delicate anatomy, primary approaches to enter the cavernous sinus include the middle cranial fossa epidural approach, the combined transsylvian-subtemporal approach, and the medial transsphenoidal approach. The middle cranial fossa epidural approach allows for access via the Glasscock triangle and provides the greatest exposure of the lateral surface of the posterior vertical and horizontal segments of the ICA, the posterior bend, and the lower part of the anterior bend [19]. The combined transsylvian-subtemporal approach initially exposes the upper wall of the cavernous sinus and proceeds into the anterior medial CS via the triangle defined by Dolenc or to the medial CS via the triangle defined by Hakuba [20,21]. Access via the anteromedial and medial triangle provides exposure to the roof of the CS; while entrance via the Parkinson triangle allows access to the lateral wall of the CS [22]. The transsphenoidal approach, is nowadays almost exclusively performed endoscopically [23]. A common encounter during cavernous sinus approach involves venous bleeding requiring adequate hemostasis.
In the case presented, a cavernous sinus chondroma resection was performed in an 18-year-old male via a pretemporal trans-cavernous approach. A pre-temporal craniotomy was performed using three burr holes. Microsurgical resection yielded visualization of the floor of the middle cranial fossa anteriorly to the temporal pole. Extradural elevation of the temporal lobe was performed until the arcuate eminence was appreciated posteriorly.
Anterior medial extradural dissection was taken until the V1 and V2 branches of the trigeminal nerve were dissected extradurally. The calcified tumor was palpated within the petrous apex and the dura was opened in a vertical manner to enter the tumor cavity. Such an approach primarily exposes the lateral wall of the cavernous sinus and upper basilar region via removal of the anterior and/or posterior clinoid processes. Lateral expansion exposes Meckel's cave with widening possible via resection of the petrous apex to aid in further debulking of tumors within this eloquent region [17].
Cavernous sinus lesions in the pediatric population are rare; management of such tumors is not well documented in current literature. Three standard approaches to cavernous sinus mass resection include the middle cranial fossa epidural approach, the combined transsylvian-subtemporal approach, and the medial transsphenoidal approach. This case report describes successful management of cavernous sinus chondroma in a young adult via a pretemporal trans-cavernous approach and discusses standard diagnostic and management strategies for cavernous sinus resections.
The project was completed without financial support.
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Data was obtained via EMR and via pubmed indexed articles for comprehensive literature review.
N/A.
Carlos Roberto Massella Jr and Yasmeen Elsawaf wrote the manuscript and edited per the direction of Sabino Luzzi, Paulo Macio Porto de Melo and Samer K. Elbabaa. The idea for the manuscript was led by Carlos Roberto Massella Jr, Paulo Macio Porto de Melo and Samer K. Elbabaa and Sabino Luzzi primarily assisted with editing of the final manuscript. All authors were involved in the final approval of the manuscript.