Pregnancy can change the behavior of brain gliomas with increased growth rate, increased frequency of seizures, and anaplastic transformation. Very rarely the presentation may be hyperacute due to intratumoral hemorrhage. We report and discuss them a management of the hemorrhagic infarction of a newly diagnosed postcentral anaplastic astrocytoma in a pregnant woman. A first MRI discovered the glioma; two days later, after acute neurological deterioration, a second MRI showed a dramatic increase in volume with intratumoral hemorrhage, possibly caused by venous thrombosis. The patient underwent a cesarean section and an urgent craniotomy with subtotal resection and a good neurological outcome. An urgent craniotomy can be performed either during pregnancy or after a cesarean delivery if the patient is at least in the gestational age of 34-36 weeks. Not only decompressing but also resecting the tumor allows performing the first stage of oncological treatment and avoiding a second surgery. Despite a potential catastrophic onset, even this type of presentation can lead to good clinical results.
Glioma, Anaplastic astrocytoma, Pregnancy, Hemorrhagic brain tumor, Intratumoral hemorrhage, Urgent craniotomy
IDH: Isocitrate Dehydrogenase; INR: International Normalized Ratio; MGMT: O6-methylguanine DNA Methyltransferase; MRI: Magnetic Resonance Imaging; PTT: Partial Thromboplastin Time; WHO: World Health Organization
The incidence of gliomas in pregnant women is low and management is still based on small case series and expert opinions [1,2]. However, advances in treatment and better quality of life have led to an increase in women with gliomas who become pregnant. We know that there are interactions between pregnancy and brain gliomas, but the exact relationship is poorly understood. Pregnancy can modify tumor behavior with increased tumor growth, increased frequency of seizures, and anaplastic transformation [2-5]. In contrast, acute growth of a glioma during pregnancy due to intratumoral hemorrhage is an exceptional occurrence. While the hemorrhagic infarction of a glioma is not uncommon, if it occurs during pregnancy we face a lack of knowledge on the management strategy and on the possible clinical results.
We report the case of a pregnant woman presenting with acute neurologic deterioration due to the hemorrhagic infarction of a newly discovered anaplastic astrocytoma, treated with an urgent craniotomy. To the best of our knowledge, this is the first description of an urgent resection of a hemorrhagic glioma in a pregnant woman. The clinical evolution was good despite its potentially catastrophic presentation.
A 33-year-old woman in the 34th week of pregnancy presented with a mild left leg weakness. She was admitted to the Neurological division of our hospital. MRI scan of the brain showed a right rolandic lesion that extended to the middle third of corpus callosum and thalamic region, with a contrast-enhancing nodule, without spectroscopic evidence of necrosis (Figure 1). Two days after, the patient suddenly presented with a complete left hemiplegia. A second urgent MRI showed a dramatic increase in tumor volume due to intralesional hemorrhage (Figure 2). INR, PTT and platelet count were in normal ranges and the patient did not use antiplatelet drugs.
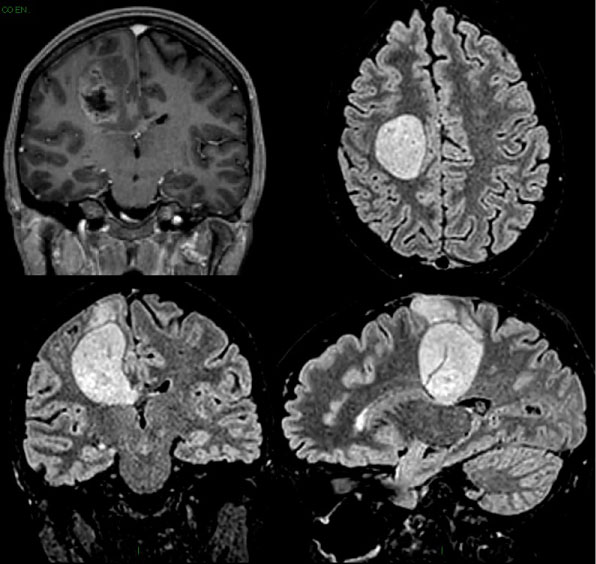 Figure 1: MRI performed at the onset of hemiparesis.
View Figure 1
Figure 1: MRI performed at the onset of hemiparesis.
View Figure 1
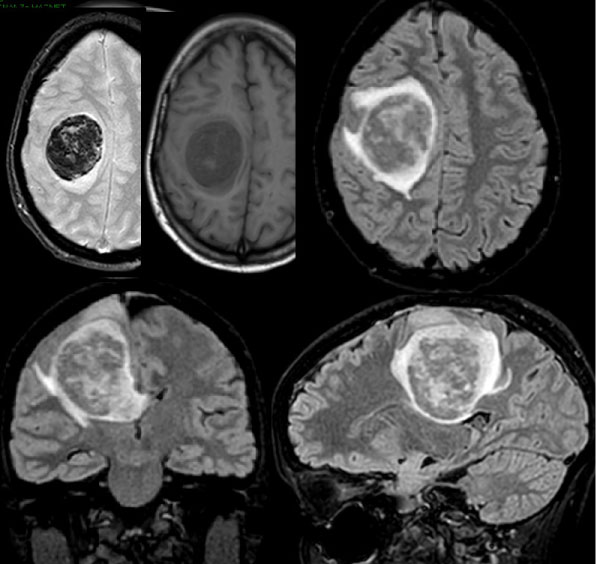 Figure 2: Second MRI, performed two days later, showing the hemorrhagic infarction of the previously diagnosed glioma.
View Figure 2
Figure 2: Second MRI, performed two days later, showing the hemorrhagic infarction of the previously diagnosed glioma.
View Figure 2
In agreement with our gynecologists we chose to anticipate the delivery with a cesarean section and then perform the craniotomy. The preterm delivery did not present any complications to the fetus. A few hours after, in the absence of maternal complications, we performed a craniotomy to relieve the mass effect.
The surgery was performed under general anesthesia. A small corticectomy in the hypovascular and edematous postcentral gyrus allowed us to reach the subcortical hematoma at a depth of about 1 cm. After suction of the blood clot we found a pathological tissue similar to a low-grade glioma with hemorrhagic infarction, extending deeply through the corpus callosum towards the right thalamus and progressively losing a cleavage plane. The pathological tissue was poorly vascularized and in the middle of the mass we found an extensively thrombosed deep vein. We did not continue the resection further in order to avoid inducing new deficits, not having performed a functional mapping and having achieved a good decompression.
The preoperative hemiplegia improved in a slight hemiparesis. The left foot maintained a mild deficit of extension and extrarotation, but the patient was able to walk. There were no significant sensory deficits and cognitive functioning was almost intact. Postoperative MRI showed a subtotal resection, with a residual enhancing nodule in the deepest part of the surgical cavity, between the deep portion of corpus callosum and the thalamus. Histopathological examination diagnosed an anaplastic astrocytoma, WHO grade III, IDH1 and IDH2 wild-type, with MGMT promoter methylation.
We performed adjuvant chemo-radiotherapy. The MRI performed after 6 months showed the complete disappearance of the enhancing tumor residue. One year after the initial presentation the patient has a good quality of life; the child is healthy and the mother is able to take care of him. The follow-up is still ongoing.
Pregnancy can be a critical period in women harboring a brain glioma. Although evidence-based guidelines have yet to be developed, some systematic reviews have been conducted. Previous studies have shown that, on the one hand, pregnancy does not influence the risk of developing "ex novo" a glioma [2,6]. On the other hand, pregnancy can modify the biological behavior of gliomas and correlates with increasing tumor volume and growth rate, and anaplastic transformation of lower grade gliomas [2-4]. Tumor progression in grade II-III gliomas can reach 44% of cases during or immediately after pregnancy [5]. A recent multicenter retrospective study based on 52 patients confirmed the link between pregnancy and glioma growth, showing increased velocity of diametric expansion in 87% of cases and clinical deterioration in 38% [4].
If a woman already knows she is harboring a low-grade glioma, there is consensus that pregnancy can be envisioned, but the patient should be informed about the possibility of tumor growth and anaplastic progression. If pregnancy is decided, it is advisable to perform a very close follow-up with repeated MRIs with quantitative assessment of tumor growth [1,2,4-6].
Otherwise, as in our case, a previously asymptomatic glioma may be discovered during pregnancy because of the onset of seizures or neurological deficits. In these cases an urgent contrast-enhanced MRI is mandatory. Gadolinium-based contrast agents have not shown potential risk to the fetus [6]. Similar cases reported in literature usually show an anaplastic glioma rather than a low-grade glioma [2,3,6], with a possible malignant transformation during pregnancy.
The acceleration of tumor growth is documented not only in gliomas but also in meningiomas, with an increase in serum progesterone levels (progesterone receptors are expressed in 70% of meningiomas) [7]. Therefore, pregnancy may accelerate the rate of growth of meningiomas and also induce water retention and engorgement of vessels resulting in hemorrhage [3,8]. Indeed, grade II-III gliomas and meningiomas appear to be the main intracranial tumors influenced by pregnancy: other tumors, such as grade I gliomas [5] or dysembryoplastic neuroepithelial tumors [2], seem to be unaffected.
In pregnant woman in the second and third trimesters harboring a glioma, the onset of a new neurological deficit may depend, in addition to tumor growth and malignant transformation, on the increased mass due to the increase in blood volume and fluid retention [6]. In contrast, the occurrence of acute mass growth due to an intratumoral bleeding is an extremely rare event. Of note, in the multicenter study by Peeters, et al. [4], in 52 cases of gliomas in pregnant women no cases of intratumoral hemorrhage were recorded: neither in the gliomas already diagnosed before pregnancy, nor diagnosed during pregnancy. No cases of intratumoral hemorrhage were recorded by Zwinkels, et al. [6] in a review of 103 pregnancies with gliomas (either already diagnosed or newly discovered). Yokohama, et al. [9] reported repeated minor intratumoral hemorrhages in an optic nerve glioma discovered during pregnancy, treated after cesarean section.
Possible mechanisms of intratumoral bleeding in brain tumors can be an excessive endothelial cell proliferation which causes obstruction of tumor vessels and therefore hemorrhage, disruption of vessels by tumor expansion, or direct infiltration of vessels. Pregnancy itself is associated with a state of hypercoagulability and a higher risk of thromboembolism: venous thrombosis can cause a hemorrhagic infarction of a brain tumor [9]. We suppose that the latter may be the cause of hemorrhage in our patient, since we observed, during surgery, an extensively thrombosed deep vein right into hemorrhagic infarction of the tumor.
A recent systematic review by van Westrhenen, et al. [1] suggests that if a low-grade glioma is diagnosed during pregnancy, it would be ideal to postpone surgery after the gestational age of 34-36 weeks. In the case of a high-grade glioma, on the other hand, there is no reason to delay surgery after delivery, since neurosurgical procedures do not increase maternal or fetal risks [10]. Obviously, if the acute increase in the mass effect causes a significant neurological deterioration, an urgent craniotomy is needed, either before or after delivery, depending on the gestational age. In our case, the patient was in the 34th week of pregnancy, so we preferred to perform the craniotomy just after an urgent cesarean delivery.
The purpose of the craniotomy is to lower the intracranial pressure by removing the blood clot [11]. In an urgent context there is the possibility of simply performing a decompressive hemicraniectomy and/or removal of blood clot without resecting the tumor. In our opinion, however, the tumor should be debulked or resected, thus performing the first stage of oncological treatment and avoiding a second surgery, bearing in mind that the urgent surgical planning and unfavorable intraoperative conditions often make it difficult to achieve the optimal neuro-oncological goal of maximum safe resection, with greater possibility of partial resection or postoperative deficits compared to elective surgery. The latter risk can be lowered by performing the debulking from within the hemorrhagic pathological tissue without extending to the portion of the tumor not affected by the bleeding.
Pregnancy can be a critical period in women harboring a brain glioma, because it can modify the biological behavior of gliomas. Very rarely the presentation may be hyperacute due to intratumoral bleeding: if there is a significant neurological deterioration, an urgent craniotomy may be necessary. It can be performed before delivery or after a cesarean delivery if the patient is at least in the gestational age of 34-36 weeks. The best surgical management will be defined from a larger number of cases: in this case, the choice not only to remove the clot, but also to resect the tumor, has allowed performing the first stage of oncological treatment and avoiding a second surgery. Despite a potential catastrophic onset, even the hemorrhagic presentation of a malignant brain tumor can lead to good clinical results.
No funding was received for this research.
All authors certify that they have no affiliations with or involvement in any organization or entity with any financial or non-financial interest in the subject matter or materials discussed in this manuscript.