Background: The alar plays an important role in the overall appearance and balance of the nose, and the correction of a hanging alar and alar flare/base is common in rhinoplasty, especially among East Asian patients. Insufficient narrowing of the alar width, unstable appearance, and obvious scarring after surgery are matters of concern.
Aim: This study was conducted to observe whether using an internal incision and suturing technique during surgery could improve the appearance of the alar while achieving a stable appearance postoperatively.
Methods: A retrospective chart review of 52 patients who underwent alar reduction between 2016 and 2021 was performed. The postoperative clinical outcomes of alar base reduction and hanging alar lifting were compared to the preoperative state. Patients were followed up for at least 6 months.
Results: All 52 cases showed improvement in postoperative nasal appearance, the alar width was reduced, the basal position of the alar met the aesthetic standard for the basal position of the columella, and a stable appearance was still maintained six months after surgery.
Conclusion: The internal incision and suturing technique achieved sufficient narrowing of the nasal base and lifting of a hanging alar and a stable appearance in the long-term follow-up.
EBM level: IV
Alar, Rhinoplasty, Internal incision
Rhinoplasty is often referred to as millimeter surgery, and subtle differences can lead to an unsightly appearance. An example of this is apparent in the aesthetics of the alar. Sheen and Gunter, et al. proposed the aesthetic relation of the alar and columella, where a difference of just a few millimeters can lead to significant aesthetic differences [1]. Rohrich [2] considered that a satisfying alar width should be 31-33 mm, while Eduardo Yap [3] proposed that the alar width should not exceed the intercanthal distance (ICD). However, all these studies focused on alar aesthetics in Caucasians. Many Asians have noses with a broad alar base and a hanging alar. As a result, alar base surgery that aims to create an aesthetically balanced alar base is an important supplementary surgical technique in rhinoplasty performed on Asian patients [4].
Both a wide alar base and hanging alar are related to the position of the alar base insertion into the face; therefore, the surgical correction is based on removing the excess tissue and repositioning the alar base insertion into the face [5]. The alar being in the desired position after surgery is a particular concern. In the treatment of a hanging alar, the position of the alar base should be 1 to 2 mm above the columellar base [6,7].
Ideally, in lateral view, a line should bisect equally the oblong formed by the alar rim and the inferior margin of the columella. The vertical distance between the columella-lobular angle and tip-defining points is divided in half by a horizontal line adjacent to the highest point of the alar rims (Figure 1). When the alar base is lower than the inferior portion of the columellar base, a hanging alar appears. In patients with a hanging alar, direct excision of the overdeveloped soft tissues can be performed, followed by closing of the incision. Suturing can change the shape of a hanging alar for a short time, but postoperative recurrence often occurs to some extent due to gravity and the pull of facial muscle tissue. Maintaining the ideal nasal axis orientation and ensuring a certain degree of lateral wall curvature after alar base reduction is a matter of reflection [8].
 Figure 1: In a normal alar-columellar relationship (ACR), the greatest distance from the long axis of the nostril to either the alar rim or the columella should be 1 to 2 mm. The picture on the left and the picture in the middle are under normal conditions, The picture on the right shows a hanging alar.
View Figure 1
Figure 1: In a normal alar-columellar relationship (ACR), the greatest distance from the long axis of the nostril to either the alar rim or the columella should be 1 to 2 mm. The picture on the left and the picture in the middle are under normal conditions, The picture on the right shows a hanging alar.
View Figure 1
Based on these findings, an ideal rhinoplasty procedure needs to adequately raise the alar base, prevent resagging, and achieve a stable appearance. We present our clinical experience with the internal incision and suture technique for alar base reduction and hanging alar correction. In this study, we aimed to emphasize the effectiveness of the internal incision and suture technique in alar base reduction and hanging alar correction and to compare the change in distance between each measurement point for the alar preoperatively and postoperatively.
All pre- and postoperative facial images, demographic data, measurement data, operative records, and complications were collected. Alar width was defined as the distance between the most lateral points on both alars, and the alar height was defined as the distance between the alar base and columellar base. To assess the efficacy of narrowing and raising, the mean change in alar width and the alar base height (preoperative minus postoperative) was compared. In addition, changes in the nasal axis were compared on the frontal view facial images. All the data were measured directly before and after surgery by the senior author using digital sliding calipers. Patients included in the comparative analysis were followed up for greater than or equal to 6 months after surgery to ensure the stability of the postoperative appearance. All patients were informed and signed informed consent voluntarily. This study was approved by the Ethics Committee of the Zhejiang Hospital and complied with the guidelines outlined in the declaration of Helsinki were followed. The written consent was received from all participants.
Alar lifting: The volume of soft tissue to be removed was estimated by the raising text, which was performed to identify the optimal location of the alar base. A shuttle incision was made along the base of the alar, and the width of the incision was flexible according to the extent of the alar base to be lifted. The tissues around the alar base were separated, and a 5-0 pds (polydio xanone) suture was fixed first on the periosteum on the edge of the piriform aperture and then on the lower lip of the incision, anchoring the alar base upward and medially to the periosteum of vomeroid bone; then, the suture was tightened, and the lower lip was fixed with 1-2 stitches in the same way if necessary. The fixation position was adjusted as needed so that the base of the alar was 1~2 mm above the columellar base, and the alar base was anchored on the other side in the same way. The skin was closed with 6-0 Prolene suture (polypropylene) (Figure 2).
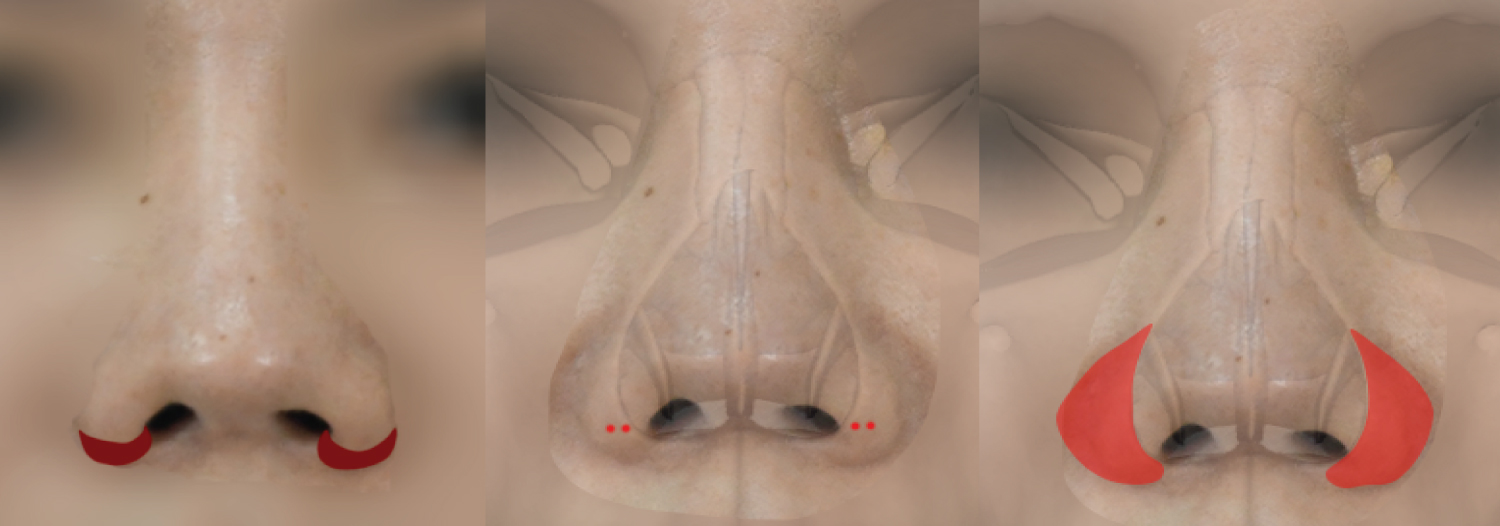 Figure 2: The left figure shows the range of the excised alar, the middle figure shows the anchor position, and the right figure shows the separated range.
View Figure 2
Figure 2: The left figure shows the range of the excised alar, the middle figure shows the anchor position, and the right figure shows the separated range.
View Figure 2
Alar narrowing: An alar wall pressure test was performed to identify the width of the incision, the extent of alar excision was marked with melanoma, a shuttle-shaped incision was made at the link between the alar and the base, the incision was sharpened into a bevel with a blade, redundant alar tissue was excised bilaterally in a wedge shape, and a small incision was made on the skin below the column. The suture needle first entered from the middle incision and passed subcutaneously to the alar incision on one side, pulled up the soft tissue and then passed subcutaneously to the middle incision. The other side was sutured in the same way, and the suture was finally sutured at the middle incision. The alar narrowed through the suture, and the tissues were pulled together.
Statistical analysis: All data were analyzed using SPSS 22.0, and continuous variables are expressed as X ± s. The independent samples t test was used for comparisons of continuous variables.
A total of 52 patients underwent surgical treatment for alar-related conditions during 2019-2021, 52 patients underwent alar base reduction and hanging alar correction, and the demographics of the patients are summarized in Table 1. There were 27 males and 25 females, of whom 21 underwent alar base reduction, 17 underwent hanging alar surgery, and 14 had lifting and narrowing together. The ages ranged from 18 to 46 years, with a mean age of 31.33 ± 7.706 years, and the follow-up time was 6-12 weeks, with a mean follow-up time of 7.267 ± 1.792 weeks.
Table 1: Demographics and clinical characteristics of patients who underwent alar surgery. View Table 1
Table 2 shows Mean Differences in Alar Width in Patients Who Underwent Alar Base Narrowing preoperatively and postoperatively. The data show that there was a significant alteration of alar width in the immediate postoperative period and at 1, 3, and 6 months postoperatively. The alar width decrease rebounded slightly in the 1-month postoperative period compared with the immediate postoperative period, but the degree was not significant; this rebound was within the range considered acceptable by the patients. The degree of postoperative narrowing was almost equal to the width of the tissue cut off after surgery (Figure 3).
Table 2: Mean differences in alar width and narrowing alar lifting. View Table 2
 Figure 3: The width of nasal alar base narrowed obviously.
View Figure 3
Figure 3: The width of nasal alar base narrowed obviously.
View Figure 3
Table 2 also shows the difference in height between the alar base and nasal column base preoperatively and postoperatively, and the data show that there was a significant alteration. The mean height of the alar base was 3.29 ± 0.69 mm higher than that of the base of the nasal column at 6 months after surgery (Figure 4).
 Figure 4: The left picture shows the hanging alar before the operation, and the right picture shows the alar base raised after the operation.
View Figure 4
Figure 4: The left picture shows the hanging alar before the operation, and the right picture shows the alar base raised after the operation.
View Figure 4
Of the 52 patients, 3 cases developed complications, which were mainly reflected in postoperative angular deformity, bilateral nostril asymmetry, and rounded and unattractive alae. The angular deformity occurred mainly at the area where the tip of the nostril joins alae, but it improved after 6 months. Patients with bilateral nostril asymmetry may undergo a second excision of the alae on the side of the larger one, and lifting of the nasal base resulting in a rounded and unsightly appearance is difficult to avoid, but these complications were mild, and neither of these patients underwent second surgery.
In these reviews, the anchoring technique provided better stability in both alar base reduction and alar lifting. The anchoring technique effectively repositioned the alar base postoperatively and achieved a stable shape 6 months after surgery. It has been proposed that the surgical solution for lateral nasal ptosis is to excise the excess vestibular skin, taking into account the retraction and gravitational stretching effect. The amount of excision should be slightly wider than the amount of ptosis but should never exceed 3 mm, as this may cause a rolling-in effect of the alar rim. Early on, we tried to design a sailing incision on the vestibular surface, the width of which was the height of the alar base lift, combined with an anchoring technique. Since the amount of lateral nasal tissue was increased by removing the vestibular tissues with longitudinal pulling sutures, the postoperative appearance tended to be "stacked" (Figure 5), producing a rounded and unattractive shape. If additional raising of the alar is necessary, the caudal aspect of the lateral crus may be trimmed to shorten the framework to promote raising of the alar. However, we recommend judicious and conservative trimming of the caudal aspect of the lateral crus precisely in the area of desired alar rim elevation. The caudal aspect of the lateral crus rarely mirrors the entire contour of the alar rim, making this technique less predictable [8]. Direct excision of the overhanging alar has also been performed without the use of the anchoring technique, which requires the removal of approximately 4 mm of tissue for every 2 mm of elevation, making it difficult to achieve satisfactory results with this surgical approach in patients with more than 2 mm of elevation.
 Figure 5: After the operation, the hanging alar was improved, but the tissue was redundant, and the alar unsightly.
View Figure 5
Figure 5: After the operation, the hanging alar was improved, but the tissue was redundant, and the alar unsightly.
View Figure 5
The anchoring technique allows the anchoring of soft tissue to hard tissue and was originally used in orthopedic surgery to provide strong attachments [8]. It was inspired by the release of orbital septal fat during eye bag surgery and the anchoring of the bulging fatty tissue to the orbital rim [9], and in alar lift surgery, excess alar tissue is directly excised and sutured; however, due to the force of muscle around the alar, skin tension, and gravity, it is easy to have a postoperative alar base lift that is not obvious. By separating the tissues around the alar base, the anatomical position of the alar base is redefined, and the tissues are riveted upward to the periosteum at the same time through a suture so that the postoperative effect is long-lasting and does not continue to droop. The base can be accurately determined during surgery. We often think about whether the base lift needs to be over raised during surgery; we found that the answer was no. The anchoring technique provides exact fixation, and the upward lift can be 1~2 mm above the base of the columellar base [10]. When suturing the incision, the depth of the suture is also a matter of concern: at first, we chose the suture point in the deeper part of the tissue and found little effect after fixation; if the position is shallow, it is easy to make a surgical incision. The effective suture depth should be near the middle position, which is not only firm but also less likely to form incision marks. Hanging alars can also be addressed by using grafts to lengthen the columella. A common problem is that if the patient has a short philtrum, the postoperative philtrum further shortening causes patient dissatisfaction, and these reasons make the surgery impossible. In such cases, the use of internal incision and anchoring is a better method.
In the past, plastic surgeons usually used sutures to close the tissue on one side of incision ‘a’, pass under the skin through the other side of incision ‘b’ to come out, suture the other side of the alar, and then return to incision ‘a’ to pull it together and tie it. We use a small incision ‘c’ taken in front of the column base, and the suture needle is passed through this incision ‘c’ to come out from both sides of ‘a’ and ‘b’, pulling together and suturing the connecting alar tissues, with the final knotting site in the middle incision ‘c’, which facilitates the suture needle being passed out under the skin. In our early surgery, the suture points on both sides of ‘a’ and ‘b’ were taken at the incision site, and it was found that the postoperative alar axis became straight and that the result was not aesthetically pleasing (Figure 6). To improve, the suture points on both sides of our ‘a’ and ‘b’ were reselected on the nasal tissue approximately 2 mm away from the pterygoid groove, which was conducive to the beautification of the pterygoid groove and the formation of an aesthetically pleasing nasal curvature (Figure 7). The skin should be mattress sutured vertically after excision to reduce skin inversion and produce unattractive "cut marks".
 Figure 6: Schematic illustration of alar excision with cinching suture (Before improvement).
View Figure 6
Figure 6: Schematic illustration of alar excision with cinching suture (Before improvement).
View Figure 6
 Figure 7: Schematic illustration of alar excision with cinching suture (After improvement).
View Figure 7
Figure 7: Schematic illustration of alar excision with cinching suture (After improvement).
View Figure 7
The advantage of an internal excision is that the scar is concealed, but for nasal wings with a vertical nasal axis, the traditional internal excision method tends to change the direction of the nasal wing axis, forming a bowling ball-like nasal wing appearance (Figure 8). The nasal axis is an important component in nasal reduction surgery [11,12]. According to the position of the vertical surface of the nasal lobules relative to the horizontal plane of the nasal base, the nasal axis can be divided into three forms: the abductor type, the vertical type and the introverted type. Normally, the nasal axis points in the downward and outward direction; if there is a patient with a vertical downward nasal axis and the contour looks toward a pair of brackets, there is a potential problem. If nasal excision and reduction are performed in this patient, the postoperative nasal shape may be distorted and have a "bowling ball" appearance in the frontal view [13,14]. In the study, for nasal wings that were also too wide in the middle, we used multipoint anchoring to narrow both the middle and the lower part of the nose to avoid the formation of an inward nasal axis (Figure 9). However, the internal incision is prone to angular deformities, and to improve it, we should improve the flap design. It is thought that the incision can be placed not at the base of the nasal wing but perpendicular to the nasal canal; however, the incision is short, and the reduction is limited. If a wider section of tissue is removed, the incision will inevitably be lengthened and produce a visible exposed scar; to prevent this, we can further design a rotational advancement flap [15,16]. In addition, the position of the nasal reduction incision should be flexibly adjusted, as this may affect the nasal and nostril aesthetics. The ideal nostril should be pear-shaped, oval-shaped, and symmetrical on both sides, and the long axis of the nostril should have a 30- to 45-degree pinch with the nasal minors. The width of the nostrils should be slightly wider than the nasal column. The width of the nasal column is about one-fifth of the width of the nasal base, and the width of the nasal base can be analyzed from the front: it should be approximately equal to the nasal spacing. The ideal width of the nasal spacing should be one-fifth of the width of the face, which is approximately the width of one eye, and slightly more for Asians [14,17,18]. According to Guyuron [19], the lateral wall of the nose is thick, the incision is close to the nasal flank, while the nostril is large, and the incision is close to the nasal canal. In people with wide nasal pedicles, the incision can be made next to the nasal pedicle, and then a penetrating suture can be made using a submerged guide technique [12] (Figure 10).
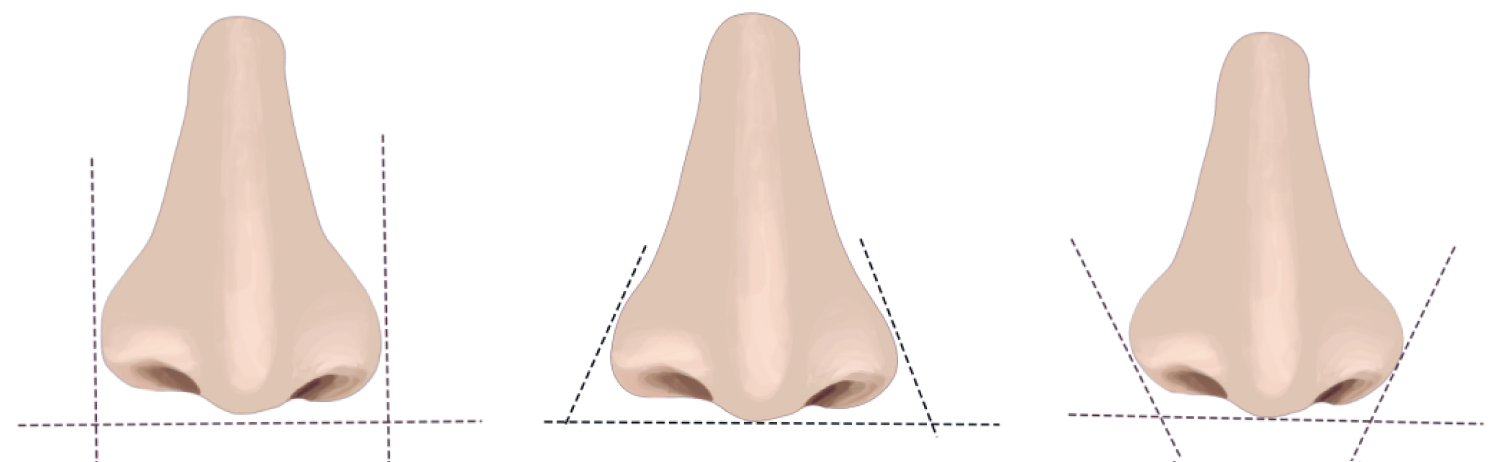 Figure 8: Illustration of the alar axis classification. (Left) Divergent, (center) straight, and (right) convergent.
View Figure 8
Figure 8: Illustration of the alar axis classification. (Left) Divergent, (center) straight, and (right) convergent.
View Figure 8
 Figure 9: There was no significant change in Alar axis after operation.
View Figure 9
Figure 9: There was no significant change in Alar axis after operation.
View Figure 9
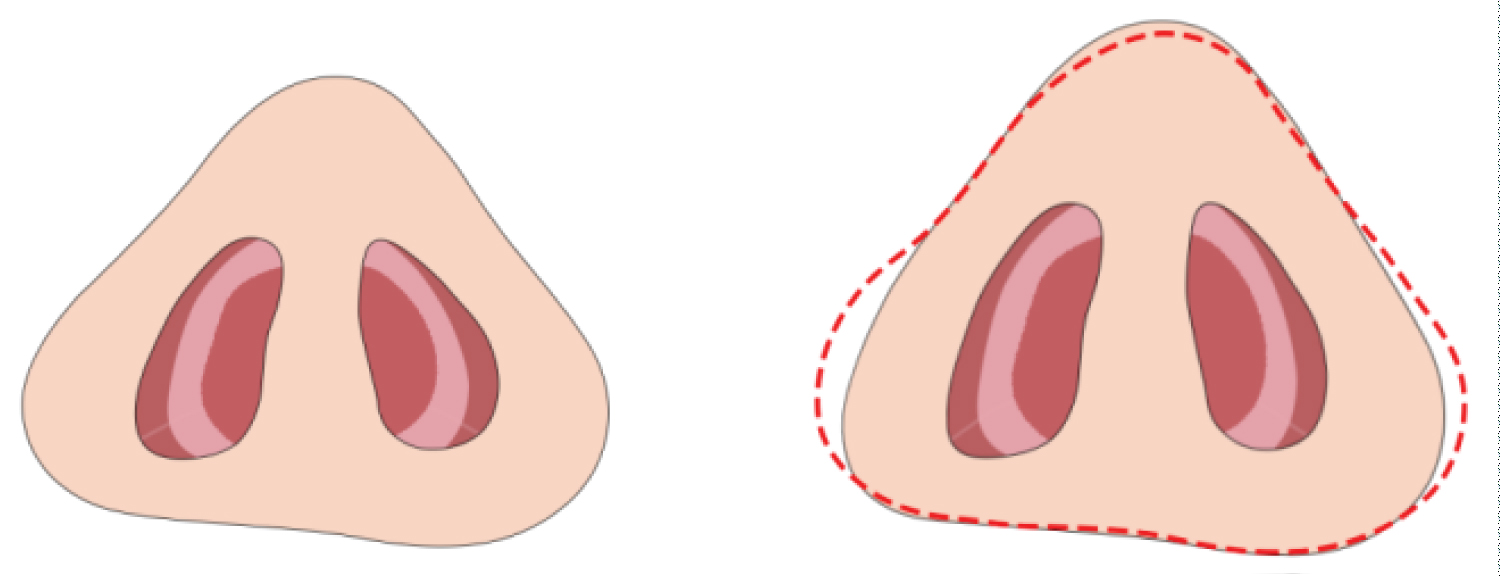 Figure 10: The figure on the left shows the alar before narrowing, and the figure on the right shows the alar after narrowing.
View Figure 10
Figure 10: The figure on the left shows the alar before narrowing, and the figure on the right shows the alar after narrowing.
View Figure 10
This study has limitations, including a small sample size and insufficient follow-up time. The next study will compare the two methods, direct excision suture and combined anchoring, to determine the optimal surgical approach for obtaining a stable result. Patient satisfaction ratings are an important way to determine surgical outcomes, and this evaluation is also underway. In addition, assessing the symmetry of the patient's nose does not only rely on frontal photographs; the symmetry of the nostrils is assessed in a three-dimensional combination of multiple angles and directions, and we change the symmetry in only one of these angles. Although there is improvement after surgery, some patients still have a slight asymmetry. It may be more appropriate to use a 3D scanning technique to observe not only the symmetry of the nostrils from multiple angles but also the dynamic changes in the nasal wings [20]. Additionally, the positioning of the various measurement points for the nasal wing at different times may be subject to error. We used photographic measurements to assess the ratio of the distance between the nasal wing and the medial canthus, and the different angles of the photographs may lead to errors. The premise of nasal base uplift is that the overall nasal length is moderately proportional to the length of the face; otherwise, uplifting the nasal tissue may visually shorten the length of the nose further and produce a constricted appearance. For patients with a short atrium or a nasolabial angle of less than 90 degrees, cartilage grafting to lengthen the nasal tuberosity is a more appropriate surgical approach [16,21,22].
Our study shows that the anchoring technique in wide nasal wings and drooping lateral nasal angles yields stable surgical results, and the anchoring technique also allows for simultaneous narrowing of the mid and lower nasal wings and beautification of the nasal axis (Figure 11 and Figure 12). In this study, subcutaneous separation and anchoring point confirmation were the keys to the success of the procedure, with subcutaneous separation allowing repositioning of the nasal base and appropriate anchoring points enabling stable postoperative results. In addition, there are strict indications for this surgery, and proper patient selection is also key to the success of the surgery. In conclusion, the use of an internal incision and anchoring technique can effectively improve nasal overhang and wide nasal deformities and achieve a stable shape after surgery. It is worth promoting its use.
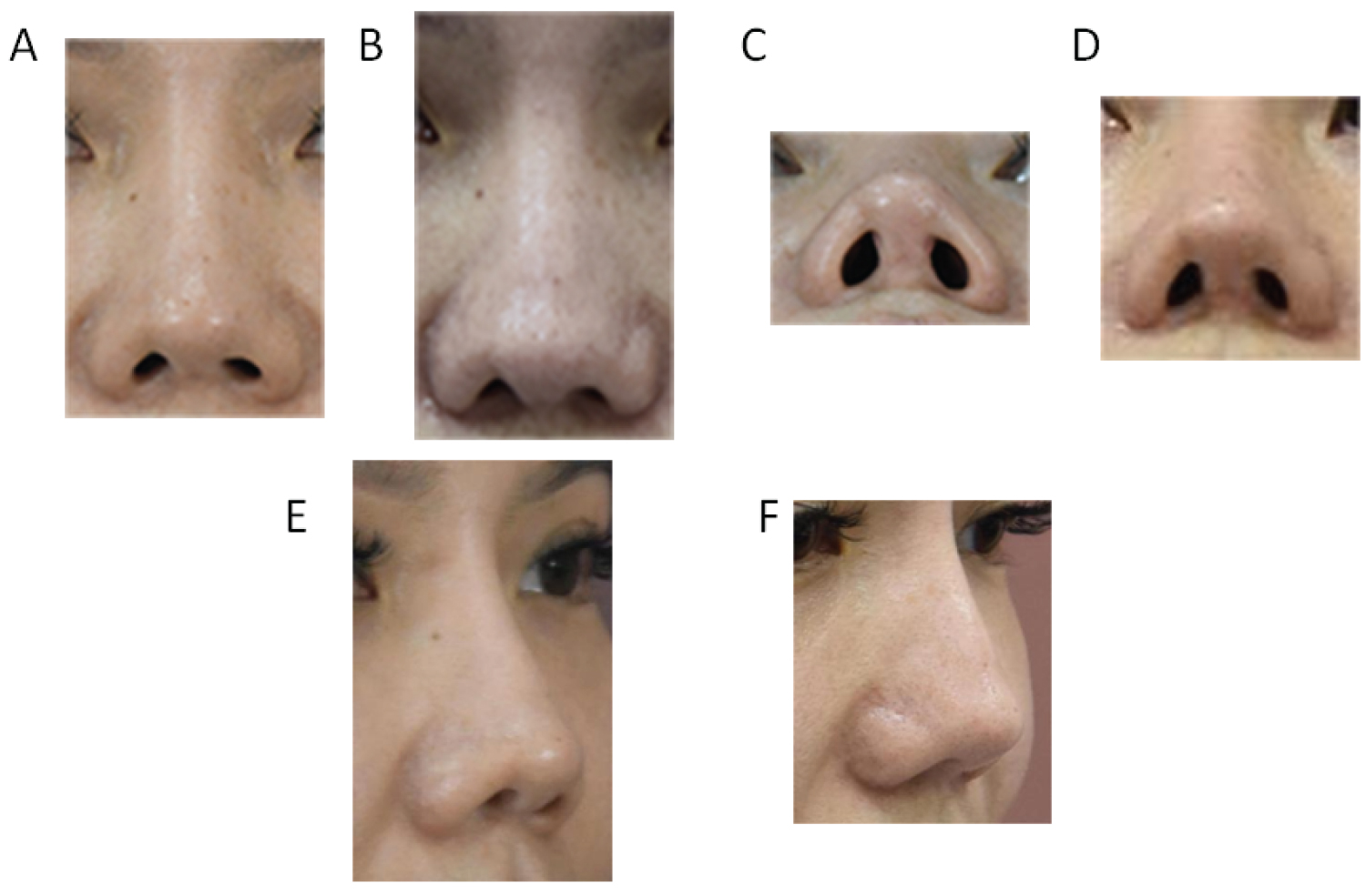 Figure 11: Preoperative and Postoperative Photographs of a 40-Year-old Female Patient (a, c, and e show the appearance of the preoperative alar, and b, d and f shows the appearance of the alar 8 months after Alar Lifting surgery).
View Figure 11
Figure 11: Preoperative and Postoperative Photographs of a 40-Year-old Female Patient (a, c, and e show the appearance of the preoperative alar, and b, d and f shows the appearance of the alar 8 months after Alar Lifting surgery).
View Figure 11
 Figure 12: Preoperative and Postoperative Photographs of a 22-Year-Old Female Patient. (a, c and e show the appearance of the preoperative alar, b, d and f shows the appearance of the alar 6 months after Alar narrowing surgery).
View Figure 12
Figure 12: Preoperative and Postoperative Photographs of a 22-Year-Old Female Patient. (a, c and e show the appearance of the preoperative alar, b, d and f shows the appearance of the alar 6 months after Alar narrowing surgery).
View Figure 12
All patients were informed and signed informed consent voluntarily. This study was approved by the Ethics Committee of the Zhejiang Hospital and complied with the guidelines outlined in the declaration of Helsinki were followed. The written consent was received from all participants.
Not applicable.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Not applicable.
None.
Xiaohui Long conceived and designed the experiments; Xiaohui Longn and Qiming Zhao performed the experiments; Qiming Zhao analyzed the data; Huahui Zhang wrote the paper. All authors have read and agreed to the published version of the manuscript.
Not applicable.
The authors declared that they have no conflicts of interest regarding this work.