Objective: This Study aimed to assess the efficacy of topical application of Mitomycin C as two doses, intraoperative and 3 weeks later, in the prevention of adhesions formation after functional endoscopic sinus surgery.
Materials and methods: A prospective randomized clinical trial conducted in Otorhinolaryngology Department, Tishreen University Hospital, Lattakia, Syria, between July 2021 and July 2022. The study included 62 patients underwent bilateral functional endoscopic sinus surgery (Fess) for chronic rhinosinusitis with or without polyps. A cotton pledget soaked with 1 ml of mitomycin C (0.8 mg/ml) was randomly applied in the middle meatus of one nasal cavity (study side) for 5 minutes and a second pledget soaked with 1 ml normal saline was applied in the contralateral side (control side) at the completion of surgery and repeated 3 weeks later.
Patients were followed for 3 months after surgery (1st week, 3rd week, 6th month, 3rd months) and assessed endoscopically for any adhesion formation and the side of it. Lund_ Kennedy endoscopic score was recorded and compared between the two sides.
Results: Adhesions were observed in 11 patients (17.74%), two patients had bilateral adhesions. 4 adhesions were in the mitomycin C side (6.45%) and 11 in the control side (17.74%) but this difference was not statistically significant (p value = 0.55). According to the endoscopic score there was a statistically significant difference between the two groups especially after the second application of mitomycin C (p value < 0.0001).
Conclusion: Topical application of Mitomycin C intra- and postoperative may reduce the incidence of adhesions after functional endoscopic sinus surgery in the dose used in our study and improve the mucosal healing.
Functional endoscopic sinus surgery, Mucosal healing, Mitomycin C, Adhesions
Functional endoscopic sinus surgery (FESS) has been accepted as the choice of treatment modality for chronic sinus diseases, and it has not only become minimally invasive by changing the access of surgery but has also switched to the aim of respecting the normal physiology of the nose and sinuses and preservation of the normal mucosa [1]. The primary surgery represents the patient’s greatest chance for long-term success when accompanied by medical treatment and appropriate postoperative care [2], but despite its established efficacy, there still be cases of persistence or recurrence of symptoms which may need revision surgery. Among the recurrence causes, osteal stenosis and adhesion formation appear to be the most frequent [3].
Adhesions formation is one of the most common complications after nasal surgeries. Previous studies have noted that it’s the most common complication after functional endoscopic sinus surgery by an incidence rate between 10-40%. Ramadan noted that 56% of patients who undergoing revision endoscopic sinus surgery had adhesions [3].
Mitomycin C (MMC) is an antineoplastic antibiotic isolated from the broth of streptomyces caespitosus , and acts as an alkylating agent able to inhibit DNA synthesis and was used as chemotherapeutic agent by inhibiting cellular mitosis [4]. Preclinical studies have demonstrated that topical application of mitomycin C on cultured fibroblasts for 5 minutes has an antiproliferative effect for about 30 days in concentration starts in 0.04 mg/ml, but has a cytocidal effect in concentration of 1 mg/ml [5]. Regarding its effect on epithelial cells, mitomycin C in these concentrations may affect proliferation and migration of epithelium but for a shorter period of time, normal epithelium regrowth was noted after 1 to 2 weeks of mitomycin C application [6].
The first clinical application of mitomycin C was in ophthalmology, it has reduced recurrence rate after pterygium surgery with remarkable results [7]. Its usage in ophthalmology has extended to include glaucoma, strabismus, optic nerve decompression, and dacryocystorhinostomy surgeries [8].
In upper aerodigestive tracts surgeries, mitomycin C was studied as an adjuvant treatment that prevent fibrosis and restenosis, such as surgery of laryngotracheal or esophageal stenosis repair [9], choanal atresia repair.
Studies of mitomycin C In preventing adhesions formation and osteal restenosis after Fess had controversial results, a vast majority of these studies assessed a single application of mitomycin C at the time of surgery with a difference in concentrations, and its effect has most noted in the early postoperative period. So, in our study we assessed the efficacy of mitomycin C (0.8 mg/ml) as two doses intra and post-operative in preventing adhesion formation and improving mucosal healing.
Assess the efficacy of topical application of Mitomycin C as two doses, intraoperative and 3 weeks later, in the prevention of adhesions formation after functional endoscopic sinus surgery.
1. Assess of mitomycin C efficacy in preventing adhesions according to the absence and presence of polyps.
2. Assess of mitomycin C efficacy in improvement of postoperative mucosal healing.
Prospective Randomized Controlled Trial.
The study was conducted in the Department of Otorhinolaryngology and Head and Neck Surgery, Tishreen University Hospital, Lattakia, Syria from July 2021 to July 2022.
A total of 62 patients were involved in this study.
Since Mitomycin C was applied topically in one nasal side and the other side was served as control by application of normal saline, then sample size was 124.
With respect that the effect of Mitomycin C is topical in this concentration, method and time of application.
All patients diagnosed with chronic rhinosinusitis with or without nasal polyps (proven by radiologic and\or endoscopic examination), who didn’t respond to medical treatment and were admitted to undergo functional endoscopic sinus surgery, and they were 80 patients.
1. Patients who underwent unilateral Fess.
2. History of Previous sinonasal surgery.
3. History of Previous radiotherapy on head and neck region.
4. History of systemic diseases: cystic fibrosis, diabetes, immune deficiency.
5. Patients who are taking any long-acting systemic steroid.
According to this we had to exclude 10 patients, and from the rest 70 patients there were 8 patients who lost to follow up after one month and they were excluded, thus it was remained 62 patients.
- We have taken a full history including the main complaints with their severity and duration, and the past history of any chronic disease, surgery, allergic reaction, medical treatments.
- General examination with CXR, ECG and laboratory tests were done.
- Full ENT examination with anterior rhinoscop (using rigid endoscope 0° or 30° and 4 mm diameter).
- Computed tomography without contrast for nose and paranasal sinuses was done in coronal, sagittal and axial views, and the findings were subjected according to Lund Mackay CT score.
- Written Informed consent was taken from all the patients for the planned procedure in a perform approved by our institutional ethical committee.
- All surgeries were done under general anesthesia with control of systemic blood pressure.
- After injecting appropriate topical decongestive, the procedure was performed by messerklinger technique and the extent of it was according to the amount and extent of the disease of each patient.
- When there was an important septal deviation, an endoscopic septoplasty was done, with partial inferior turbinectomy when hypertrophic.
- At the completion of procedure and after an appropriate hemostasis, a cotton pledget soaked with 1 ml of mitomycin C (0.8 mg\ml) was applied in the middle meatus of one of the nasal cavities, and another pledget soaked with normal saline was applied in the middle meatus of the other nasal side. This methodology was useful to avoid bias as each patient served as his or her own control. After 5 minutes the pledgets were removed and nasal cavities were irrigated with 30 ml of normal saline.
- The side of mitomycin C application was selected randomly, and the place of application was between the middle concha and lateral nasal wall, being in direct contact with the lateral side of the concha and the extent of surgical procedure (ethmoidal infundibulum, anterior ethmoids, posterior ethmoids), we didn’t put any other splints or pledgets in the middle meatus.
- After hours of surgeries patients were discharged with a course of oral antibiotics, analgesics, nasal spray of normal saline without any systemic or nasal steroids.
Postoperative
- Patients were followed for 3 months period which included 4 visits conducted at the end of (1 st week, 3 rd week, 6 th week, 3 rd month).
- In every follow-up, Meticulous nasal endoscopic assessment was performed under local anesthesia with report of any adhesion in the middle meatus and the side of it. Debridement for severe crusts and clots was also done.
- Endoscopic findings were subjected according to Lund Kennedy endoscopic score.
- The mitomycin C application was repeated in the same side of the nose three weeks postoperatively under local anesthesia and with the use of an endoscope. The contralateral side received again a cottonoid soaked with normal saline.
- Simple adhesions were divided in the clinic under local anesthesia, severe adhesions which found in only two nasal sides were divided under general anesthesia with appropriate hemostasis, and a small merocel pack saturated with antibiotic ointment was applied and then removed the next day.
Statistical analysis
- Data were entered, checked, and analyzed using Microsoft Excel 2019.
- X 2 (chi-squared) was used for difference between qualitative variables.
- T-student was used for difference between quantitative variables.
- This study was conducted on 62 patients, 39 (62.9%) were men, and 23 (37.1%) were women. The age ranged from 21 to 55 years (mean age = 39.89 ±5 years). The majority of patients (40.32%) were in the 4 th decade of age. Among 62 patients, 38 (61.29%) had chronic rhinosinusitis without polyps CRSsNP and 24 (38.71%) had chronic rhinosinusitis with polyps CRSwNP.
- Preoperative CT score ranged from 4 to 22, from 2 to 11 in each side with a mean of 5.9 ±4 in mitomycin C side, and 5.67 ± 2.3 in control side, without any statistically significant.
- Totally at the end of follow up period, adhesions had been observed in 11 patients (17.74%), 4 patients had adhesions in both nasal sides .4 adhesions were in mitomycin C side (6.45%), and 11 in control side (17.74%) With a difference close to statistically significant but didn’t reach it (p value = 0.055) (Table 1).
Table 1: Incidence of postoperative adhesions in follow-up visits. View Table 1
- Among 24 patients who had CRSwNP, adhesions were found in 6 patients, one of them had bilateral adhesions, 1 adhesion developed in mitomycin C side and 7 were in control side with a statistically significant difference (p value = 0.02) (Figure 1).
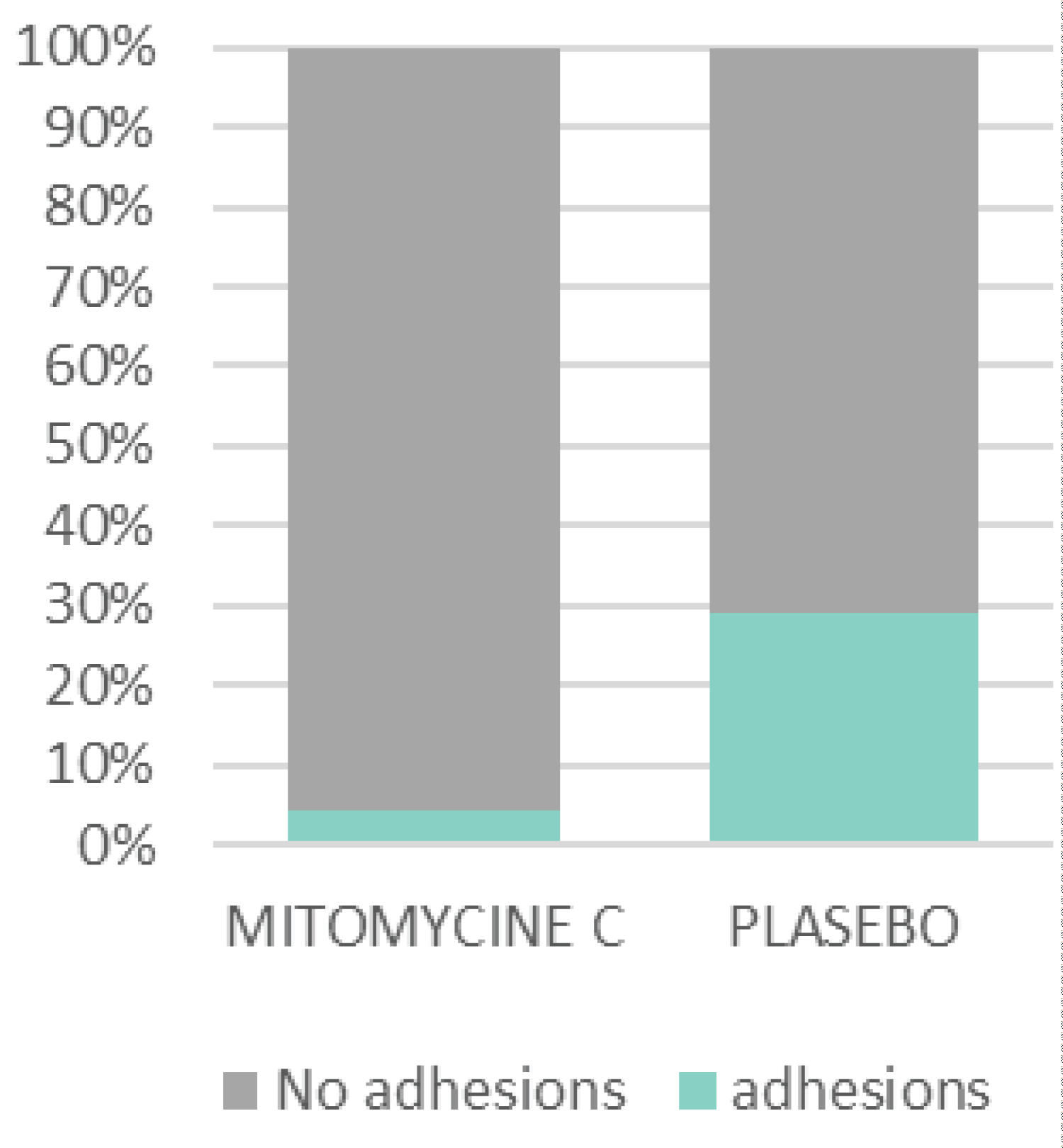 Figure 1: Adhesions rate in patients with Chronic rhinosinusitis with nasal polyps.
View Figure 1
Figure 1: Adhesions rate in patients with Chronic rhinosinusitis with nasal polyps.
View Figure 1
- Among 38 patients who had CRSsNP, adhesions were found in 5 patients, one of them had bilateral adhesions, 3 adhesions developed in mitomycin C side and 4 were in control side without a statistically significant difference (p value = 0.7) (Figure 2).
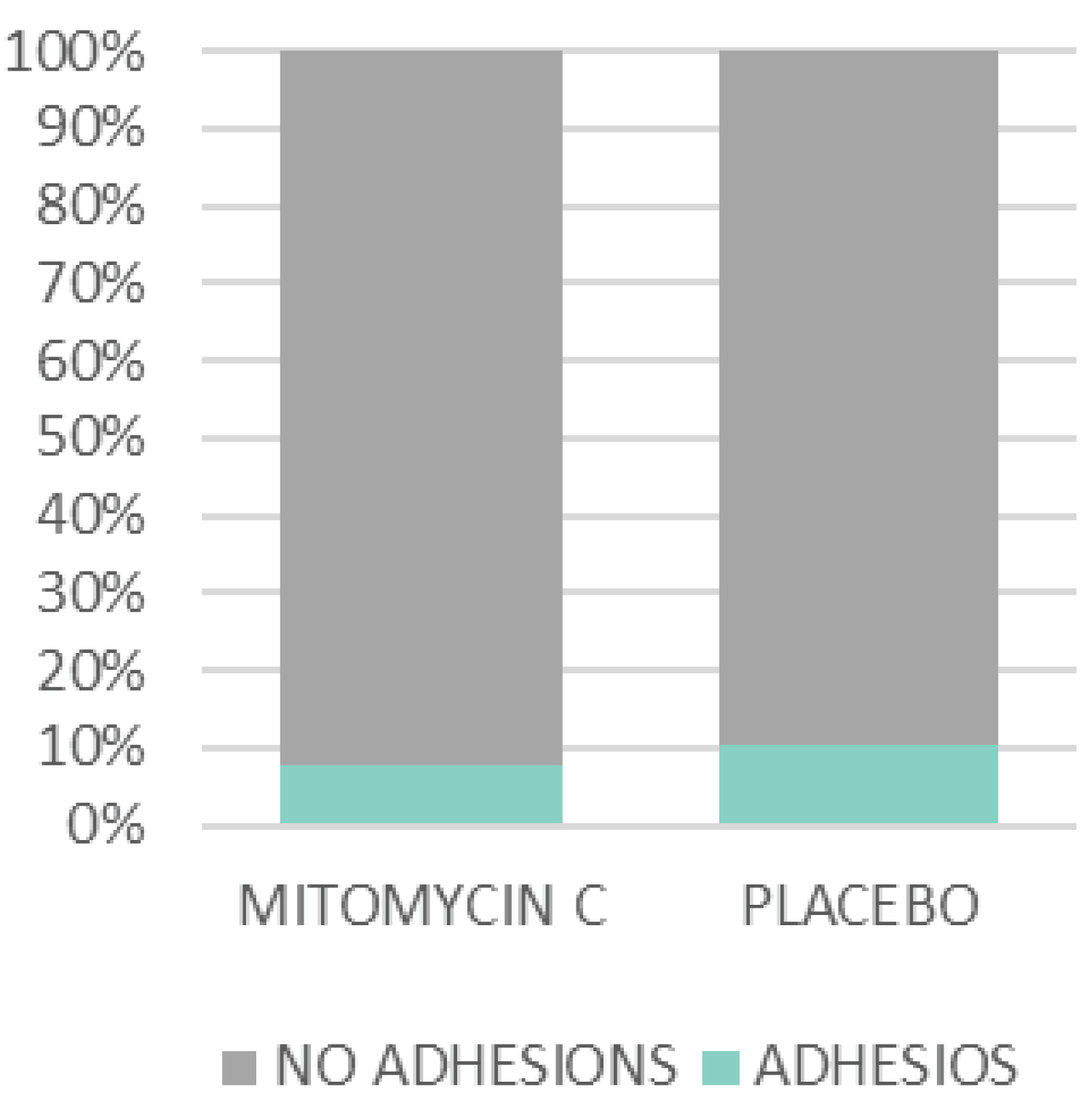 Figure 2: Adhesions rate in patients with Chronic rhinosinusitis without nasal polyps.
View Figure 2
Figure 2: Adhesions rate in patients with Chronic rhinosinusitis without nasal polyps.
View Figure 2
- The difference in mean endoscopic score between mitomycin C side and control side was statistically significant in all follow-up visits especially after the second application of mitomycin C (Figure 3)
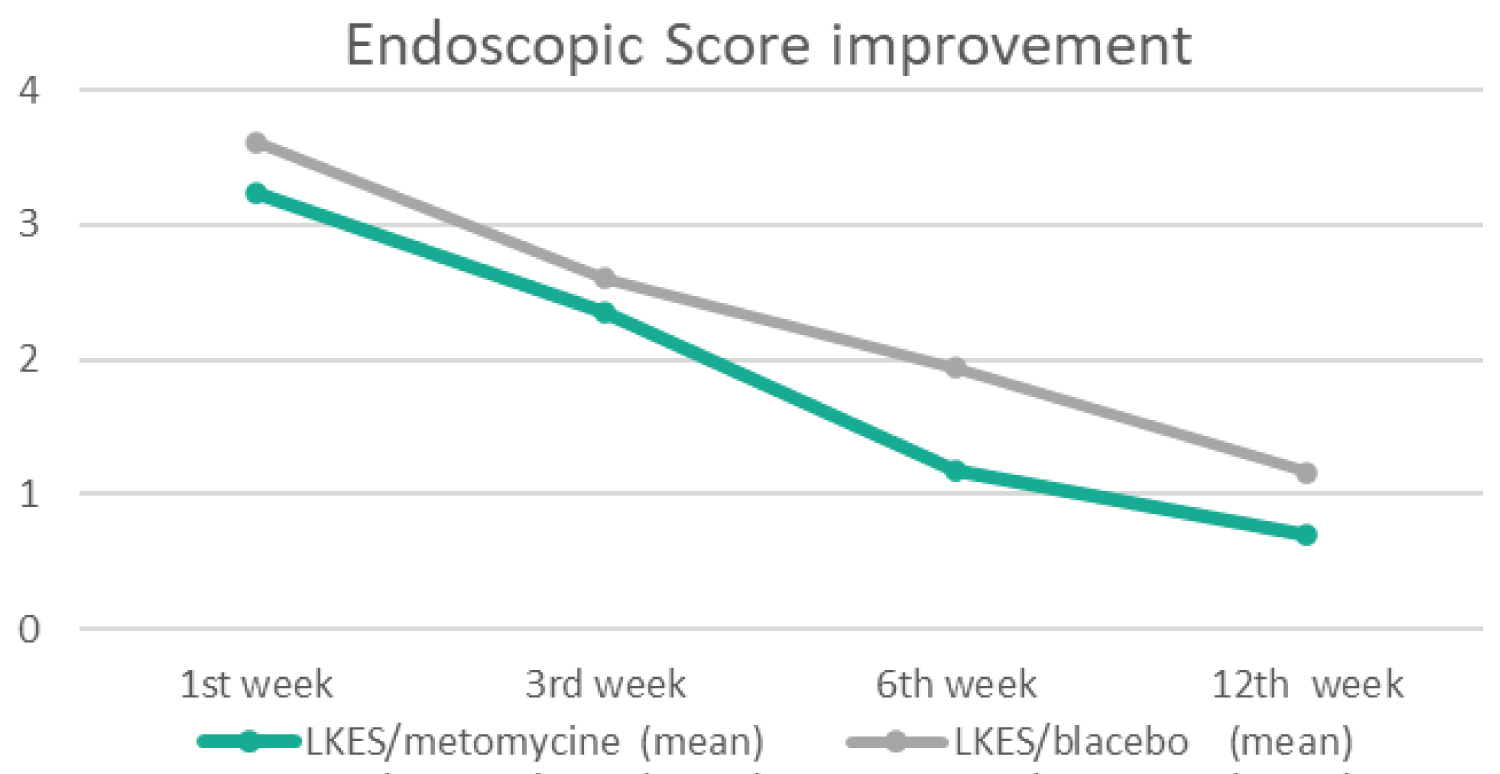 Figure 3: Comparison of postoperative mean endoscopic score between the two study sides (groups).
View Figure 3
Figure 3: Comparison of postoperative mean endoscopic score between the two study sides (groups).
View Figure 3
- 1 week postoperative it was 3.23 ± 9 in mitomycin C side, and 3.58 ± 1 in control side (p value = 0.02). 3 weeks postoperative it was 2.35 ± 0.7 in mitomycin C sides and 2.6 ± 0.8 in control sides (p value = 0.03). 6 weeks postoperative 1.18 ± 0.7 in mitomycin C side and 2.06 ± 0.9 (p value < 0.0001). And at the end of follow-up period, it was 0.71 ± 0.9 in mitomycin C side and 1.16 ± 1.2 in control side (p value = 0.001).
Functional Endoscopic sinus surgery has gained impressive popularity in dealing with chronic paranasal sinus diseases. The persistence or recurrence of symptoms even after multiple sinus surgeries is still a big challenge, blockage of sinus ostium and mucosal hypersensitivity are the two common causes of recurrence, nearly half of patients who have need revision surgery had adhesions [3].
Prevention of adhesion formation starts preoperative with good preparation of patients. In the operative room, meticulous removal of bone splinter and avoiding mucosal stripping will help to avoid adhesion formation. Also, appropriate postoperative care by delicate debridement of crusts and clots and nasal wash has an important role in prevention of adhesions.
For reducing the adhesions formation, several measures have been attempted [10], they had limited success with undesirable side effects for some. Bolgerisation or middle turbinate conchopexy were found to reduce the incidence of adhesions but iatrogenic hyposmia is a potential concern raised. Middle meatal splints placement was found to be effective with secondary outcomes include post-operative facial pain, nasal obstruction and bleeding.
In addition to be an antibiotic and antineoplastic agent, mitomycin C was known to have an antifibrotic effect by inhibiting fibroblasts proliferation and increasing their apoptosis [5]. Because of this property, topical application of mitomycin C was studied as an adjuvant treatment to upper aerodigestive tracts surgeries to prevent scars and adhesions formation or restenosis of hollow organs [8]. It had promising results.
In functional endoscopic sinus surgery, mitomycin C was studied to assess its efficacy in preventing adhesion formation and restenosis of sinus ostium, and the results were controversial, that may because of the single application of mitomycin C in the vast majority of studies, or the low concentrations in some.
In our study we assessed the efficacy of mitomycin C (0.8 mg/ml) as two doses topical application, the first was intraoperative and the second three weeks later, based on the fact that although postoperative wound healing is a long and complex process, but the most important period is the first 6 to 8 weeks [11].
Our study showed that topical application of mitomycin C in this concentration and two doses has decreased the incidence of adhesions formation in the middle meatus after FESS, the possible reason we didn’t reach the statistical importance is sample size, or that the incidence rate of adhesions was low in both groups, and that because of good surgical techniques conducted by our professors with delicate instrumentation and preserving of mucosa.
In this study we observed a statistically significant difference in adhesions formation between mitomycin C side and placebo side in patients with nasal polyposis, and that may because of its effect in down-regulation of the immunologic biomarkers which known to have higher expression in nasal polyp mucosal tissue, and known to have a profibrotic role [12,13]. Statistically significant differences were found in Endoscopic score between the two groups in all follow-up visits. Crusts, edema and fibrosis were less in mitomycin C group compared to control group.
Kim ST, et al. [14] studied the effect of single application of mitomycin C (0.4 mg/ml) at the end of surgery on the size of antrostomy, their study showed a short-term effect in maintaining the patency of antrostomy during the first month postoperative but no effect was found in long-term follow-up, and that because of low concentration (0.4 mg/ml), single dose application, or small sample size (20 patients). Yamaoka WY, et al. [15] studied mitomycin C application in a concentration of 1 mg/ml on 14 patients at the end of fess surgery, patients were followed up for a year, adhesions incidence was 21.43% in mitomycin C side and 64.29% in control side, and hence it decreased adhesions formation, and severe adhesions compared to control. However, very small sample size might be the reason they didn’t reach the statistically significant difference. Harugop, et al. [16], and Krishnan, et al. [17] found a statistically important difference in decreasing adhesions formation between mitomycin C and control groups when applying it topically intraoperative as concentrations of 0.4 and 0.5 mg/ml respectively.
Some previous studies have referred to the mitomycin C positive effects on mucosal healing, but without recording scores like our study, and without studying the efficacy according to sinusitis phenotype or histopathologic type [18].
The results of our study showed that topical application of mitomycin C (0.8 mg/ml) as two doses intraoperative and 3 weeks later may decrease adhesions formation after functional endoscopic sinus surgery especially for severe cases like patients who have polyposis, in addition to its effect in improvement of nasal mucosal healing after surgery. More researches are needed on a large number of polypoid patients with studying of healing and recurrence rate.
We wish to thank all medical staff in Otorhinolaryngology Department at Tishreen University Hospital for their hard work even with hard circumstances and great difficulties.
None.
The authors declare that they have no conflict of interest.