Introduction: Mucoceles originating from supraorbital ethmoid cells are difficult to treat. Due to its lateral location the endonasal approach with endoscopes is sometimes not sufficient to achieve adequate exposure and the use of extended transnasal techniques and even external approaches is required.
Objectives: To determine the success rate of surgical treatment performed endonasally with endoscopes or combined, endonasal and trough a transpalpebral approach to treat mucoceles originating in supraorbital cells.
Methods: Patients with mucoceles originating in supraorbital cells were treated using endonasal extended approaches to the frontal sinus and external transpalpebral approach with fat obliteration of the supraorbital cell cavity. Endoscopes were used in all.
Results: Four patients had mucoceles located in supraorbital cells. All had erosion of the anterior and inferior wall of the supraorbital cell and entered the orbit, one also had erosion of the posterior wall and the mucocele capsule contacted the meningeal.
The disease was resolved in all four patients, but in two of them it was necessary to perform a new combined endonasal and transpalpebral approach, with fat obliteration of the supraorbital cell due to recurrence of the mucocele.
Conclusions: The success rate with primary and revision surgery in patients treated by mucoceles located in supraorbital cells was 100%.
Mucosal resection, bone drilling, and supraorbital cell obliteration with fat are part of a treatment algorithm, representing the point of greatest surgical aggressiveness.
Mucoceles, Supraorbitalcell, Endoscopic surgery, Transpalpebral, Obliteration
Mucoceles are pseudotumors with mucous or mucopurulent content, which can originate in the paranasal sinuses or in isolated ethmoid cells.
Supraorbital cells are anterior ethmoidal cells that invade the frontal orbital plate [1].
Obstruction of the drainage of a supraorbital cell can cause a mucocele, and in 10% of endoscopic revision surgeries can be found unopened [2].
Due to its location, the surgical approach to the supraorbital cells can be difficult and involve the management of different endonasal and external surgical techniques.
The aim of the present study is to determinate the success rate of the treatment the mucoceles located in supraorbital cells by endonasal or combined endonasal and transpalpebral approaches.
Through the review of the electronic medical records, the patients who underwent endonasal surgery with endoscopes and combined, endonasal and transpalpebral approaches for suffering mucoceles located in supraorbital cells were selected.
Mucoceles originating in the frontal sinus were excluded from the study. The surgeries were performed in the Rhinosinusology Section of the Otorhinolaryngology Service of the Hospital Italianoin Buenos Aires from March 2010 and January 2018.
All patients were evaluated by ENT examination, nasal endoscopy, computed tomography, and magnetic resonance imaging. The surgeries were performed under general anesthesia, with endoscopes of 0° and 30°.
Neuronavigation with an optical system was used in one. The endonasal surgical techniques used were different.
In the first patient operated on in 2010, a uncinectomy, middle maxillary antrostomy, ethmoidectomy, and a Draf II-B frontal sinus drainage (unilateral drainage of the frontal sinus, between the papyracea lamina of the orbit and the nasal septum) were performed. With the 30° endoscope the medial wall of the supraorbital cell was visualized and resected marsupializing the cavity to the frontal sinus (Figure 1).
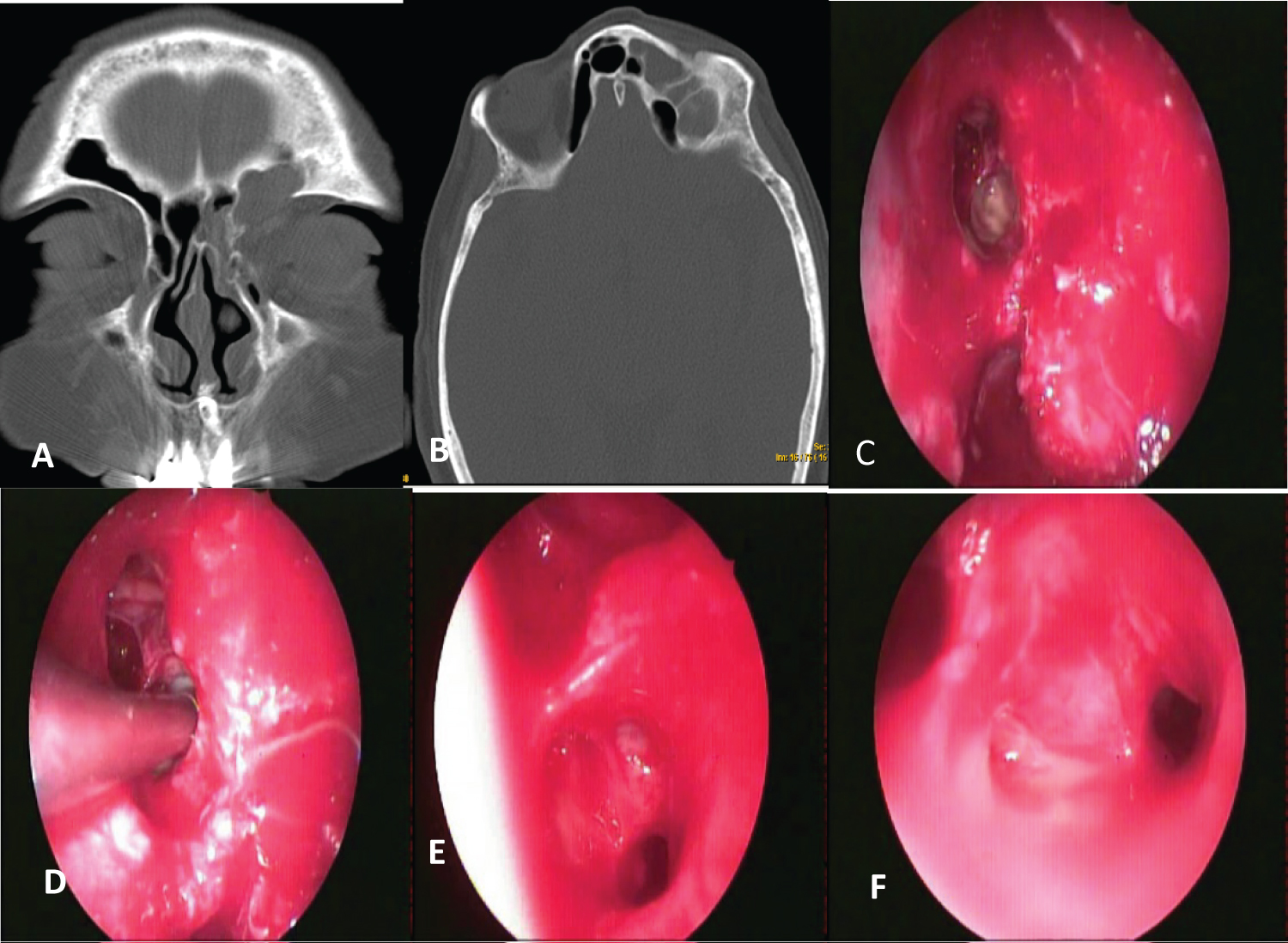 Figure 1: Supraorbital cell mucocele (A,B) Coronal and axial CT; (C) Orbital fat bulging into nasal cavity (arrow), due to previous surgery for chronic sinusitis; (D,E,F) Draf II-B and supraorbital cell marsupialization to frontal sinus.
View Figure 1
Figure 1: Supraorbital cell mucocele (A,B) Coronal and axial CT; (C) Orbital fat bulging into nasal cavity (arrow), due to previous surgery for chronic sinusitis; (D,E,F) Draf II-B and supraorbital cell marsupialization to frontal sinus.
View Figure 1
In another a Draf III or Lothrop modified frontal drainage was performed (bilateral frontal drainage between both papyraceas laminas of the orbits, with anterosuperior septectomy), and the supraorbital cell could be communicated to the frontal sinus (Figure 2).
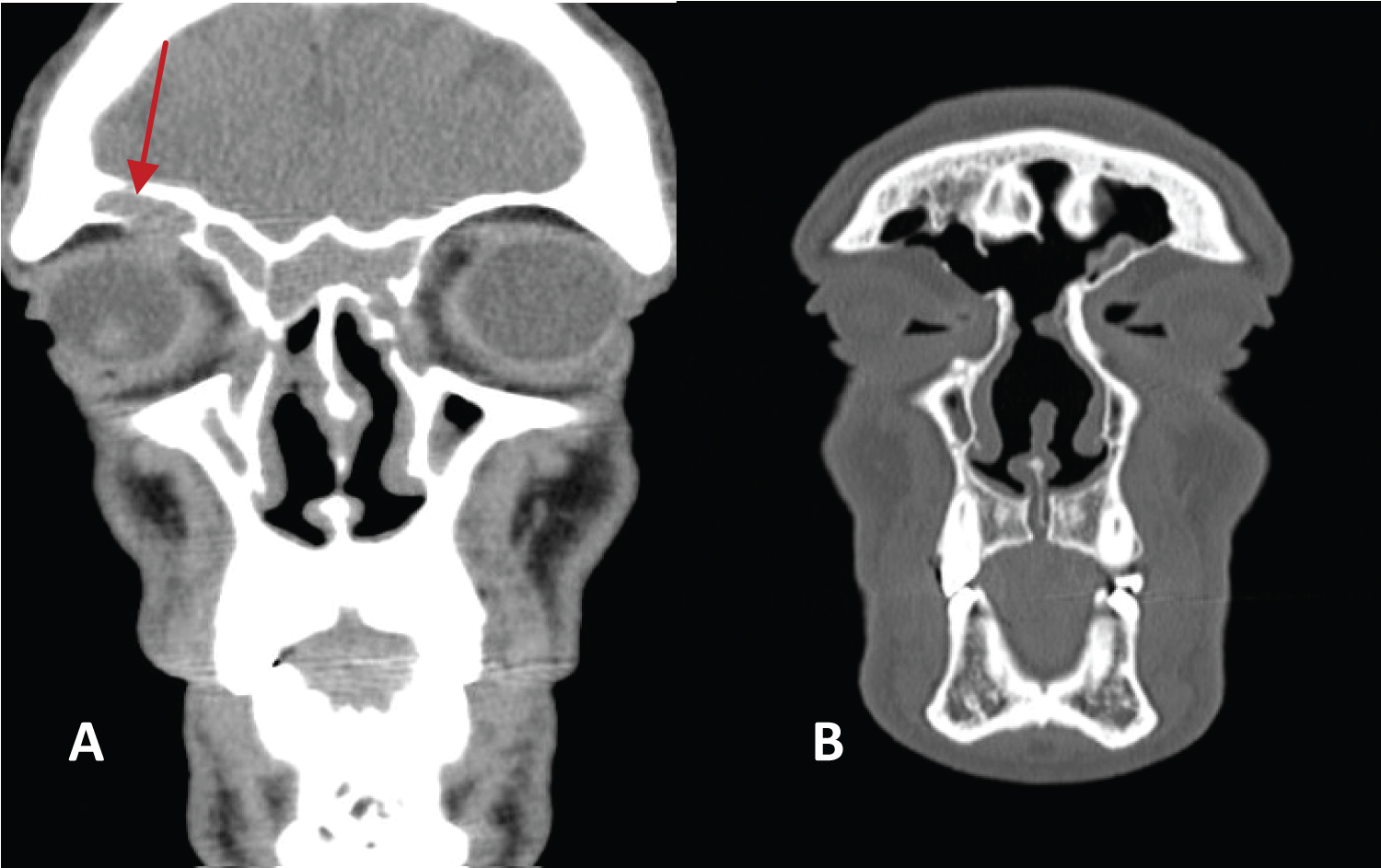 Figure 2: A) CT where mucocele is seen in a supraorbital cell (arrow); B) Posoperative CT after performing a modified Lothrop approach.
View Figure 2
Figure 2: A) CT where mucocele is seen in a supraorbital cell (arrow); B) Posoperative CT after performing a modified Lothrop approach.
View Figure 2
In two other patients a Draf II-B and modified Lothrop frontal drainage were performed, combined with an external transpalpebral approach a through a 2 cm incision.
The mucosa of the supraorbital cell was resected, the bone was drilled with a diamond bur and the supraorbital cell cavity only was obliterated with fat (Figure 3 and Figure 4).
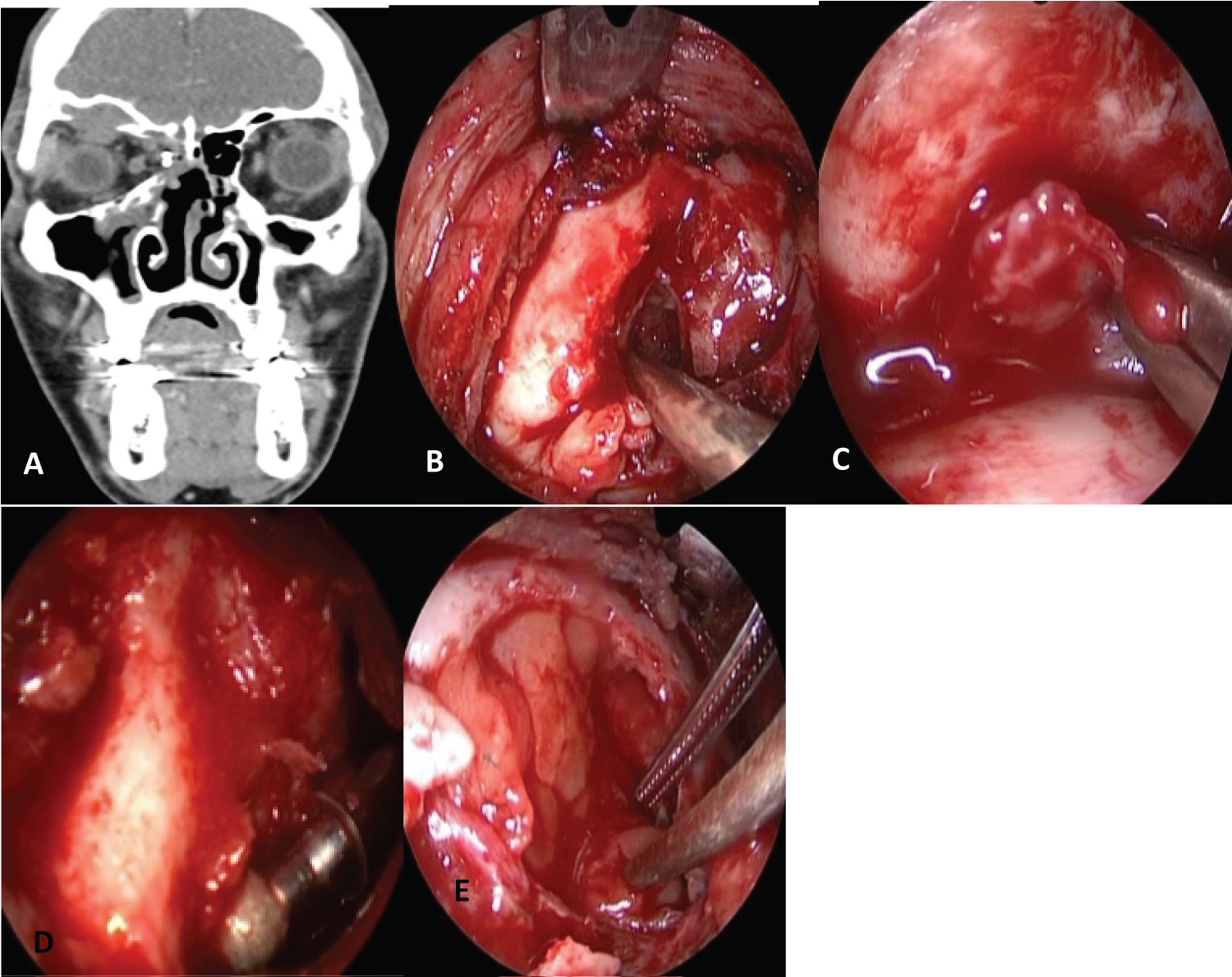 Figure 3: A) CT: Supraorbital cell mucocele; B) Transpalpebral approach; C) Resection of the mucosa of the supraorbital cell; D) Drilled of the bone; E) Fat obliteration of supraorbital cell cavity (miniobliteration).
View Figure 3
Figure 3: A) CT: Supraorbital cell mucocele; B) Transpalpebral approach; C) Resection of the mucosa of the supraorbital cell; D) Drilled of the bone; E) Fat obliteration of supraorbital cell cavity (miniobliteration).
View Figure 3
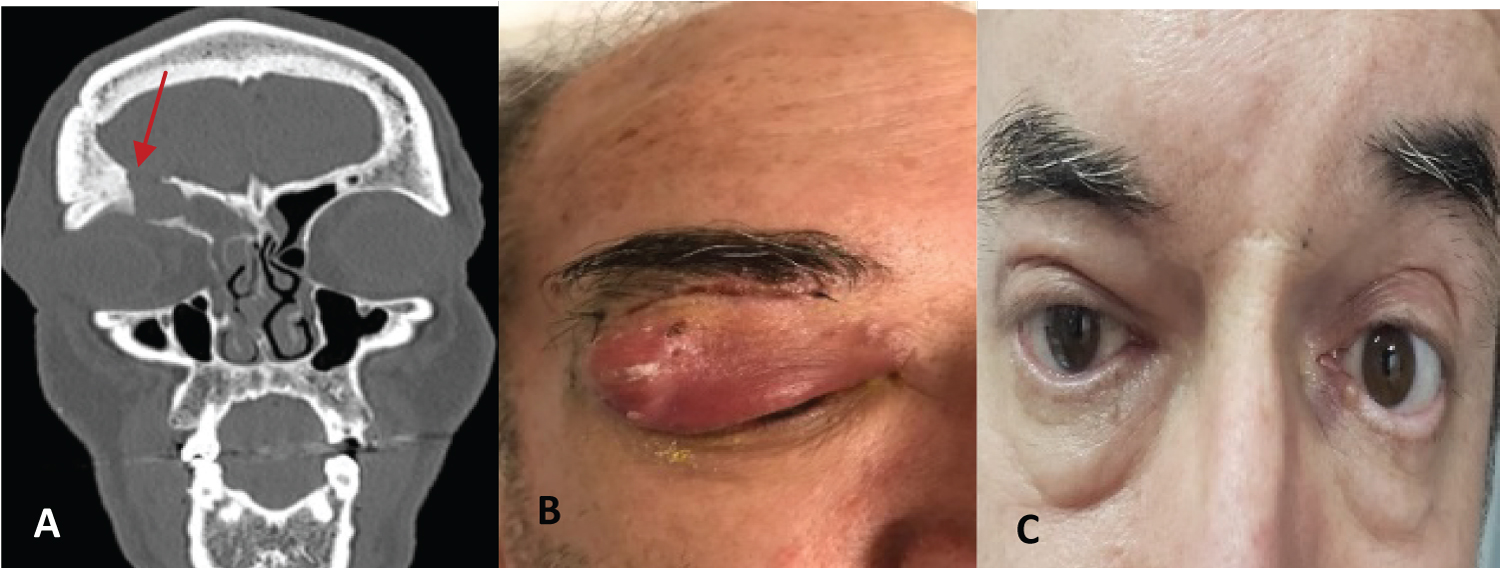 Figure 4: Revision surgery by supraorbital cell mucocelewith erosion of the inferior and posterior wall of the frontal sinus: Endonasal endoscopic and transpalpebral approach with fat obliteration of supraorbital cell cavity. A) Preoperative CT, Patient; B) Preoperative eyelid abscess and C) Postoperative.
View Figure 4
Figure 4: Revision surgery by supraorbital cell mucocelewith erosion of the inferior and posterior wall of the frontal sinus: Endonasal endoscopic and transpalpebral approach with fat obliteration of supraorbital cell cavity. A) Preoperative CT, Patient; B) Preoperative eyelid abscess and C) Postoperative.
View Figure 4
Controls were done with computed tomography and nasal endoscopy (Table 1).
Table 1: Supraorbital cell mucoceles: Surgical approaches. View Table 1
Four patients were treated with surgery by mucoceles located in supraorbital cells. Three were men and one woman, the average age was 51 years.
Two patients consulted for proptosis, and two others for proptosis and preseptal cellulitis with suppuration. In three the right orbit was affected and in one left.
All had a history of previous surgeries involving the paranasal sinuses, approximately 10 years before the consultation (chronic sinusitis 2/4, facial trauma 1/4 and craniotomy for an aneurysm of the anterior communicating artery with obliteration of the frontal sinus 1/4). One of the patients had no papyracea lamina on the same side of the mucocele.
By computed tomography, an erosion of the anterior and inferior wall of the supraorbital cell with penetration of the mucocele into the orbit was diagnosed in all patients, and in one, an erosion of the posterior wall was also observed, where the mucocele capsule had contact with the meninge.
In two patients who were treated by combined approaches (endonasal and transpalpebral) to marsupialize the mucoceles to the ethmoid cavity, recurrences occurred in a short time due to drainage stenosis of the supraorbital cells.
Revision surgery was indicated in both, again using a combined approach: Endonasal with endoscopes and transpalpebral.
The supraorbital cell cavity was again communicated to the ethmoid, but the entire mucosa was removed, the bone was drilled and only the supraorbital cell cavity was obliterated with fat.
There were no complications and the patients were discharged from hospital 24 hours after surgery.
Washes with physiological solution and corticosteroids were indicated and periodic cures were performed by sucking secretions and crusts.
In one patient, the cultures isolated staphylococcus aureus, enterococcus faecalis and cloacae. He was treated according to the indication of infectology with 1 gram of ertapenem and limezolad for 30 days.
All of them had good evolution during an average follow-up time of 2.75 year.
Supraorbital ethmoid cells are pneumatizations of the orbital plate of the frontal bone. They are located lateral and posterior to the frontal sinus, anterior to the anterior ethmoidal artery and drain laterally or posteriorly to the frontal ostium in the frontal recess.
They originate from the anterior ethmoid cells, although they may also develop from the posterior ethmoid. The size may vary and there may be more than one supraorbital cell.
In one study Van Alyea described supraorbital cells in 15 of 100 adult anatomical preparations and in another he found 14 among 242 specimens from different series [3]. Dixon in another study found 5% of supraorbital cells among 200 anatomical pieces [4].
By computed tomography of the paranasal sinuses, the supraorbital cells may have the appearance of a multiple frontal sinus, or that there are several septa within the sinus. In fact, the cell occupies a lateral and posterior position in relation to the frontal sinus.
In the axial sections it is observed posterior to the crista galli process, or more posterior to the more medial frontal cell.
Choby and collaborators analyzed 100 tomography scans of the paranasal sinuses (200 sides), and diagnosed 28.5% of supraorbital ethmoid cells [5].
By nasal endoscopy, the supraorbital cell drainage can be identified as an opening in the anterior and lateral sector of the ethmoid, in front of the ethmoid artery and behind the frontal ostium.
Some use the drainage opening of the supraorbital ethmoid cell to identify the anterior ethmoid artery, which would be at the posterior edge of the drainage hole [6].
The preoperative diagnosis of a supraorbital ethmoid cell with pathology is very important because it facilitates the choice of the best surgical approach to access it.
An undrained supraorbital cell was found in 10% of endoscopic revision surgeries of the frontal sinus [2]. In two patients in our series, despite having identified the involvement of the supraorbital cell in the production of the disease in the preoperative period, the initial surgery failed and we had to perform a more aggressive revision surgery.
In addition, diagnosing the presence of a supraorbital cell with pathology in the preoperative period can facilitate the choice of the best surgical approach to solve the existing pathology.
One of the most common inflammatory pathologies of supraorbital cells are the mucoceles. They can compromise the supraorbital cell alone or more frequently coexist with frontal sinusitis.
All the patients described in this study had mucoceles that destroyed the bone walls of the supraorbital cell and penetrated in to the orbit and in one the mucocele displaces the dura.
There are two challenges that the surgeon must consider to treat this pathology: The adequate vision of the cell located laterally to the frontal sinus and the maintenance of the drainage permeability of the mucocele located in the supraorbital cell.
Lateral vision can be obtained after performing an anterior ethmoidectomy and a Draf II or modified Lothrop frontal drainage when there is infection in both frontal sinuses.
Subsequently, with a 30° angled endoscope, the medial bone wall of the supraorbital cell can be resected with angled instruments marsupializing the mucocele in the frontal sinus.
A Draf III or modified Lothrop frontal drainage can also be performed to have better access, or to treat the infection of both frontal sinuses.
Some studies describe a surgical technique called modified hemi-Lothrop, which consists of performing an anterior ethmoidectomy, a Draf II-B on the involved side, and then an anterosuperior septectomy in order to introduce the endoscope from the contralateral nasal cavity and obtain a better angle and vision of the lateral mucocele [7,8].
Another possibility to treat a lateral mucocele in a supraorbital cell is to perform a combined, endonasal and transpalpebral approach with endoscopes to access the lateral supraorbital cell and marsupialize it to the nasal cavity [9-11].
In the two patients that we treated with combined approaches, the transpalpebral approach gave us a very good vision perpendicular to the supraorbital cell and the endonasal approach allowed us to control the amplitude of the drainage to the nasal cavity.
The other challenge is to prevent the drainage from the supraorbital cell closes due to scarring. For this, postoperative care is essential performing corticosteroid washes and debridements.
Some propose using a stent made with a pediatric biliary T-tube, placed by frontal trephination and by an endonasal approach with endoscopes so that the drainage persists open [12].
In two of the patients described after marsupializing the mucocele to the ethmoidal cavity using a combined approach (endonasal and transpalpebral), there was an obstruction of the drainage and the recurrence of the mucocele and its symptoms.
In one of them, possibly the presence of a titanium microplate used in facial reconstruction performed several years earlier and the significant distortion of the frontal and ethmoidal drainage region could explain the drainage stenosis and the recurrence of the mucocele.
In the revision surgery performed on the other patient, by making a more extensive drilled, we resected a bone-like material that was used to obliterate the frontal sinus in a craniotomy performed 15 years earlier. This material could have been a focus of recurrent infection that caused the drainage stenosis.
We reoperated them using a combined approach, but we resected all the hyperplastic mucosa, and drilled the supraorbital cell bone, obliterating only the cell cavity with fat. We call this technique mini-obliteration and we did not find it described in the literature.
The success rate with primary and revision surgery in patients treated by mucoceles located in supraorbital cells was 100%.
Endonasal approaches extended to the frontal sinus alone or combined with external approaches by transpalpebral incision allow adequate vision and drainage of the supraorbital cell and control of the extent of marsupialization towards the frontal sinus or ethmoidal cavity.
Mucosal resection, bone drilled, and supraorbital cell obliteration are part of a treatment algorithm, representing the point of greatest surgical aggressiveness.
We have no conflicts of interest.