Objective: To evaluate the success rate of revision myringoplasty using temporalis fascia graft myringoplasty and to analyse the effect of potential influencing factors on closure of tympanic membrane (TM) and hearing outcome such as size of perforation (less or greater than 50% of tympanic membrane), site (anteriorly or posteriorly located) of perforation, whether the patient smokes or not, and condition of contralateral ear.
Materials and methods: Thirty patients were included in this prospective study, who underwent revision myringoplasty for chronic otitis media without cholesteatoma in the period between 1-1-2017/1-6-2019 in ENT H&N surgery department in Almowasat University Hospital. Data of all patients: Perforation size and localization, middle ear status, surgical approach, graft material, pre- and postoperative morphological (otomicroscopy) and functional (hearing examination evaluating pure-tone audiogram) results were analysed. All operations were performed using an underlay technique and the retroauricular approach. The temporal fascia, were used for the reconstruction of TM. The interrelation between multiple preoperative parameters and post-operative morphological (closure of the perforation) and functional (hearing level) outcomes was analysed.
Results: Successful closure rate of the TM perforation was 86.66% (in 26 out of 30 patients) and failure rate was 13.33% (in 4 out of 30 patients) in revision myringoplasty. Graft uptake was higher in cases with small perforation (< 50% of TM) 91.30% than in cases with large perforation (> 50% of TM) 71.42%, (P 0.002- statistically significant). Graft uptake with normal opposite ear was 90.90%, and with abnormal opposite ear (retraction tympanic membrane without cholesteatoma) was 75% (P 0.001- statistically significant). We found no statistically significant difference in graft uptake results with other factors. The improvement of the air bone gap between 10-20 was 76.66% decibels (23 out of 30 patients) while the air bone gap (between 20-30 decibels) remained unchanged 23.33% (7 out of 30 patients).
Conclusion: Revision myringoplasty can offer reasonably good chances for postoperative graft healing and hearing improvement with a high success rate. This gives the patient a good benefit in protecting the ear from developing complications that may have poor structural changes in the middle ear (ossicular necrosis and tympanoscerosis) which in turn leads to hearing loss.
Revision myringoplasty, Temporalis fascia, Tympanic membrane perforation, Revision surgery
Myringoplasty is performed as a single procedure, or as a part of another ear operation such as a tympanoplasty or tympanomastoid surgery, is not always successful, many studies are cited to be from 75-100% [1,2]. The primary outcome measure for success is the perforation closure. The secondary outcomes are hearing change and reduction in frequency of ear infections. Successful results of tympanoplasty are consistent today, however, failures happen. The success rate of revision tympanoplasty for chronic otitis without cholesteatoma is not uniformly evaluated in literature. Although morphological results for primary and revision myringoplasty are similar [3,4]. Revision myringoplasty has been shown by numerous authors to be a risk factor for a subsequent failure in graft acceptance and hearing results [1,5], consequently it has led to the need for a particular graft.
Temporalis fascia is still considered the best choice as a graft material for TM closure and it remains the most commonly used graft in primary tympanoplasties [6-8]. However, a sceptical view exists regarding the use of fascia for residual defects after primary surgery, although the number of studies comparing the success rates of fascia and other grafts for revision tympanoplasty is few [9,10]. Due to its excellent healing potential and satisfactory hearing outcomes, the cartilage has been advocated as a first choice substrate for tympanic membrane repair in revision tympanoplasty [11,12]. In fact, there are no studies available in which the same author reports the results of primary and revision tympanoplasty in one study using the same technique.
The limited available literature that reports the results of revision myringoplasty is sometimes used to support the contention that revision myringoplasty is less successful than primary surgery [13,14]. However, there are certain situations such as atelectatic ear, eustachian tube dysfunction, active suppuration, tympanosclerosis and revision myringoplasty among others, where these results have not been as gratifying. These cases are defined as high-risk perforations [15,16]. Candidates for revision tympanoplasty have experienced at least one failed attempt at repair of the tympanic membrane and are, therefore, at higher risk for subsequent repair failure [12,17-19]. Revision tympanoplasty cases are a delicate situation for otologists and the success rate decreases in such operations [6,9].
The aim of the present study is to evaluate the success rate for revision myringoplasty after a previously unsuccessful reconstruction of TM to find the results of re-tympanoplasty using the same technique, and to analyse the effect of the factors such as size of perforation (less or greater than 50% of tympanic membrane), site (anteriorly or posteriorly located) of perforation, side of perforation, whether the patient smokes or not, and condition of contralateral ear that potentially influence the closure of TM and hearing outcome.
This prospective study was conducted in Almouwasat University Hospital during the period between 1-1-2017/1-6-2019. This study included all patients, who underwent re-myringoplasty for chronic otitis media without cholesteatoma. All patients were followed up clinically at 1 and 3 weeks postoperatively, and clinically and audiologically at 6-9 months postoperatively.
Patients who fulfilled the following criteria were included in the study: Patients between 18 and 65 years of age with residual or recurrent central tympanic perforation after previously unsuccessful reconstruction of TM and no active infection for at least 3 months before the revision procedure and those with mild (25-40 dB) conductive hearing loss. Patients below 18 years and above 65 years of age, those with active ear infection, those with attic perforation and/or retraction, those with audiometric loss not consistent with sole involvement of tympanic membrane were excluded from our study. Sex of the patient, size of perforation (less or greater than 50% of tympanic membrane), site (anteriorly or posteriorly located) of perforation, and the side of perforation, whether the patient smokes or not, condition of contralateral ear were collected to see its effect on the success rate of the surgery. Audiometric values were taken at frequencies 500, 1000, 2000, and 4000 Hz preoperatively and at 6-9 months postoperatively.
The researchers candidated under the criteria of ethics of Damascus University which is compatible with Helsinky standards. All patients agreed to participate in the study and were well informed about the study, stages and the operation risks.
The surgery was performed under general anesthesia. The incision area behind the pinna and the auditory canal was injected by a solution of lidocaine/adrenaline 1.100.000. An incision was made 0.5-1 cm behind the postauricular crease with harvesting of the deep temporalis fascia graft. Thereafter, the external auditory meatus was entered, trimming the edges of tympanic membrane remnants, raising the tympanomeatal flap and annulus to reach the middle ear cavity (ossicular chain was normal in all patients) and the graft was fixed using the underlay technique, a gel foam was used to cover the graft. Repositioning of the flap was performed, followed by closure of the wound.
All of the data was collected and arranged on Excel 2016 to draw tables and illustrations, and SPSS Ver 16 was used to perform the necessary statistical tests for this work, as a t test and Chi-Square test were used, the P value.
The closing of the perforation of the tympanic membrane and improvement of the air-bone gap to between 10-20 dB after 6-9 months was considered the success of this surgery.
A total of 30 patients were included in the study and underwent the surgery, and completed the follow-up program. The time period from the primary operation to revision ranged from 18 months to 24 months. The patients were carried out during the preparation of the surgery, by examining the affected ear (dry central TM perforation) and the contralateral ear. We found by examining the contralateral ear preoperatively a varying degrees of retraction tympanic membrane without cholesteatoma that was evaluated by tympanometry test (type C) in 8 patients. Graft uptake was observed in 26 out of 30 (86.66%). Patient's ages ranged from 18 to 65 years. There were total 12 (40%) males and 18 (60%) females. Fourteenth (46.66%) underwent right myringoplasty and sixteenth (53.33%) underwent left myringoplasty. The graft uptake results in relation to various factors are shown in tables below. Site of perforation and smoking status were not found to be significant determining factor for successful revision myringoplasty. Graft uptake was higher in cases with small perforation (< 50% of TM) 91.30% than in cases with large perforation (> 50% of TM) 71.42%, this result was statistically significant (p = 0.002). We found that 22 patients, who underwent myringoplasty, had normal contralateral ear. Graft was taken up in 20 (90.90%). 8 patients had a varying degrees of retraction of TM in the contralateral ear and graft was taken up in 6 patients (75%). Graft uptake was significantly poor when the contralateral ear had retraction of TM (p = 0.001). All 30 patients had normal ossicular chain. The average pre-operative bone conduction threshold was 16.75 dB and the average post-operative bone conduction threshold improved to 13.50 dB, which was not statistically significant (P = 0.332). The average pre-operative air conduction threshold was 38.5 dB and the average post-operative air conduction threshold improved to 27.25 dB, which was statistically significant (p = 0.001). The average pre-operative air bone gap was 21.5 dB and the post-operative air bone gap was 13.25 dB, which was statistically significant (p = 0.004) Table 1 and Table 2.
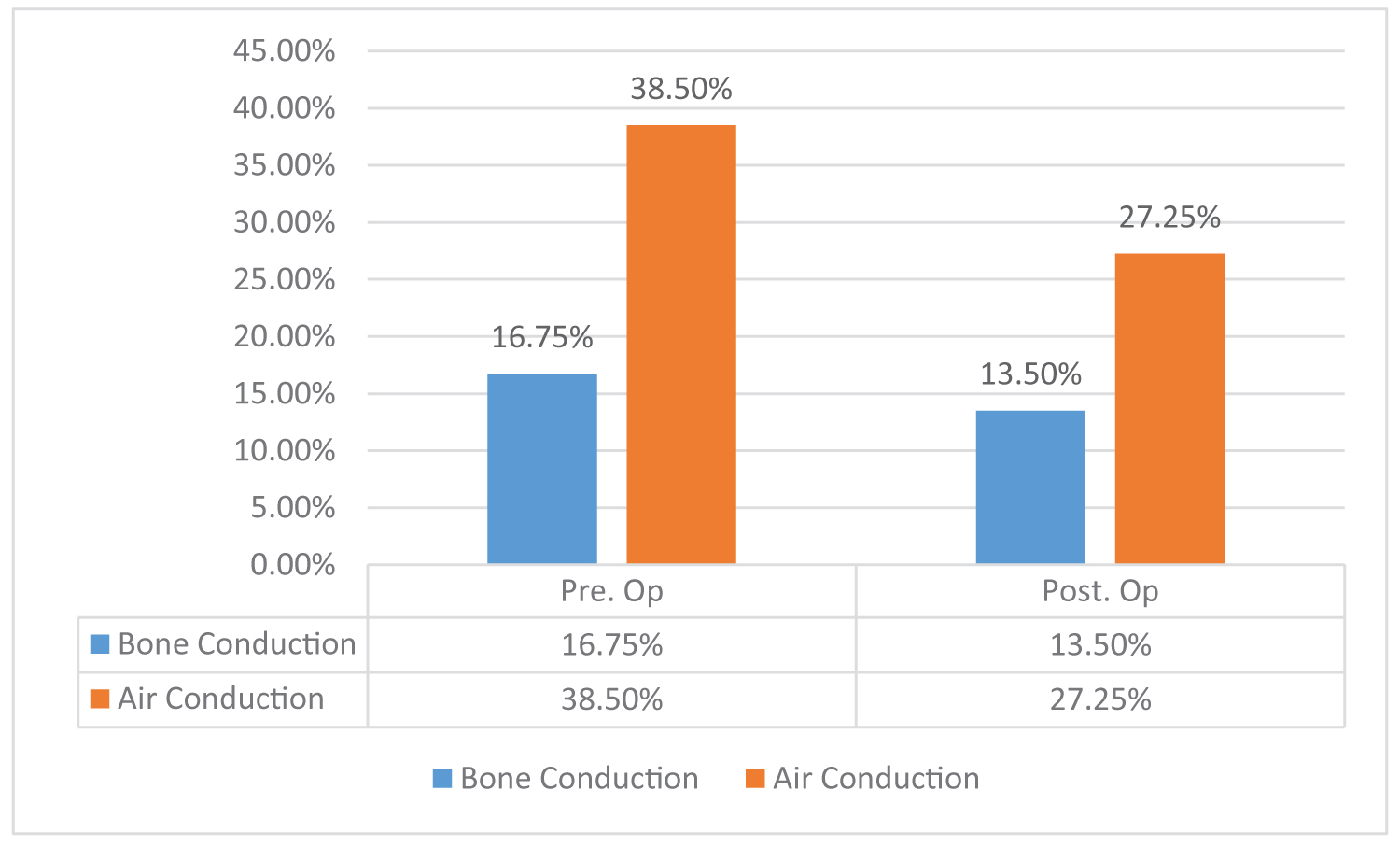 Figure 1: Shows change in air-bone thresholds before and after surgery.
View Figure 1
Figure 1: Shows change in air-bone thresholds before and after surgery.
View Figure 1
Table 1: Factors affecting success rate of revision myringoplasty. View Table 1
Table 2: Hearing results after revision myringoplasty. View Table 2
Myringoplasty is the most common middle ear surgery performed in our center, with cases referred from all regions of the country. Repair of a recurrent tympanic membrane perforation is a challenge for the ear surgeon. Although primary tympanoplasty has high successful rates, around 90% or higher [6,7,20], successful outcome in revision cases can be more difficult to achieve [21,22].
There was a significant difference in graft uptake with the size of perforation in this study, similar results have been shown in some international studies. In this study the researcher achieved a success rate of 91.30% for small perforations (size less than 50%) and 71.42% for large perforations (size greater than 50%). However, in the case of larger TM defects, healing has a much poorer prognosis and because of the increased technical difficulty and area that must be vascularized and epithelialized with larger perforations, surgical failures are not unexpected [23,24]. The absence of an adequate residual TM in subtotal or total TM perforations remains a challenge to otolaryngologists. Study by Kotecha, et al. and Onal, et al. have shown better graft uptake in small size perforation as compared with large perforation [25].
In this study, the researcher found the status of the contralateral ear to be an important prognostic factor for graft uptake. Graft uptake was significantly poor when the contralateral ear had a retraction of TM (P = 0.001). We found similar results in some international studies. This finding might indicate an eustachian tube dysfunction and the tendency of chronic otitis media to present as a bilateral disease [25]. The status of contralateral ear is important in two aspects: First, in its contribution for understanding the pathogenesis of otitis media, and second, in its implications in treatment and counseling. The researcher found similar results in the studies by Calyan, et al. and Ophir, et al. [25,26].
There was no significant difference in graft uptake with the site of perforation in this study, although the success rate in posterior perforations was slightly higher than anterior perforations 90.90% vs. 84.21% respectively. This has been attributed to technical challenge to repair due to the poor visibility of anterior margin of perforation, more difficult access, inadequate graft support, and relatively poorer perfusion in anterior portion of tympanic membrane [25], most of the recent studies have found that the site of perforation is not a determining factor for successful myringoplasty [27,28].
In this study, 24 patients were non-smokers and 6 patients were smokers. The graft uptake in non-smoking group was 87.5% and that in the smoking group was 83.33%. This difference was not statistically significant, likely due to a disproportionate population within the subgroup.
However, we did not take into account details of amount and duration of smoking in this study. We have to know that smoking changes the amount and viscosity of mucous and destroys the ciliated epithelium of the eustachian tube and middle ear mucosa [28]. Nicotine causes cutaneous vasoconstriction, promotes thrombosis, and carbon monoxide inhaled in cigarette smoke also reduces the oxygen-carrying capacity of the blood, which in turn causes inadequate oxygenation of the graft. These factors may impair the graft vascularization. The systemic effects of smoking are the chemoallergic and immunosuppressive properties that may cause increased susceptibility to the infectious agents and thereby lead to graft failure [28]. A study by Wasson, et al. did not find smoking to be a significant factor for successful myringoplasty [29-31].
The researcher also found a statistically significant functional result when studying closure of the ABG in our study, with most being between 10-20 dB. Hearing improvement after myringoplasty is statistically significant if the ossicles are normal.
The researcher also found that the leading causes of failure (4 cases) were associated with a complete no-take of the graft (1 case), infection with graft necrosis (1 case) and poor anterior adaptation of the graft (2 cases).
Revision myringoplasty can offer reasonably good chances for postoperative graft healing and hearing improvement with a high success rate. This gives the patient a good benefit in protecting the ear from developing complications that may have poor structural changes in the middle ear (ossicular necrosis and tympanosclerosis) which in turn leads to hearing loss. Despite the recommendation of many studies that the use of a cartilage graft in the revision myringoplasty is more preferred, the researchers found that using a facial graft gives good surgical results, both in terms of graft uptake or improving hearing after surgery. In this study, we were not able to adopt a control group for comparison, and the sample was relatively small. Therefore, the researchers recommend in the future to conduct similar studies, but with the adoption of a control group to compare the results and take a larger sample in order to make the results more accurate.
Prof. M. Nabil Dandashli. MD, PhD made great contributions in editing the intellectual content and proofreading of this paper.