To present a case of sinonasal meningioma and to review the literature on its pathophysiology, clinical presentation, diagnosis, and management.
Design: Case Report; Setting: Tertiary Government Hospital; Patient: One.
A 53-year-old male presented with persistent right nasal obstruction and recurrent epistaxis. He was initially managed as a case of nasal polyposis. However, persistence of symptoms prompted consult with another ENT specialist. Further evaluation revealed meningioma in the sinonasal tract. The patient underwent bifrontal craniotomy with excision of the intracranial extension of the tumor and endoscopic excision of the intranasal meningioma. Follow-up revealed resolution of symptoms and absence of tumor recurrence.
Although rare, meningioma may originate in the sinonasal tract with non-specific manifestations. A thorough assessment and the use of appropriate diagnostics will help establish a precise diagnosis and prevent delays in providing definitive management.
Meningioma, Sinonasal meningioma, Intranasal mass
Meningioma is a slow-growing neoplasm of the central nervous system and is thought to arise from meningocyte capping of arachnoid villi [1]. It is a common intracranial tumor accounting for 15% of all intracranial tumors [2]. In rare instances (< 2%), it appear extracranially, most often in the head and neck region, and specifically in the sinonasal tract [3]. Given its rarity, extracranial meningiomas of the sinonasal tract are frequently misdiagnosed, resulting in inappropriate clinical management [4]. This paper aims to present a case of sinonasal meningioma and to discuss the clinical course and management of this disease.
A 53-year-old Filipino male presented with two-year history of right nasal obstruction with rhinorrhea and epistaxis. He was initially managed medically as a case of nasal polyposis. He denied any history of visual impairment, seizure, headache, and weakness. Despite good compliance with the medications prescribed to him, no relief of symptoms was noted. He went to another specialist for a second opinion. Paranasal sinus CT Scan (Figure 1) was done which revealed a large expansile mass in the right nasal cavity. This was followed by MRI of the paranasal sinuses (Figure 2) with gadolinium that revealed a right heterogeneously enhancing nasal mass with no intracranial extension. Punch biopsy of the mass revealed features suggestive of hemangiopericytoma, ectopic meningioma, and glomangiopericytoma. Immunohistochemical staining was suggested for a definitive diagnosis. Immunostain with Vimentin and Epithelial Membrane Antigen were strongly positive. This confirmed the diagnosis of ectopic meningioma. The patient was advised surgery, but was lost to follow up.
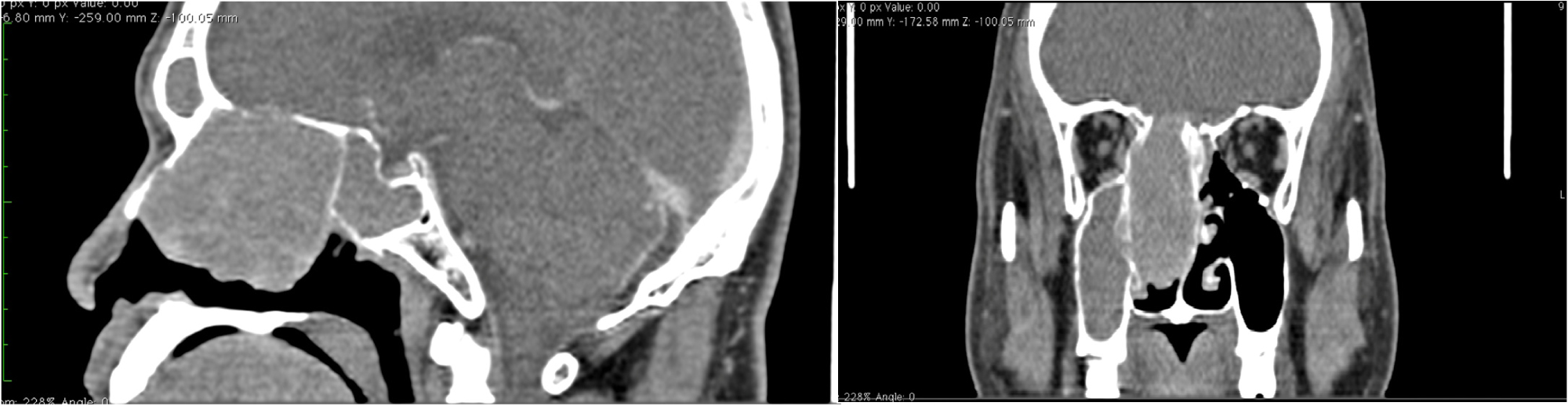 Figure 1: Sagittal and coronal CT scans with contrast showing a mass filling the right nasal cavity enhanced by the contrast associated with filling of ipsilateral maxillary sinus.
View Figure 1
Figure 1: Sagittal and coronal CT scans with contrast showing a mass filling the right nasal cavity enhanced by the contrast associated with filling of ipsilateral maxillary sinus.
View Figure 1
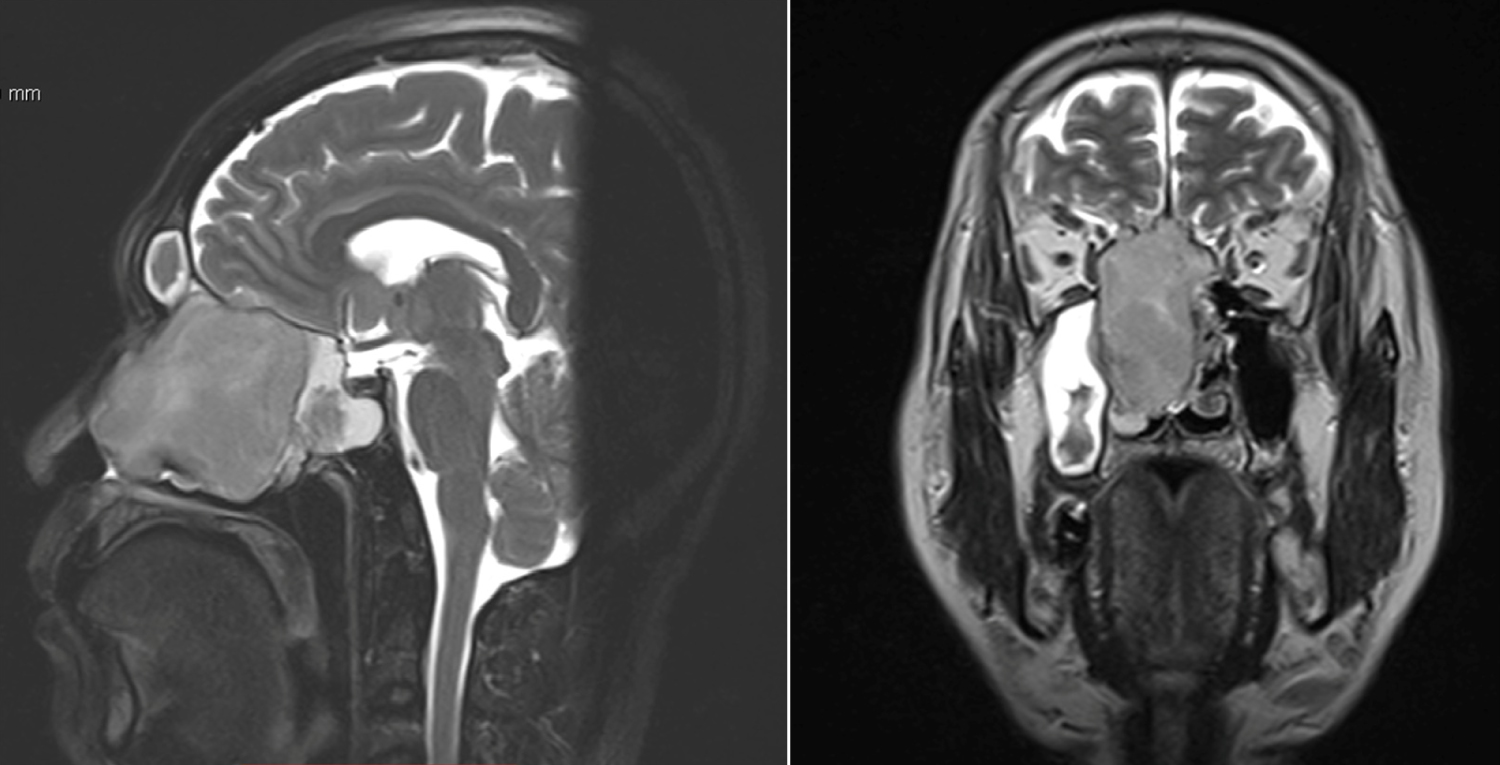 Figure 2: Sagittal and coronal MRI of the Paranasal Sinuses with Gadolinium shows a heterogeneously-enhancing mass in the right nasal antrum. The mass superiorly involves all the right ethmoid sinuses and sphenoethmoidal recess eventually indenting the floor of the anterior cranial fossa but with no intracranial extension.
View Figure 2
Figure 2: Sagittal and coronal MRI of the Paranasal Sinuses with Gadolinium shows a heterogeneously-enhancing mass in the right nasal antrum. The mass superiorly involves all the right ethmoid sinuses and sphenoethmoidal recess eventually indenting the floor of the anterior cranial fossa but with no intracranial extension.
View Figure 2
Five months later, the patient was seen at our institution. Initial symptoms were still present. Anterior rhinoscopy revealed a firm, pinkish, fleshy mass completely filling the right nasal cavity. Septal deviation to the left was noted. Neurologic examination was unremarkable. Repeat paranasal sinus CT Scan (Figure 3) showed a large expansile right intranasal mass with dehiscence of the cribriform plate of ethmoid with extradural protrusion or extension. Surgical management was planned and Neurosurgery referral was made for co-management.
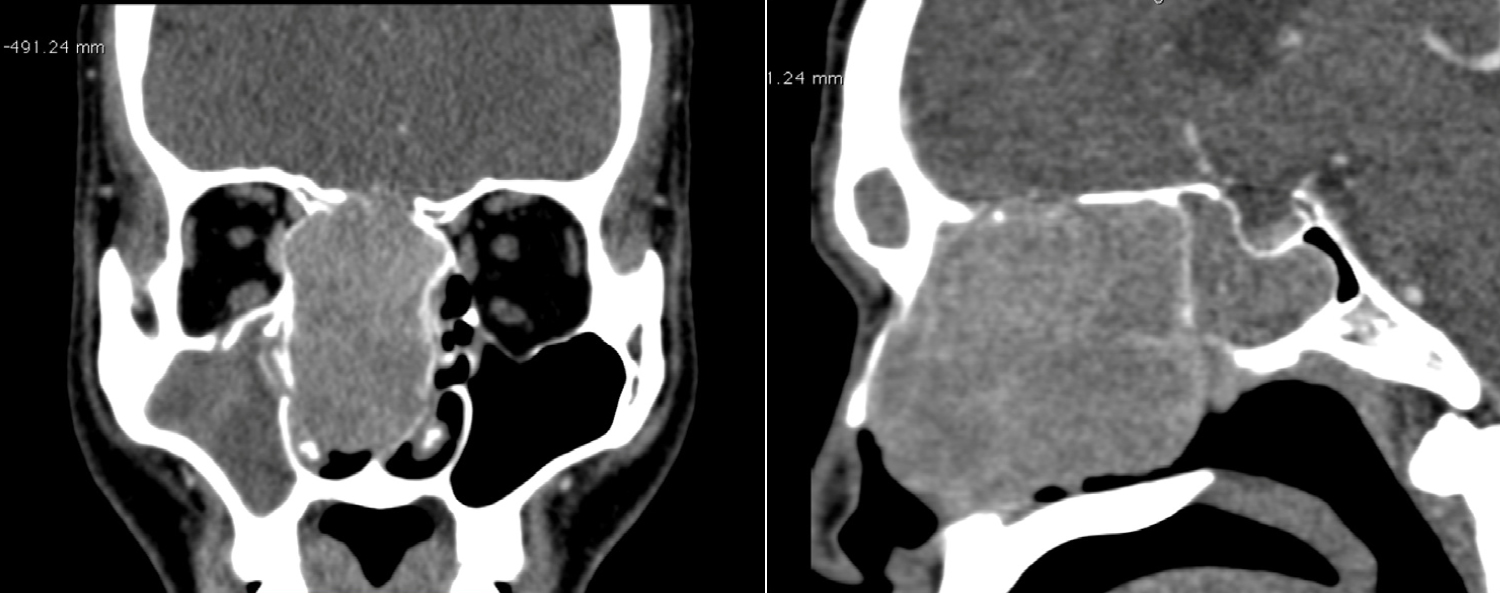 Figure 3: Coronal and sagittal CT scans with contrast showing a large expansile mass in the right nasal cavity. The cribriform plate of ethmoid, basal lamellae, and inferior half of crista galli are absent representing resorption with soft tissue extension into the olfactory grooves.
View Figure 3
Figure 3: Coronal and sagittal CT scans with contrast showing a large expansile mass in the right nasal cavity. The cribriform plate of ethmoid, basal lamellae, and inferior half of crista galli are absent representing resorption with soft tissue extension into the olfactory grooves.
View Figure 3
The patient underwent bifrontal craniotomy. Subfrontal excision of meningioma was performed. Intra-operatively, the tumor was seen invading the cribriform plate and dura. Following the excision of the intracranial extension of the tumor and repair of the dura, endoscopic excision of the intranasal meningioma was done. The mass was attached to the nasal septum anterior to posterior and middle turbinate (Figure 4). Tumor debulking was done using a micro-debrider. Histological examination later showed transitional meningioma. Microscopic sections show tissues composed of lobulated, nested, or whorled aggregates of polygonal to epithelioid cells with inconspicuous nucleoli, lightly eosinophilic cytoplasm, and indistinct cytoplasmic borders, with areas having psamomma bodies (Figure 5). Postoperative recovery was uneventful and there was no recurrence after a 4-month follow up.
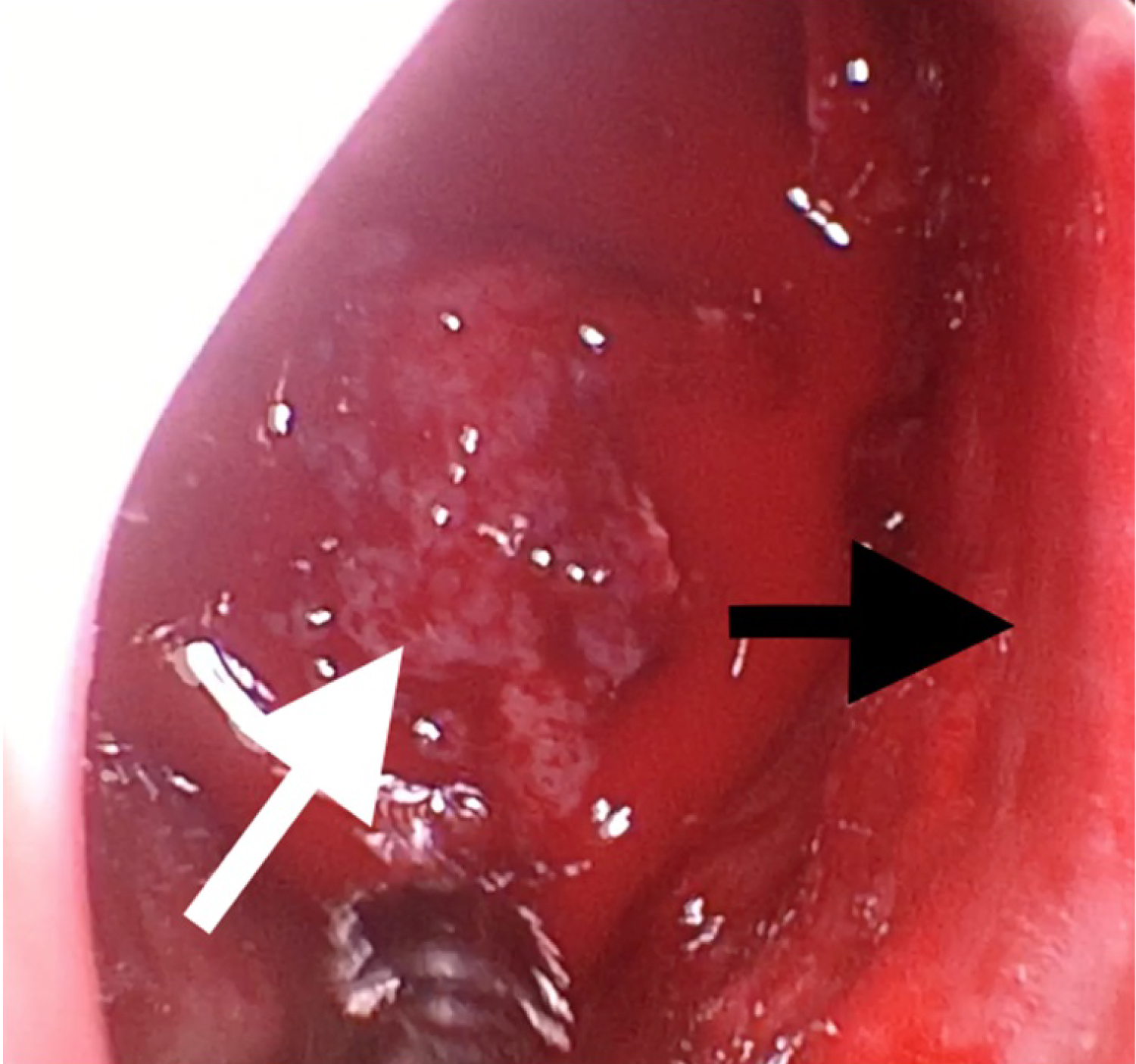 Figure 4: Pinkish polypoid mass in the right nasal fossa seen intraoperatively (white arrow). Nasal septum deviated to the right (black arrow).
View Figure 4
Figure 4: Pinkish polypoid mass in the right nasal fossa seen intraoperatively (white arrow). Nasal septum deviated to the right (black arrow).
View Figure 4
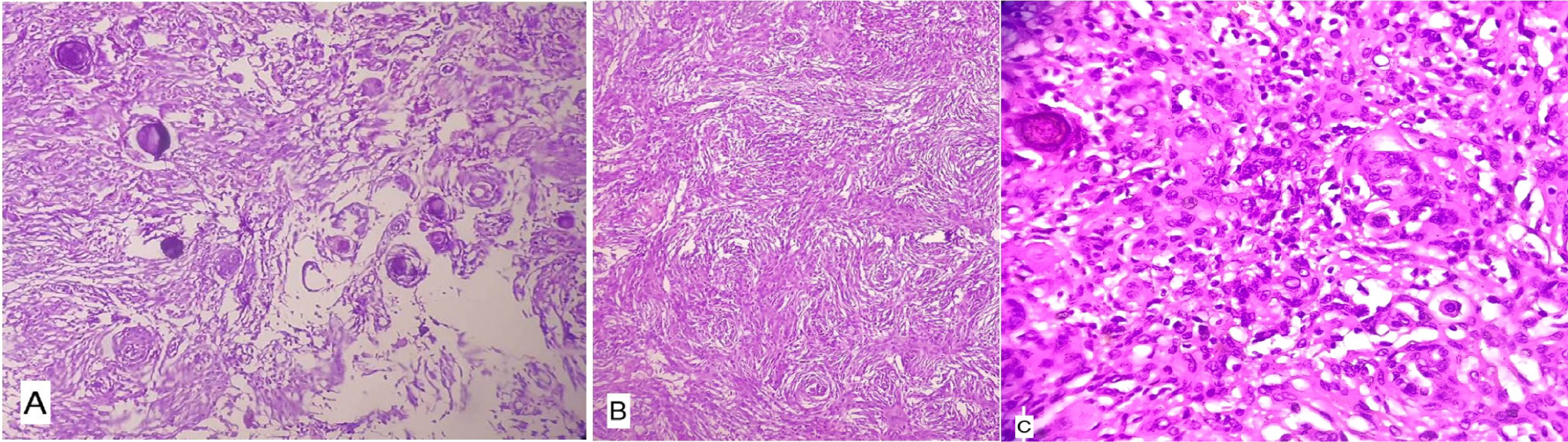 Figure 5: A) Scanner view (4X); B) Low power view (10X); C) High power view (40X). H&E stain: Lobulated, nested, or whorled aggregates of polygonal to epithelioid cells with inconspicuous nucleoli, lightly eosinophilic, and indistinct cytoplasmic borders, with areas having psamomma bodies.
View Figure 5
Figure 5: A) Scanner view (4X); B) Low power view (10X); C) High power view (40X). H&E stain: Lobulated, nested, or whorled aggregates of polygonal to epithelioid cells with inconspicuous nucleoli, lightly eosinophilic, and indistinct cytoplasmic borders, with areas having psamomma bodies.
View Figure 5
Extracranial primary meningioma is notably a tumor of rare occurrence with an incidence of 0.9% [5]. They are most commonly found in the cervicofacial region particularly the orbit, the scalp, the petrous pyramid and the paranasal sinuses [2].
Meningiomas arise from arachnoid cap cells, with different mechanisms to suggest how extracranial meningiomas arise:
• Arachnoidal cells are present in the sheaths of nerves or vessels where they emerge through the skull foramina.
• Displaced pacchionian bodies become detached, pinched off, or entrapped during embryologic development in an extracranial location.
• A traumatic event or cerebral hypertension that displaces arachnoid islets [6].
• The classification system of Hoye encompasses the major etiologies proposed in the development of extracranial meningiomas [3].
• Extracranial extensions of a meningioma with an intracranial origin (Secondary).
• Extracranial extensions of a meningioma arising in a neural foramina (Primary).
• Ectopic, without any connection either to foramen of a cranial nerve or to intracranial structures (Primary).
• Extracranial metastasis from an intracranial meningioma (Secondary).
Clinical features are nonspecific [2]. Patients usually presents with nasal obstruction, nasal mass, proptosis, epiphora, pain and occasionally epistaxis [6].
CT Scan or MRI precisely gives information of the extent and invasion of the tumor and is imperative in the diagnosis. However, the final diagnosis depends on the histological examination [5]. The current World Health Organization classification distinguishes between three grades of meningioma: Typical or benign (Grade I); atypical with frequent mitosis (Grade II); and anaplastic with invasion (Grade III) [4]. The most common histopathological subtype of Primary Extracranial Meningiomas (PEMs) in the head is meningothelial meningioma. Other common subtypes include transitional, psammomatous and fibrous [7]. The histological features are characteristic in the meningothelial form but can be less typical in the other forms hence the importance of immunohistochemical studies. Meningiomas express a strongly positive reactivity for vimentin and epithelial membrane antigen (EMA) and exhibit focal immunoreactivity with S-100 protein, keratin and CEA [2]. In the present study, the tumor was classified as Grade 1 and histopathologic subtype was transitional meningioma. Immunohistochemical studies revealed a strongly positive reaction for both vimentin and EMA.
Treatment of primary extracranial meningioma is surgical excision because meningiomas are known to be radio resistant and recurrence is very rare following adequate surgical resection [7].
Primary sinonasal meningiomas are infrequently occurring tumors. Although the etiology remains unknown and the symptomatology is non-specific, treatment of sinonasal meningioma is less difficult if guided by a thorough understanding of the appropriate diagnostic and management principles. CT and MRI show the extent and invasion of the tumor while histologic and immunohistochemical studies confirms the diagnosis. Complete surgical excision is the definitive treatment. Prognosis is excellent because recurrence is very rare following adequate surgical resection of the tumor. The authors declare that this represents original material, that the manuscript has been read and approved by all the authors, that the requirements for authorship have been met by each author, and that each author believes that the manuscript represents honest work.
The authors signed disclosures that there are no financial or other (including personal) relationships, intellectual passion, political or religious beliefs, and institutional affiliations that might lead to a conflict of interest.