Frozen shoulder is a condition of uncertain etiology characterized by limitation of both active and passive shoulder movements in the absence of intrinsic shoulder pathology. In our study, we are comparing the efficacy of two modes of treatment for frozen shoulder i.e. suprascapular nerve block vs. intraarticular steroid in relieving pain and disability.
Patients who are diagnosed to have frozen shoulder on an OPD basis are included in the study. 50 patients were randomly divided into 2 groups. One group received suprascapular nerve block using nerve stimulation guided technique and the other group received intraarticular steroid. Home physiotherapy was advised following the procedure. Pain and disability were assessed at 2 wks, 4 wks, 8 wks, and 12 wks post-injection by SPADI scores.
The baseline SPADI score in the IAS group was 55.56 (13.169) which at 12 weeks improved to 27.80 (10.778) which was significant (p = 0.001). The baseline SPADI score in the SSNB group was 57.28 (17.353) and at 12 weeks improved to 11.48 (4.885) which was significant (p = 0.001). Between group comparison showed better improvement of SPADI score with SSNB (p value 0.001). SPADI score improved at a rate of 3.81 per week in SSNB group as compared to 2.31 per week in the IAS group. Both the groups showed significant improvement in SPADI scores however the SSNB group had a more efficient and faster relief of symptoms compared to the IAS group.
Suprascapular nerve block using nerve stimulator and intraarticular steroid injection are effective and reliable method in reducing shoulder pain and disability in frozen shoulder. Compared to intraarticular steroid injection, suprascapular nerve block attains a faster and better reduction in SPADI scores.
Frozen shoulder, Suprascapular nerve block, Nerve stimulation, Intraarticular steroid, SPADI score
Chronic shoulder pain, Frozen shoulder, Suprascapular nerve block
SPADI: Shoulder Pain and Disability Index; IAS: Intraarticular Steroid; SSNB: Suprascapular Nerve Block
Frozen shoulder is a condition that is associated with pain and progressive stiffness of the shoulder joint [1]. It is more frequently seen in middle-aged and elderly and in diabetics. Codman [2] in 1934 described this disease as one with slow onset pain in the shoulder with restricted active and passive range of movements of shoulder.
Pathogenesis of frozen shoulder is not fully understood, but evidence shows capsular contracture and proliferative synovitis as integral to the pathology [3]. This condition is characterized by a painful inflammatory phase (Phase 1), a stiffening phase (Phase 2), and a thawing phase (Phase 3). Patients with frozen shoulder generally improve for pain but some have a functional limitation due to ensuing stiffness. This course of clinical improvement can be rather protracted resulting in months of protracted night pain and loss of function.
The mainstay of treatment is to control the inflammation with NSAIDs. Exercises to improve the range of movement of the shoulder are also started during the treatment. However, some patients are refractory to the above line of management and are intolerant to the use of NSAIDs. Refractory cases are managed by various options like intraarticular steroid injection, suprascapular nerve block, manipulation under anesthesia, arthroscopic adhesiolysis, etc. Manipulation under anesthesia has some disadvantages like an increase in soft-tissue trauma thereby causing an inflammatory response. This can increase the pain of the patient and can also cause an inadvertent fracture. Once the disease has progressed to Phase 3, most cases will require arthroscopic capsulotomy. The addition of intraarticular steroid injection or a suprascapular nerve block before physical therapy has been shown to accelerate functional recovery in metanalysis [4,5]. These treatments are likely to be more effective in Phase 1 (painful phase) of the disease. But whether one intervention is superior to the other, remains to be seen.
The study aims to compare the effectiveness of suprascapular nerve block to intraarticular steroids as a prior adjuvant to physical therapy in relieving pain and improving shoulder disability in patients with frozen shoulder.
Clearance of the Institutional Ethics Committee (HEC12/10/2019/MCT) was obtained and the trial is registered in CTRI-REF/219/025684.
Design: Double-blinded randomized controlled study.
Setting: Orthopedic outpatient clinic at Government Medical College, Trivandrum.
Inclusion criteria: Consecutive patients with a clinical diagnosis of the frozen shoulder between the age group 40 to 60 years were included. The duration of onset of symptoms should be more than 4 weeks and less than 6 months.
Exclusion criteria: Patients whose symptoms were less than 4-weeks-old were excluded as they have a chance for spontaneous improvement.
Similarly, patients whose symptoms were more than 6 months were also excluded as these patients might require a different therapeutic approach.
Patients who showed glenohumeral arthritis or extensive cervical degenerative changes in X-rays.
Secondary frozen shoulder due to rotator cuff tears as they were managed differently by arthroscopic interventions.
Patients with upper limb monoplegia following cerebrovascular accident.
History of prior physiotherapy to shoulder or history of prior intraarticular injections within the last 6 months.
History of allergy to any of the injectables used.
Patients with bilateral frozen shoulder.
The outcome assessed was the change in shoulder pain and disability index (SPADI) scores in the two group's pre- and post-intervention.
The study design was that of a double-blinded randomized controlled trial. The randomization sequence was generated using block randomization with a block size of four. The intervention was masked for the patients as well as for the evaluator. Patients assigned to the two treatment groups. Consecutive 50 patients who met the inclusion criteria were randomized into two groups --Group A: Intraarticular steroid group (IAS group): Received intraarticular triamcinolone mixed with 0.5% ropivacaine and Group B: Received suprascapular nerve block (SSNB group) with 0.5% ropivacaine and 40 mg triamcinolone. Group A patients were also given a sham suprascapular nerve block where only the nerve was stimulated via nerve stimulator but no drug was given. Group B patients were also given a needle prick at the posterior joint line of the shoulder but no drug was injected. This was done to blind the patients on the treatment they received. Both the groups were started on home physical therapy. A chart containing figures of exercises to be performed was given and a video demonstration of the home exercises. Patients were reassessed at 2 weeks, 4 weeks 8 weeks, and 12 weeks.
Patients were asked to fill the self-administered SPADI questionnaire (Shoulder Pain and Disability Index (SPADI) score at Week 0 (before injection) and at the stipulated intervals of 2 weeks, 4 weeks, 8 weeks and 12 weeks. SPADI score consists of 5 questions for pain domain and 8 questions for Disability domain [6].
Technique: Intraarticular steroid injection 4 was done through the posterior approach. The needle is inserted 2-3 cm inferior and medial to the posterolateral corner of the acromion and directed anteriorly towards the coracoid process. The needle is advanced in this direction and a loss of resistance indicates the needle is in the glenohumeral joint. 5 cc of ropivacaine mixed with 40 mg triamcinolone was injected.
Suprascapular nerve block: We followed the Meier technique [7] (Figure 1). With the patient sitting, the midpoint of the spine of the scapula is marked. A point 2 cm above and 2 cm medial to the midpoint of this line is chosen and nerve stimulator needle (Stimuplex, Braun) is inserted at an angle of 45 degrees coronal and 30 degree caudal inclination to hit the suprascapular nerve. Elicitation of external rotation movement at 0.5 mA is considered as an ideal block. 10 ml of 0.5% ropivacaine and 40 mg of triamcinolone is injected.
Post-injection protocol: Patients were advised to use analgesics for 2 days after the injection. Ice pack application for shoulder was advised at night time. They were instructed to start with a home program of Codman pendulum exercises and capsular stretching as per the home therapy booklet given to them (Appendix).
The trends in the reduction of outcome scores (pain, disability, and SPADI) were measured in changes in median (IQR). The positional measures central tendency and dispersion were used because these variables were skewed as per normality tests. Friedman test was used to test the significance of a change in outcome scores over time. General linear models for repeated measures were used to test between-group variations.
Mean (SD, range) of the age of IAS group was 58.96 (8.15, 44-70) years and that of SSNB group was 55.64 (10.84, 34-77) years. Fifteen (60%) of the former and 11 (44%) of the latter were belonging to the above 60 age category. Number (%) of men in IAS and SSNB categories were 12 (48) and 8 (32) respectively.
The mean pain score in SPADI in the IAS group was 27.84 (SD 8.523) in the pretreatment phase. This improved to 23.84, 13.24, 11.24, and 8.92 at 2 weeks, 4 weeks, 8 weeks, and 12 weeks respectively.
The mean pain score in SPADI in the SSNB group was 30.64 (SD 9.318) in the pretreatment phase. This improved to 14.52, 11.92, 9.92, and 7.4 at 2 weeks, 4 weeks, 8 weeks, and 12 weeks respectively.
The mean disability score in SPADI in the IAS group was 72.96 (SD 21.011) in the pretreatment phase. This improved to 63.16, 53.16, 43.00, and 36.16 at 2 weeks, 4 weeks, 8 weeks, and 12 weeks respectively.
The mean disability score in SPADI in the SSNB group was 73.88 (SD 24.492) in the pretreatment phase. This improved to 36.36, 27.68, 18.08, and 13.08 at 2 weeks, 4 weeks, 8 weeks, and 12 weeks respectively.
The mean SPADI score in the IAS group was 55.56 (SD 13.169) in the pretreatment phase. This improved to 48.00, 41.28, 30.88, and 27.88 at 2 weeks, 4 weeks, 8 weeks, and 12 weeks respectively.
The mean SPADI score in the SSNB group was 57.28 (SD 17.353) in the pretreatment phase. This improved to 28.04, 21.58, 14.83, and 11.48 at 2 weeks, 4 weeks, 8 weeks, and 12 weeks respectively.
There was a significant difference favoring the SSNB group in the total SPADI score (p-value 0.001, p < 0.05 as significant) and the disability domain of the SPADI scores (p-value of 0.003, p < 0.05 significant). However, there was no significant difference between the two groups in the pain domain of the SPADI score (p-value 0.083, p value < 0.05 as significant).
The trends in the change in Pain, Disability, and SPADI scores are tabulated below (Table 1, Table 2 and Table 3).
Table 1: The trend in pain score over time across the study group. View Table 1
Table 2: Trend in disability score over time across the study group. View Table 2
Table 3: Trend in SPADI score over time across the study group. View Table 3
The average rate of reduction in pain Score in the IAS group was 1.58 per week while that in SSNB group was 1.94 per week (Figure 1). An adjusted mean (95% CI) difference of 3.31 (-0.42 to 7.03) was noted in overall pain scores in favor of SSNB, but the difference was not significant statistically (p = 0.081).
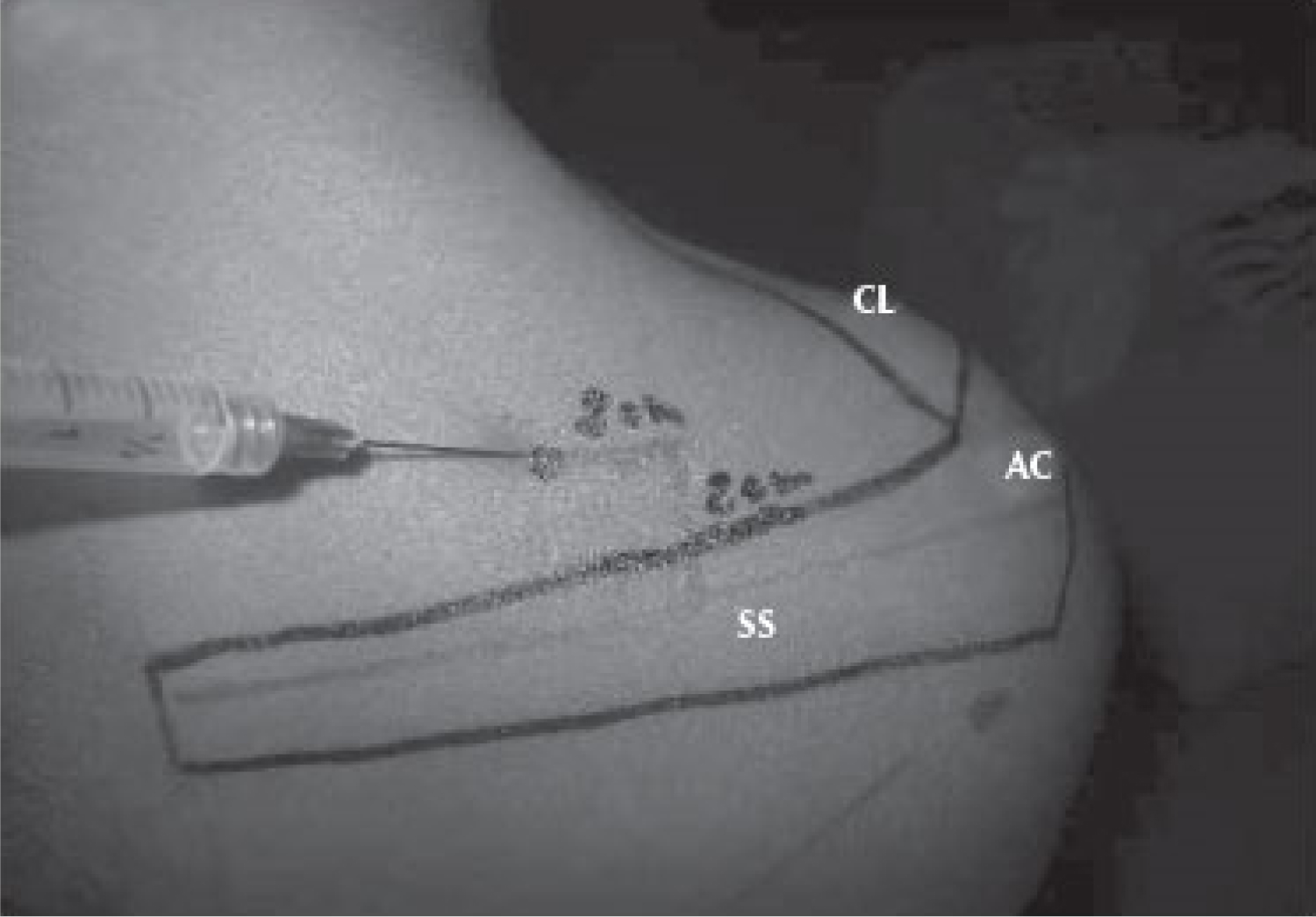 Figure 1: Technique of suprascapular nerve block.
View Figure 1
Figure 1: Technique of suprascapular nerve block.
View Figure 1
Average rate of reduction in Disability Score in IAS group was 3.07 per week while that in SSNB group was 5.07 per week (Figure 2). An adjusted mean (95% CI) difference of 17.91 (6.37 to 29.44) was noted in overall Disability scores in favor of SSNB and the difference was statistically significant (p = 0.003).
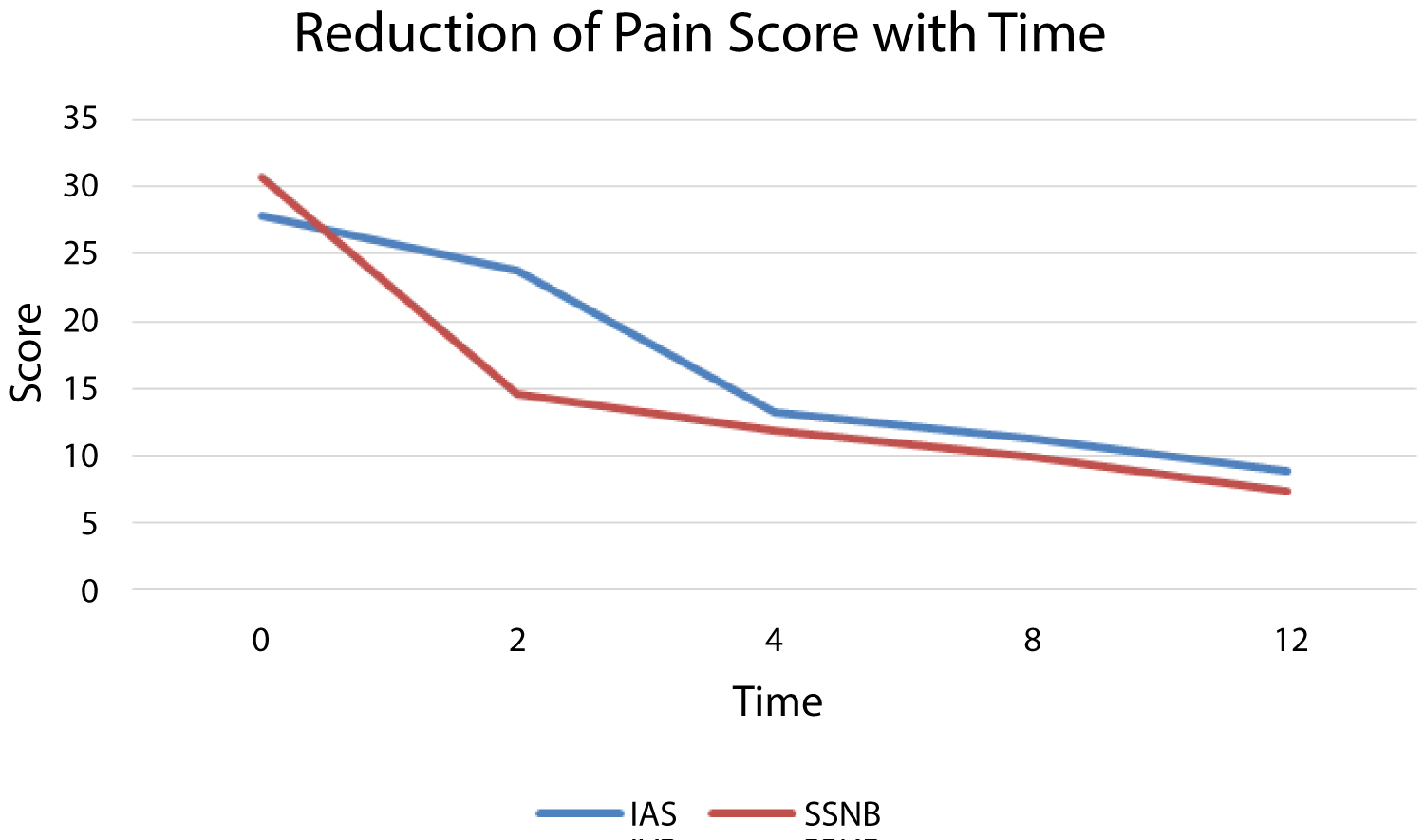 Figure 2: Reduction of pain score with time.
View Figure 2
Figure 2: Reduction of pain score with time.
View Figure 2
The average reduction in SPADI Score in IAS group was 2.31 per week while that in SSNB group was 3.81 per week (Figure 3). An adjusted mean (95% CI) difference of 13.64 (6.03 to 21.25) was noted in overall SPADI scores in favor of SSNB and the difference was statistically significant (p = 0.001) (Figure 4).
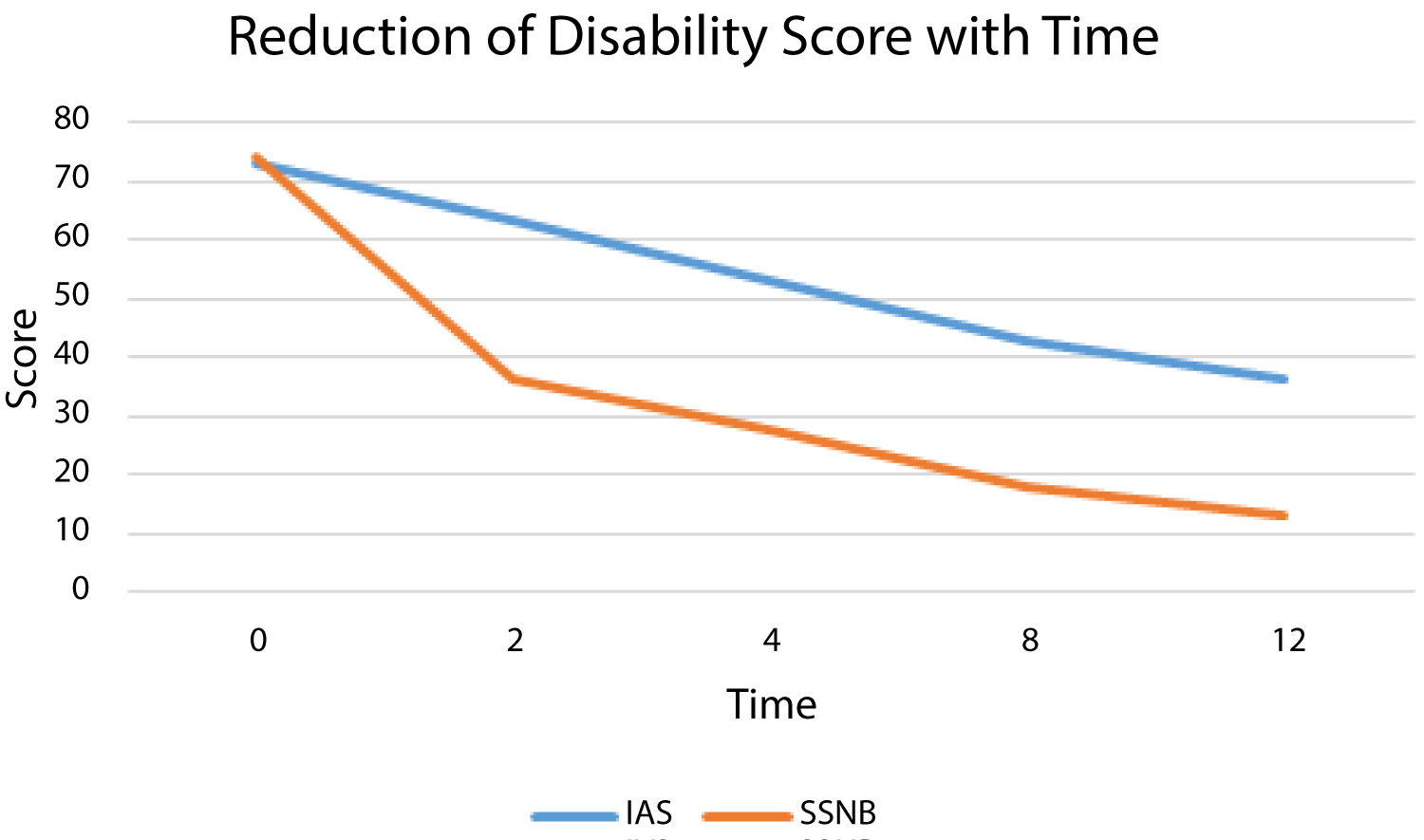 Figure 3: Reduction of disability score with time.
View Figure 3
Figure 3: Reduction of disability score with time.
View Figure 3
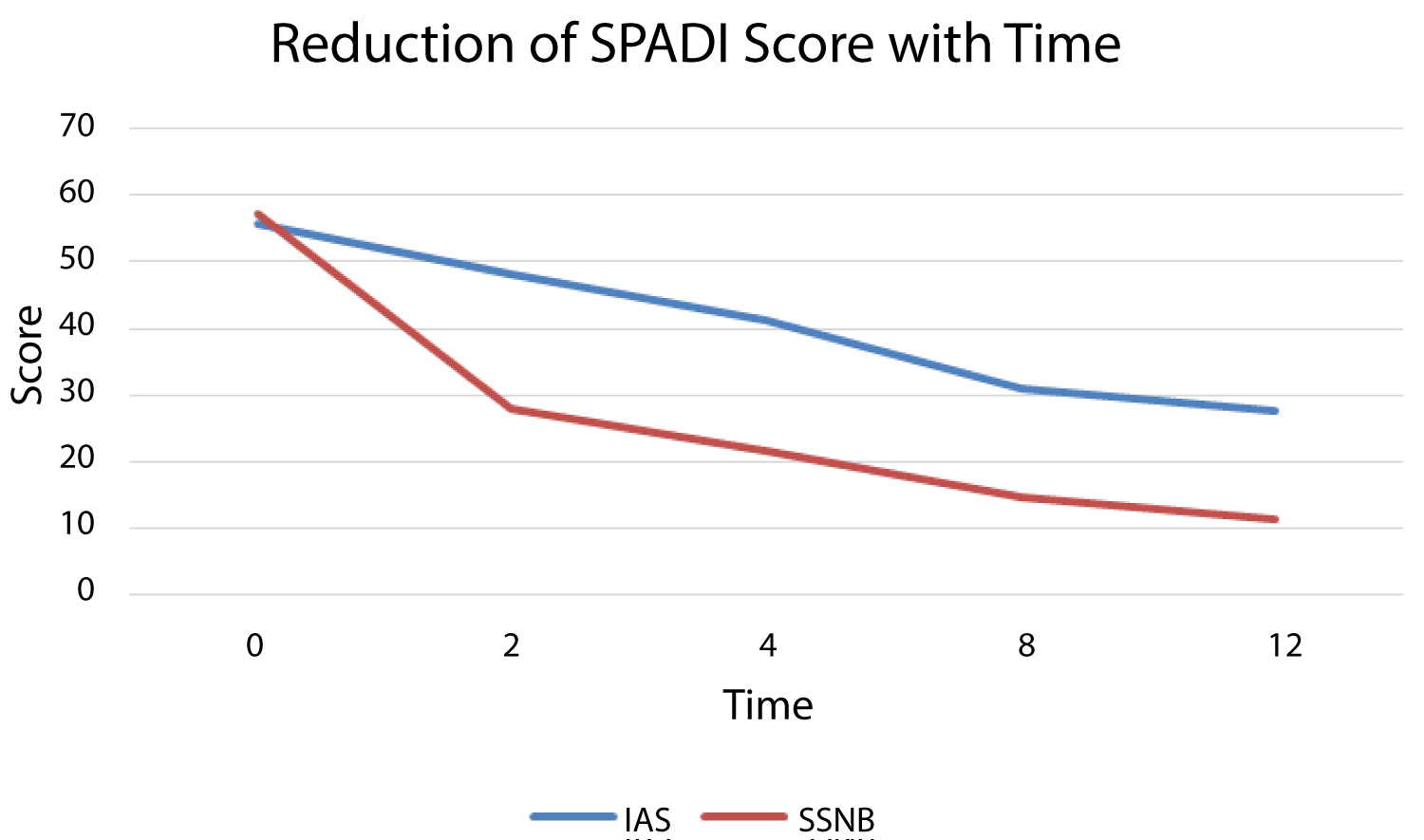 Figure 4: Reduction of SPADI score with time.
View Figure 4
Figure 4: Reduction of SPADI score with time.
View Figure 4
The study did not notice any significant differences in Pain, Disability or SPADI scores across age and gender groups.
Frozen shoulder, a debilitating and painful condition of the shoulder is characterized by soft-tissue contracture of capsulosynovium secondary to inflammation in the joint [8]. Patients in Phase 1 of the frozen shoulder are initially managed by NSAIDS and exercises. However, some patients are refractory to the above line of management and are intolerant to the use of NSAIDs. Refractory cases are managed by various options like intraarticular steroid injection, suprascapular nerve block if they are in Phase 1 of the disease process. But all these modalities will require home-based or supervised exercises of the shoulder. Control of pain is of paramount importance so that patients can cooperate well with the physiotherapy regimen. Both intraarticular steroid injection and suprascapular nerve block aim to control the pain of the patient so that they can perform the capsular stretch exercises. So it is a common practice to administer intraarticular steroid injection or suprascapular nerve block before starting the physical therapy. Our study aimed to find out whether either of the two modalities described above had an advantage over the other. Our study clearly showed that SSNB had a better outcome with respect to SPADI score. Subgroup analysis showed SSNB group had significant improvement in disability compared with IAS group. However, with respect to the pain domain, though SSNB showed better improvement, it was not statistically significant.
Various studies report the use of either of these modalities as an adjunct to physical therapy. Klc, et al. [9] reported on an RCT of 41 patients where they compared a group with physical therapy alone to another group which had suprascapular nerve block before physical therapy. They concluded that suprascapular nerve block is safe and well-tolerated and gives better relief of pain and improvement in function when compared with physical therapy alone. In a meta-analysis of 9 RCTs, Sun, et al. [10] reported that intraarticular steroids before physical therapy improve SPADI score and external rotation range in patients with frozen shoulder compared with physical therapy alone. Lee, et al. [11], Bulgen, et al. [12], have also reported better outcomes with intraarticular steroids. We could not find studies that compared the suprascapular nerve block with intraarticular steroids. Hence we decided to do this study to assess which is better in terms of functional improvement by SPADI score. The suprascapular nerve supplies 70% of the shoulder joint. The suprascapular nerve block was described by Wertheim and Rovenstein [13] in 1941. Ozkan, et al. [14] studied the nerve stimulator guided suprascapular nerve block with 1% lignocaine and methylprednisolone in 10 patients with refractory frozen shoulder and found satisfactory improvement. Use of Ultrasound-guided suprascapular nerve block with 0.5% bupivacaine was compared with intraarticular steroids in 60 patients (thirty in each group) by Sonune, et al. [15]. They found that suprascapular nerve block improved VAS and shoulder Range of Motion much earlier than intraarticular steroids alone. Our study also shows that both intraarticular steroid and suprascapular nerve blocks are effective in improving symptoms of frozen shoulder. But patients who received suprascapular nerve block improved quicker and better as evidenced in our RCT. We used 0.5% ropivacaine which gives longer pain relief and could be the reason for the larger difference in SPADI scores as compared with Sonune, et al. Since the initial pain relief is better and quicker in suprascapular nerve block, patients have better nighttime sleep and cooperate with physiotherapy. We have used only single-shot intraarticular steroid or single-shot suprascapular nerve block but still, consistent improvement is obtained even at 12 weeks. This may be because significant pain relief is obtained in the initial period itself and patients can perform capsular stretches better which may accelerate the healing phase in these patients.
Our study shows that suprascapular nerve block gives faster relief than intraarticular steroids in frozen shoulder.
Our study has its limitations due to its small sample size. We used only clinical assessment for frozen shoulder and no MRI imaging was performed.
A combination of intraarticular steroids with suprascapular nerve block may be better than individual treatments alone and this needs further evaluation. Suprascapular nerve block has the potential of graduating to patient-controlled analgesia technique and this may be used for better compliance while doing physiotherapy [16].
Suprascapular nerve block achieves faster improvement in pain and disability compared with intraarticular steroids in patients with frozen shoulder when used as an adjunct to home-based physical therapy.
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
The authors wish to acknowledge the support of the State Bureau of Medical Research in their help in conducting the study.
The authors acknowledge the help of Dr. Anish TS, Epidemiologist in the statistical assessment of the study.